(1)
Gastroenterology and hepatology, Chinese PLA General Hospital, Beijing, China, People’s Republic
Abstract
In this chapter we discussed the use of tunnel technique for esophageal achalasia, that is peroral endoscopic myotomy (POEM). The history, indications and procedure of POEM are described first. Then, in addition to the inner circular myotomy and full-thickness myotomy of LES, another two new types of myotomy are introduced. The first is the circular muscle myotomy plus 2 cm-balloon plasty, which is performed in the way that a balloon of 2 cm in diameter was set at the cardia to further dilate the LES right after completion of the myotomy of the inner circular muscle. The second is the glasses style anti-reflux myotomy, which retains about 1 cm of longitudinal muscle at the level of the dentate line after incision of the inner circular muscle, and selective incision of the longitudinal muscle right above and below the dentate line. And the retained 1 cm of longitudinal muscle is expected to achieve a best result to prevent the reflux after POEM. At last we report the effect of Ling classification on complications of POEM.
7.1 History, Indications and Procedure of POEM
7.1.1 History of POEM
During POEM, the most critical technique used is to establish a peroral submucosal tunnel in the esophagus, and the idea of realizing myotomy through a submucosal tunnel has been originated from two mutually independent backgrounds, which namely are endoscopic submucosal dissection (ESD) and natural Orifice transluminal endoscopic surgery (NOTES).
7.1.1.1 Origin from ESD
In 2009, Linghu [1] used tunnel technique to treat a case of esophageal circumferential lesion of 8 cm in length, which was the first time that tunnel technique had been clinically reported. For that long esophageal circumferential lesion, it would have been too difficult to achieve en bloc resection without destruction of the structure of the lesion if traditional ESD without tunnel technique had been used. So, after making circumferential incision along the anal and the oral edge of the lesion, a tunnel was established from the oral incision to the anal incision in the submucosal layer and then making use of the room afforded by the submucosal tunnel, the rest of the lesion was gradually resected as a single piece. The technique used in treating this circumferential lesion was similar to the tunneling method in engineering technology and thus it was named tunnel technique. Linghu et al. [2] subsequently reported application of tunnel technique in treating circumferential early esophageal cancer and non-circumferential large esophageal lesions, which made the conception of tunnel technique more widely accepted. In the following years, other diseases from mucosa, muscularis propria and even diseases outside of the esophageal lumen were reported to be treated by tunnel technique, and POEM was a typical use of tunnel technique to treat diseases from muscularis propria [3].
7.1.1.2 Origin from NOTES
To explore the possibility of performing peroral myotomy for treatment of esophageal achalasia, Ortega et al. [4] reported as early as in 1980 that a modified needle knife was used to directly incise the muscularis propria through the mucosal layer by endoscopy without establishing a submucosal tunnel, the disadvantage of which was that myotomy was performed blindly and thus perforation and damage of adjacent tissues could not be avoided with certainty. Considering its above mentioned disadvantages, that kind of blind myotomy was not repeated by others for many years. In 2004, Kalloo et al. [5] first put forward the idea of incisionless NOTES, the core of which was that using a flexible endoscope to access the abdominal cavity, retroperitoneum, thoracic cavity to perform surgery without incisions on the surface of the body through a natural orifice of the body, such as the esophagus, the stomach, the intestine or the vagina. In 2007, Pasricha et al. [6] reported that myotomy of the esophageal muscularis propria was successfully performed by establishing a submucosal tunnel in a porcine model, and they reported that average LESP (Lower esophageal sphincter pressure, LESP) was reduced from the pre-myotomy 16.4 mmHg to the post-myotomy 6.7 mmHg. Then, there was a report [7] in 2008 that cholecystectomy was successfully performed through the stomach. In 2010, Inoue et al. [8] first reported the results of 17 patients with achalasia treated by POEM and the short-term outcomes were satisfactory with the average LESP of patients reduced from the pre-POEM 52.4 mmHg to the post-POEM 19.9 mmHg, and the term POEM was also coined by Inoue H then.
The two different origins of tunnel technique finally led to the same destination that esophageal achalasia was treated by peroral myotomy making use of the establishment of a submucosal tunnel. Tunnel establishment and myotomy are the two core steps of POEM, and the two origins of POEM are fundamentally different considering the timing of the combination of the two steps of POEM. In the history of origin from ESD, tunnel establishment was first used to treat long esophageal circumferential lesions that were difficult for traditional ESD to achieve en bloc resection, and then indications of tunnel technique was extrapolated to myotomy for achalasia. While in the history of origin from NOTES, direct endoscopic myotomy was first attempted by natural orifice and then to minimize the risk of complications like perforation and to better control the depth of incision, tunnel establishment was introduced into the procedure of endoscopic myotomy.
7.1.2 Indications of POEM
It has been reported that the success rate of POEM for esophageal achalasia 90.9–100 % [8–12]. Yet, it is still inconclusive currently on all the indications of POEM. Whether all the patients diagnosed with esophageal achalasia could be treated by POEM still warrants further researches.
Inoue et al. [8] reported that for endoscopists in their early-stage practice of POEM, the patients with obvious esophageal distortion should not be included, while for experienced endoscopists in performing POEM, the inclusion criteria could be extended to all the patients with esophageal achalasia, including patients with previous history of POEM or Heller myotomy.
To investigate the indications of POEM, Linghu et al. [13, 14] analyzed the endoscopic pictures of nearly 1,000 patients with achalasia and proposed the Ling classification for selection of appropriate candidates for POEM. The Ling classification divided the patients into three types according to the middle and lower esophageal morphology. And they suggested that type Ling I and IIa are indicated for POEM with safety and that Ling IIc and Ling III are indicated for POEM only when the crescent like structure or the diverticular structure are not in the rout of tunnel establishment.
Though POEM was initially used to treat the primary esophageal achalasia, the indications of POEM are not just limited to esophageal achalasia by now. It has been reported that other esophageal motility disorders such as diffuse esophageal spasm [15], distal esophageal spasm [16] and nutcracker esophagus [10] could successfully be treated by POEM.
7.1.3 Procedure of POEM
7.1.3.1 Patient Management Before and After POEM
We routinely use the following preoperative and postoperative guidelines to treat the patients of esophageal achalasia by POEM (Table 7.1).
Table 7.1
Patient management before and after POEM
Routine checks | Preparations before POEM | Treatment after POEM | Follow up after POEM |
|---|---|---|---|
Endoscopy Esophagography Esophageal manometry 24 h pH monitoring CT (if necessary) Eckardt score | Fast for 48 h with drinking water allowed Antibiotics started before surgery for 3 day Endoscopy before anesthesia to ensure no food residues in the esophagus and stomach | Fluoroscopy for gas-related complications Fast for 3 days and then liquid and semi-liquid food | Endoscopy Esophageal manometry Esophagography 24 h pH monitoring (if necessary) Eckardt score |
Eckardt score is a commonly used scale as an evaluation of symptoms of patients with esophageal achalasia and was described in Table 7.2.
Table 7.2
Eckardt score
Score value | Weight loss (kg) | Dysphagia | Posterior sternal pain | Reflux |
|---|---|---|---|---|
0 | None | None | None | None |
1 | <5 | Occasionally | Occasionally | Occasionally |
2 | 5–10 | Each day | Each day | Each day |
3 | >10 | Each meal | Each meal | Each meal |
7.1.3.2 Procedure of POEM
During POEM, patients are in the left lateral position, or the supine position with the right shoulder elevated. ECG, blood pressure and oxygen saturation are monitored, and CO2 gas insufflation should be used. The procedure of POEM steps can be generally divided into four steps (Fig. 7.1), including entry incision, establishment of the tunnel, myotomy and sealing of the entry incision.
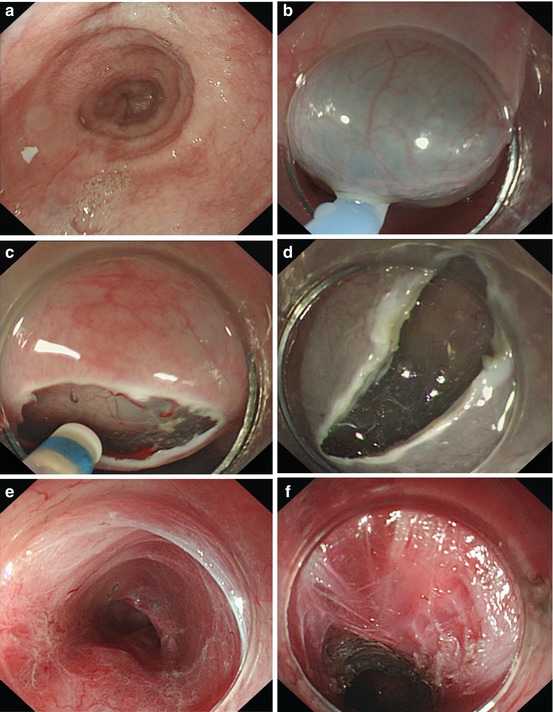
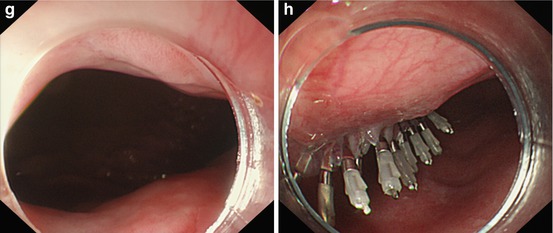
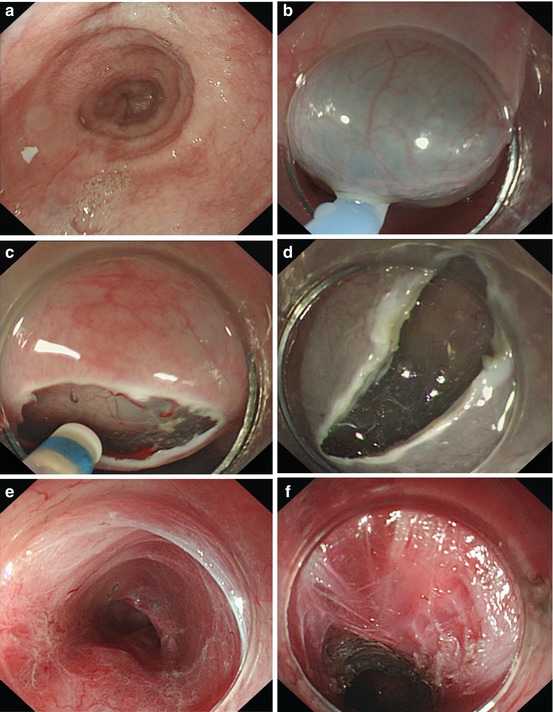
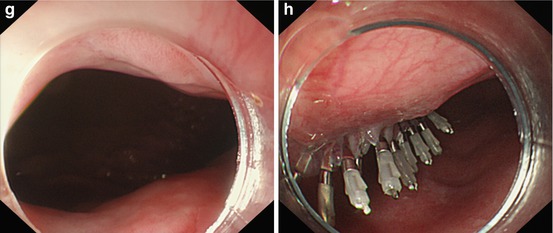
Fig. 7.1
The procedure of POEM. (a) The cardia is tightly closed before POEM. (b) Submucosal injection in mid-esophagus. (c) Transverse entry incision. (d) Longitudinal entry incision. (e) Submucosal tunnel established till 3 cm below GEJ. (f) Inner circular muscle incised. (g) The cardia becomes relaxed after POEM. (h) The well sealed entry incision
7.1.3.3 Key Points of Myotomy of the Muscularis Propria
Myotomy of the muscularis propria is a critical step during the procedure of POEM, and below discussed are the technical key points of myotomy of the inner circular muscle, and those of myotomy of the full thickness of muscularis propria.
Myotomy of the Inner Circular Muscle
1.
Location of muscularis propria in the tunnel
When the submucosal tunnel is established at the 12 o’clock position, the muscularis propria is located in the upper half of the tunnel (Fig. 7.2a, b);when the submucosal tunnel is established at the 6 o’clock position, the muscularis propria is located in the lower half of the tunnel (Fig. 7.2c, d). To determine the location of muscularis propria from within the tunnel, two key anatomic marker should be recognized. The first is the blood vessels that are on the side wall of the mucosa when the depth of the submucosal tunnel is to SM2-SM3, but may be on the side of muscularis propria when the depth of the submucosal tunnel is not deeper than SM1, and the second is the circular muscle fibers which is the most accurate marker of the muscularis propria.
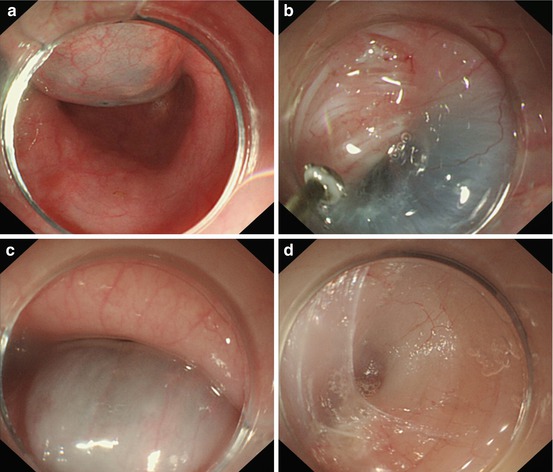
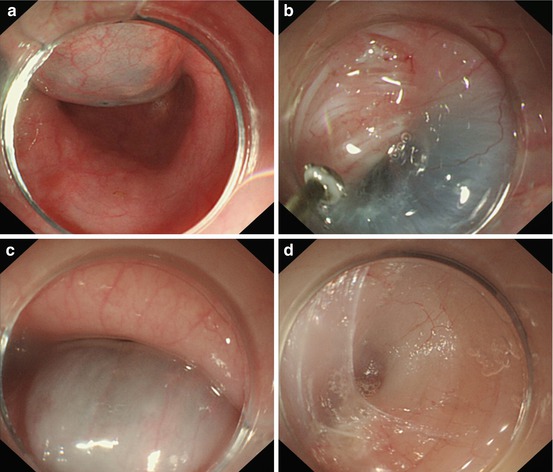
Fig. 7.2
(a) Twelve o’clock submucosal injection for entry incision. (b) The muscularis propria is located in the upper half of the tunnel. (c) Six o’clock submucosal injection for entry incision. (d) The muscularis propria is located in the lower half of the tunnel
2.
Electro surgical knives
Endoscopic electro surgical knives, such as TT knife, hook knife, hybrid T knife or Dual knife, could be chosen to perform myotomy according to the preference of the operators.
3.
Output power
Generally used for myotomy is the hybrid coagulation out power but not the forced coagulation.
4.
Start point
The start point of myotomy is recommended at the oral edge of the narrow position of the muscularis propria observed from within the tunnel (Fig. 7.3a).
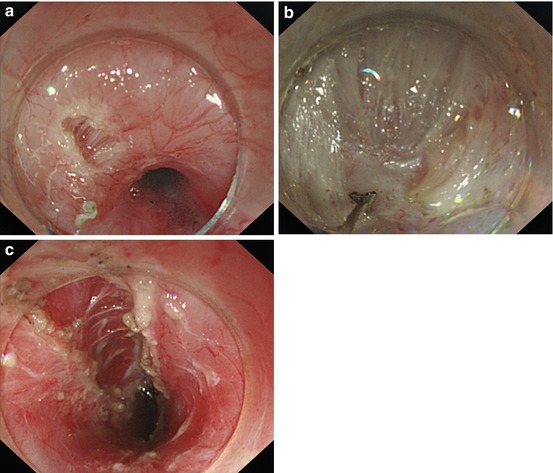
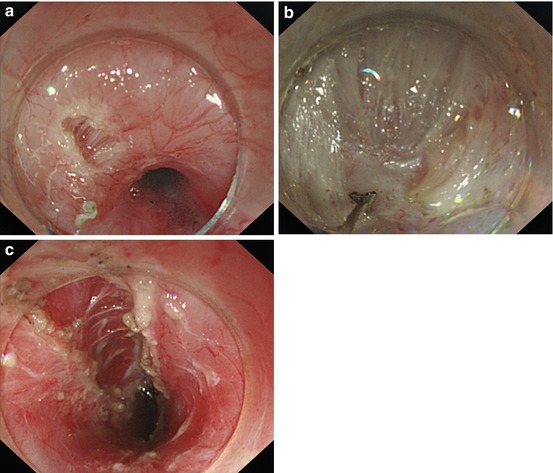
Fig. 7.3
(a) The start point of myotomy is recommended at the oral edge of the narrow position of the muscularis propria. (b) Myotomy is gradually performed from the oral side to the anal side. (c) The end point of myotomy is at 2 cm below the GEJ
6.
End point
The end point of myotomy is at 2 cm below the GEJ (gastroesophageal junction) (Fig. 7.3c).
7.
Myotomy
Take the TT Knife (triangular tip knife) as an example to introduce the technique of myotomy of inner circular muscularis propria: First gently attach the TT knife to the muscularis propria and gently step upon the pedal to cut open and expose part of the circular muscular layer (Fig. 7.4a). Then continue to perform myotomy of the inner circular muscular layer with the TT knife incising forward closely along the longitudinal muscular layer (Fig. 7.4b). Till myotomy performed to the cardia where muscularis propria has 3 layers of muscle, the inner two layers of muscle will be incised with the outmost longitudinal layer of muscle left intact (Fig. 7.4c). When the hybrid T knife is used (Fig. 7.4a), it could be inserted directly between the circular and the longitudinal muscular layer at 6 o’clock to perform myotomy of the inner circular muscle(Fig. 7.4b). The endoscope could also be pulled backward to finish the myotomy of the residual circular muscle to best achieve complete myotomy of the inner circular muscle.
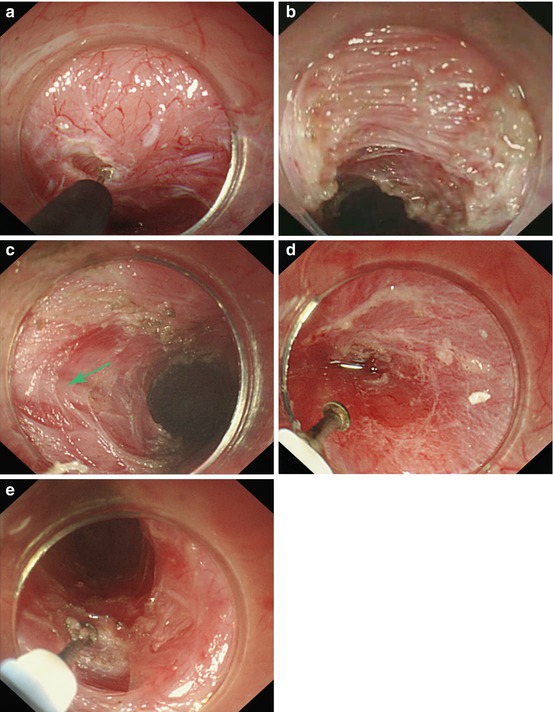
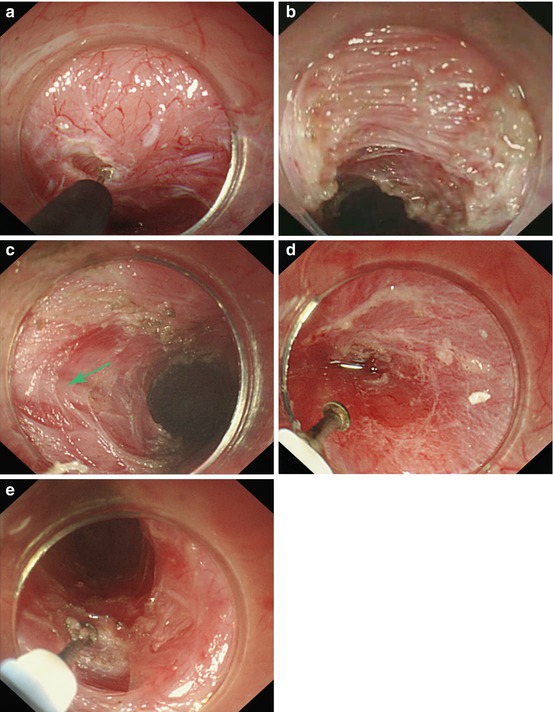
Fig. 7.4
(a) Part of the circular muscular layer is exposed. (b) Part of circular muscle has been incised. (c) The outmost longitudinal layer of muscle left intact (arrow). (d) The tunnel has been established using the hybrid T knife. (e) The hybrid T knife is inserted between the circular and the longitudinal muscular layer at 6 o’clock to perform myotomy
8.
Hemostasis
When seeing the vessels located along with the circular muscular fibers (Fig. 7.5a), try to avoid incising the vessels. But if blood is oozing from the cutting edge of the circular muscle, coagulation should be promptly performed to stop the bleeding with the endoscopic electro surgical knife (Fig. 7.5b); if the bleeding is as acute as gushing that could not be stopped by the knife (Fig. 7.5c), enough water should be injected to wash the bleeding site to clearly distinguish the bleeding vessel and use the hemostatic forceps to clip and coagulate it (Fig. 7.5d, e).
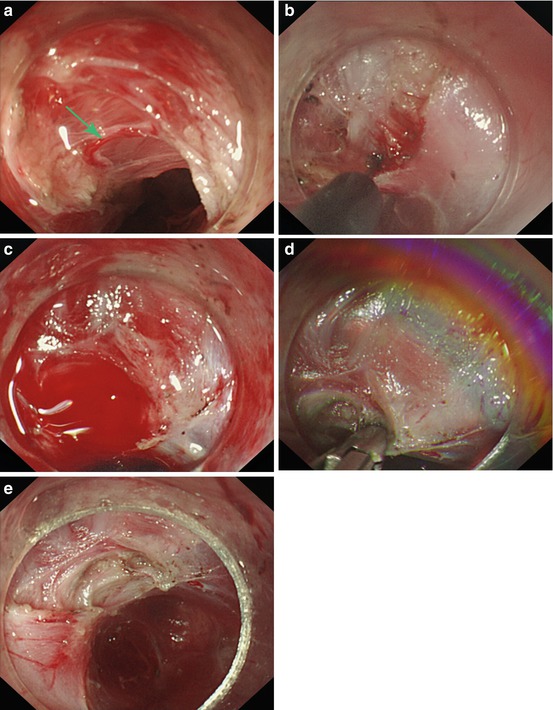
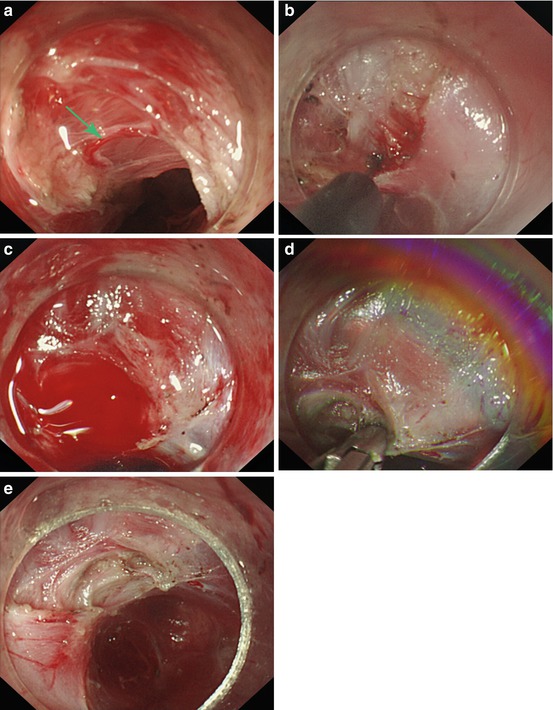
Fig. 7.5
(a) Vessels located along with the circular muscular fibers (arrow). (b) Coagulation should be promptly performed to stop the bleeding. (c) The bleeding is as acute as gushing. (d) Distinguish the bleeding vessel and use the hemostatic forceps to clip it. (e) The bleeding vessel is coagulated by the hemostatic forceps
9.
Length of myotomy
The length of myotomy ranges in our experience from 3 to 7 cm. After myotomy of the circular muscle, the endoscope should be pulled back into the esophageal lumen to observe if the cardia has become more relaxed than before myotomy (Fig. 7.6). If the cardia is still as tight as before myotomy, myotomy should be extend to longer inner circular muscle.


Fig. 7.6
The cardia becomes more relaxed after myotomy
Full Thickness Myotomy of Muscularis Propria
The full thickness myotomy of muscularis propria is usually performed below the cardia (Fig. 7.7) and is more easy to perform compared with the myotomy of inner circular layer of muscularis propria. The myotomy could be performed either from the anal to the oral side or from the oral to the anal side, but be sure not to damage the large vessels adjacent to the outer layer of the muscularis propria at below the cardia.
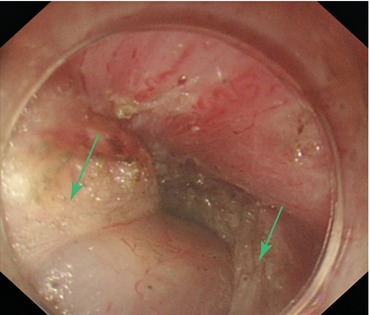
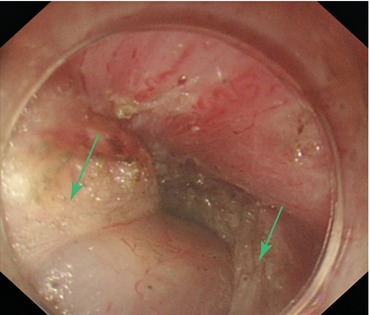
Fig. 7.7
Full thickness myotomy of muscularis propria below the cardia (the arrows denote the incised muscle fibers)
7.1.3.4 Efficacy Evaluation of POEM
Efficacy of POEM can be evaluate by symptoms, esophageal manometry, esophagography, 24 h pH monitoring and endoscopy.
Symptoms
The symptoms quickly resolve in patients after POEM with a symptom remission rate of 93.4–100 %. These results are from the short term follow-up studies, while the long-term efficacy remains to be further clarified. The definition of symptom remission of Eckardt score is no more than 3.
Esophageal Manometry
LESP was significantly lower after POEM (Fig. 7.8), which indicates that the myotomy of muscularis porpria achieves a successful incision of the LES.
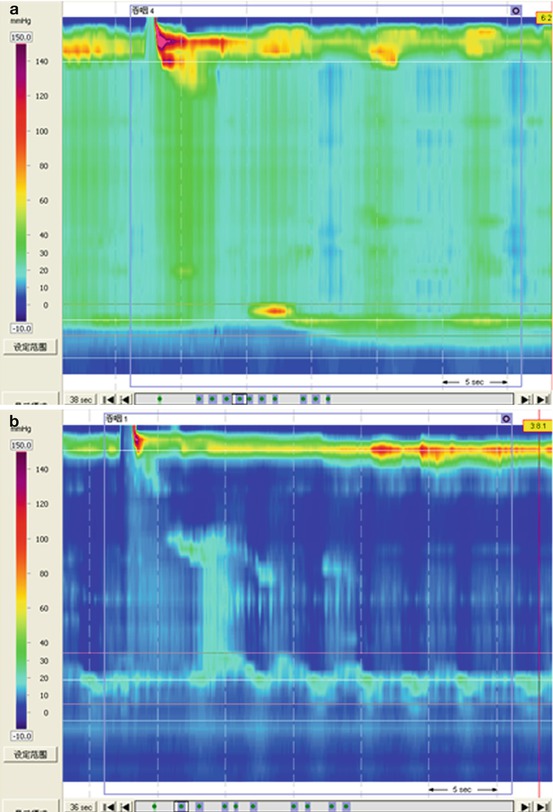
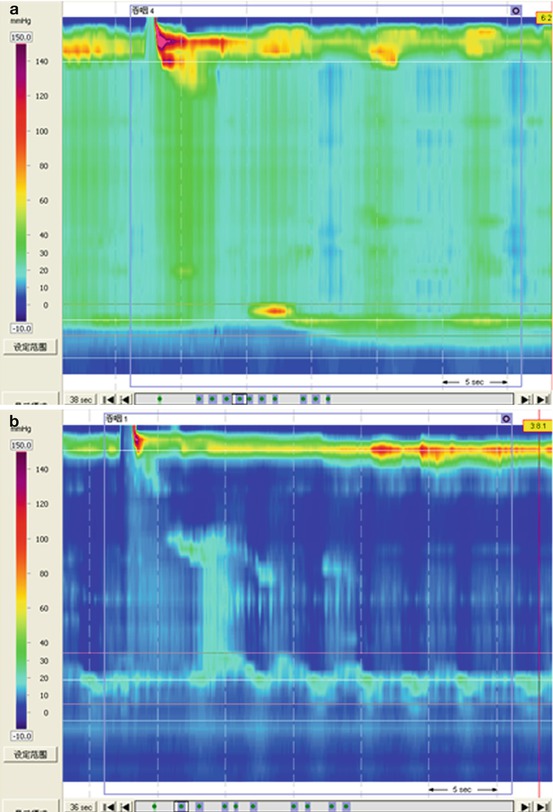
Fig. 7.8
(a) LESP can be seen significantly higher before POEM. (b) LESP decreased to normal after POEM
Esophagography
The width of the esophagus dropped in most patients after POEM, which indicates the relaxation of the LES (Fig. 7.9).
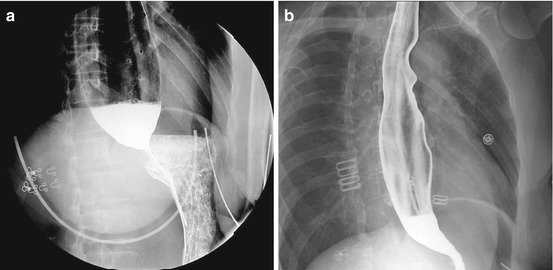
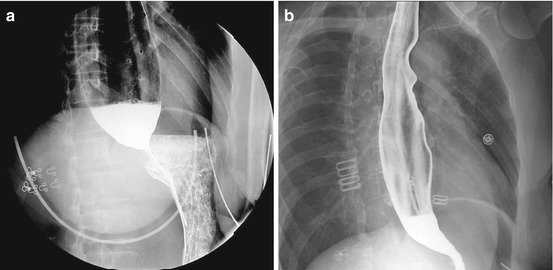
Fig. 7.9
(a) Dilated esophagus before POEM. (b) Dilation relieved after POEM
24 Hours pH Monitoring
Reflux esophagitis and non-erosive reflux disease (NERD) are reported after POEM and 24 h pH monitoring is recommended for post-POEM patients with symptoms of heartburn and regurgitation but without endoscopic esophagitis.
Endoscopy
Relaxation of LES could be judged by the relieved resistance of maneuvering the endoscope after POEM. Endoscopy is routinely performed within 1 month after POEM to determine the healing of the entry incision.
Randomize Controlled Study
We conducted a randomized controlled study comparing BTI, BD and POEM for treatment of esophageal achalasia (DDW) and will now introduce it as follows.
BTI, BD and Heller myotomy (HM) are the three commonly used treatments for achalasia. BTI was confirmed to have a lower symptom remission rate than BD and HM [17–19]. However, many patients would prefer to choose BTI as their first-line treatment because of its less invasiveness, better endurance, lower complication rate and shorter recovery time compared with BD and HM. And in addition, BD or HM could be a rescue therapy once TBI failed. Randomized studies comparing efficacy between BD and HM had different results. Boeckxstaens et al. reported that therapeutic success rates in BD and HM were 93 % VS. 90 % 1 year after treatment and 90 % VS. 86 % 2 years after treatment, and no significant difference was observed between them [20]. On the contrary, Kostic et al. reported that efficacy of HM was superior to BD because HM had higher therapeutic success rates than BD (77 % VS. 96 %) when studied 1 year after treatment [21]. So, whether HM was superior to BD still remains controversial.
In 2010, POEM was first introduced to clinical use by Inoue et al. [8] and by now has been reported to have satisfactory short term efficacy by several other studies from different countries [9–12]. However, complications of POEM like mucosal perforation, pneumothorax, pneumoperitoneum et al. were not uncommon [8–12, 22, 23]. Even seemed as a promising treatment, role of POEM in treatment for achalasia still needs to be eventually determined by randomized studies and yet no randomized studies have been reported. So, we compared efficacy and safety among POEM, BTI and BD in a randomized manner in this study.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








