Fig. 32.1
Intraoperative ultrasound monitoring of flexible ureteroscopy
Lithotripsy
Given the risks entailed and personnel and resources assembled, it is advisable to have appropriate tools for lithotripsy on hand. A stone small enough to allow uncomplicated extraction should be a pleasant surprise as opposed to the expected norm. If a stone is encountered that is too large to safely attempt basket extraction, the ideal lithotripter should have an appropriate tissue safety margin, the flexibility to be delivered via semirigid or flexible ureteroscopes, induce the least peripheral tissue damage, pose the least risk to the fetus, and cause the least reduction in irrigant flow.
Although ultrasonic lithotripters were utilized in one of the earliest reports of ureteroscopy in pregnancy, the authors raised the concern for possible auditory damage to the fetus. No follow-up after birth was available to assess whether fetal hearing had been impaired [31]. Another technology specifically avoided during pregnancy is electrohydraulic lithotripsy, which has been cited to have the narrowest margin of tissue safety, with unproven but queried effects on fetal hearing and uterine contractions [28].
Pneumatic lithotripsy has been successfully employed for intracorporeal lithotripsy during pregnancy. However, it must be used with a semirigid ureteroscope, leaving no option for lithotripsy if flexible scopes are required for navigation to stone or stone fragments. Furthermore, retropulsion of stone fragments is a well-recognized effect of this device and in one series, 27% of pregnant patients had stones pushed back to the renal pelvis and required postpartum SWL [32, 33].
The holmium:YAG laser best meets the demands of the ideal lithotripter in this situation and has emerged as a first line lithotripsy device, with excellent safety profile [28]. The holmium:YAG laser’s small diameter fibers allow passage through flexible scopes with preservation of irrigant flow. It has also been demonstrated to have significantly less retropulsion than pneumatic lithotrites [34].
Stent Placement
After ureteroscopic inspection confirms all ipsilateral stone fragments have been removed, a stent is typically placed. A retrospective review detailing a single institution’s experience in ureteroscopy in seven pregnant women noted that both of the two who did not have stents placed returned postoperatively with severe colic requiring hospitalization of 48 and 72 h. A third whose stent was removed the day of placement also returned with severe colic and premature uterine contractions requiring stent replacement. These authors thus recommended that all pregnant women have stents placed for at least 72 h postoperatively [35].
Over the previously placed safety wire, a stent of appropriate length is passed. Real-time ultrasound confirms the tram-track appearance of the hollow stent in the renal pelvis (Fig. 32.2), and as the wire is withdrawn, the deployed curl is visualized. Direct visualization of the distal curl confirms adequate coil in the bladder.
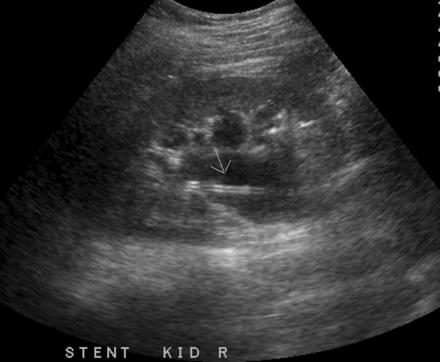
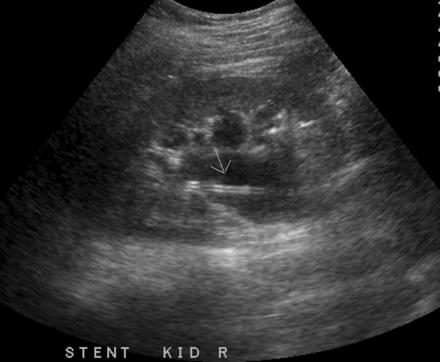
Fig. 32.2
Intraoperative ultrasound appearance of stent within renal collecting system
Note well, care must be taken to ensure timely removal of the stents. Encrusted stents may be encountered. Cystolitholopaxy, ureteroscopic lithotripsy and stent extraction, postpartum PCNL, and ureterolithotomy all may be potentially required to address these encrusted stents [1, 26, 33]. Tethers left attached to the distal curl may be utilized to aid timely removal of the stents in appropriately selected patients.
Complications
With unique anatomic and physiologic characteristics, the pregnant woman is different than the nongravid patient undergoing ureteroscopy. In light of this, a systematic review of the literature and meta-analysis was performed to assess the endoscopic safety of ureteroscopy in pregnancy. The overall complication rate was 8.3%—2 Claiven 1, 6 Claiven 2, and 1 Claiven 3 complications were noted. These were then compared with the complication rates derived from the AUA/EAU ureteral stone guidelines and specifically revealed no statistical difference in the rate of ureteral injury or UTI [36].
In order to better define the risk of obstetric complications, a multicenter retrospective review was performed of 46 ureteroscopies performed during pregnancy [37]. There were two obstetric complications of preterm labor in this series for an incidence of 4.3%. One was managed with tocolytics and the other required cesarean section. There were no pregnancies lost. The reported 4.3% incidence of obstetric complication is no more than that observed in women simply admitted with renal colic during pregnancy. Nonetheless, their occurrence emphasizes the need for a multidisciplinary team prepared to manage preterm labor expediently if it occurs.
Summary
When expectant management fails and temporizing measures are not tolerated or unacceptable, ureteroscopy has been shown to be an effective method for treating stones during pregnancy. Obstetric consultation should be obtained. Fetal heart monitoring, obstetric services, and a neonatal team may be required and thus should be available. If all of the recommended services are available, the experience and expertise of the urologist and anesthesiologist serve as final determinants as to whether it is prudent to proceed or whether transfer to another center should be considered.
Ureteroscopy may be performed as typically described, although intraoperative radiation exposure should be minimized. Techniques to reduce or eliminate this exposure have been outlined and should be utilized. Lithotripsy may be safely performed if required, ideally with holmium:YAG laser. Brief postoperative stenting has been recommended. Endoscopic complications are no more common in the gravid patient, although preterm labor is a complication unique to and observed in this cohort, underscoring the need for the coordination of a team with the necessary expertise to ensure safety of both the mother and child in the intra- and postoperative period.








