(1)
Gastroenterology and hepatology, Chinese PLA General Hospital, Beijing, China, People’s Republic
Abstract
The tunnel technique develops rapidly, and promising results have been shown in clinical studies and animal experiments. In this technique, one submucosal tunnel is created to provide working space for further endoscopic interventions, such as cutting the muscularis propria in the treatment of achalasia, removing gastrointestinal submucosal tumors, or even allowing access to the peritoneal and thoracic cavity for further interventions. Since 2009, Professor Enqiang Linghu has attempted to improve ESD procedure by use of tunnel technique, and thus one submucosal tunnel extending from oral margin to anal margin is established to facilitate en bloc resection of the lesions. Tunnel technique has been used to treat esophageal circumferential lesions, large esophageal lesions and gastric large lesions, and proved to be safe and effective, which will be discussed in detail in this chapter. Tunnel technique changes the standard procedure of ESD from marking–injection–circumferential incision–dissection to marking–injection–anal incision–oral incision–tunnel creation–bilateral resection.
The detection rate of superficial gastrointestinal neoplasms, including precancerous lesions and early cancer, increases with the popularity of endoscopic examination and development of endoscopic technique. Meantime, endoscopic submucosal dissection (ESD) has been recognized as one standard and minimally-invasive treatment for en bloc resection of gastrointestinal neoplasms [1, 2]. However,two problems would occur fro the dissection of large lesions using the standard procedure ESD, one of which is that the lifting effects of submucosal injection is quite different before and after circumferential incision and more specifically is less obvious after circumferential incision, the other of which is that when the dissection reaches the central part of a large lesion, the endoscopic vision is obscured because the space for maneuvering the endoscope becomes confined mainly due to the contraction of the dissected part of the lesion [3, 4]. These problems make further dissection difficult, unsafe and time-consuming. To overcome these difficulties, modified fishing-line traction system (Fig. 6.1) and “medical ring” (Fig. 6.2) have been devised in ESD procedure for resection of large esophageal tumors and early gastric cancer respectively [5, 6]. In the procedure of resecting large lesions, these methods can avoid the obstruction of endoscopic view from resected mucosa, but they cannot be applied easily or conveniently.
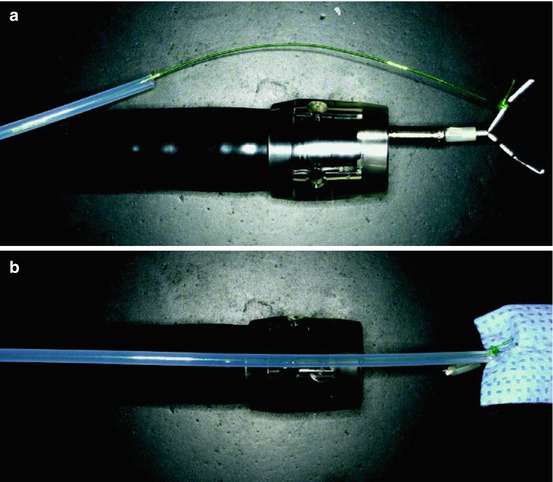
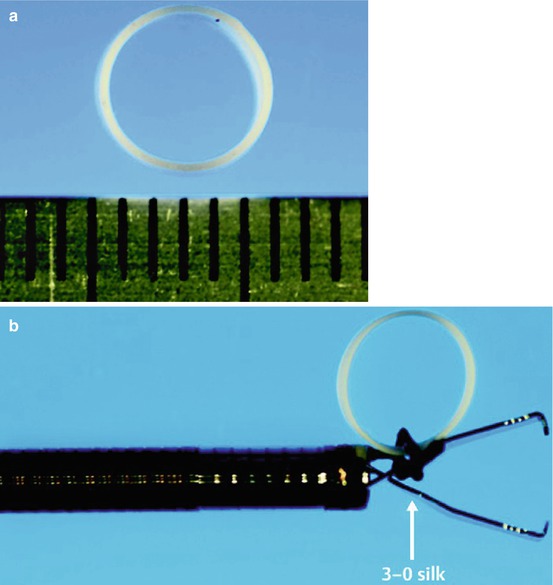
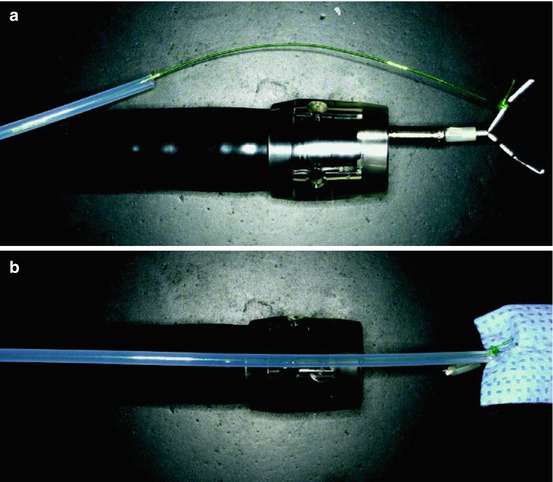
Fig. 6.1
Fish-line traction system (a) Fishing line tied to the endoclip. (b) A plastic sheath is inserted along the fishing line after placement of the endoclip (Reproduced with permission from Tsao et al. [5])
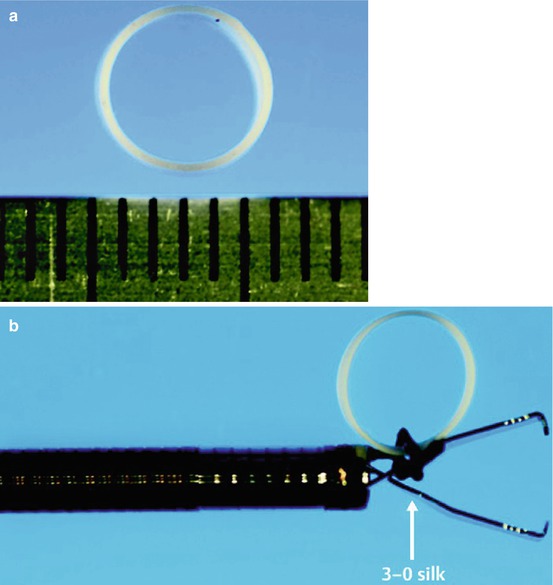
Fig. 6.2
“Medical ring” (a) The “medical ring” has a diameter of 6 mm with width of 2 mm and thickness 200 µm, and is white to ensure the highest level of visibility. (b) For mounting, the ring is attached to a hemoclip with 3-0 silk. (Reproduced with permission from Matsumoto et al. [6])
The tunnel technique develops rapidly, and promising results have been shown in clinical studies and animal experiments [7–16]. In this technique, one submucosal tunnel is created to provide working space for further endoscopic interventions, such as cutting the muscularis propria in the treatment of achalasia, removing gastrointestinal submucosal tumors, or even allowing access to the peritoneal and thoracic cavity for further interventions. Since 2009, Professor Enqiang Linghu has attempted to improve ESD procedure by use of tunnel technique [7, 8], namely endoscopic submucosal tunnel dissection (ESTD). In ESTD procedure, one submucosal tunnel extending from oral margin to anal margin is established to facilitate en bloc resection of the lesions. ESTD has been applied in esophageal circumferential lesions, large esophageal lesions and gastric large lesions, and proved to be safe and effective [3, 4, 8, 9].
The procedure of the standard ESD includes marking, injection, circumferential incision and dissection, while the procedure of ESTD is different and includes marking, injection, anal incision, oral incision, tunnel establishment and bilateral resection [3, 4].
During ESTD procedure, the anal incision is made before the tunnel creation. The anal incision can serve as the endpoint of the tunnel so that the submucosa will not be dissected immoderately. In addition, the anal incision can prevent abundant gas from over accumulation during the creation of the tunnel, which might result in extra mucosal separation [3, 4].
The following points may explain the advantages of ESTD [3, 4]: (i) The transparent cap attached to the endoscope has an effect of blunt dissection with the moving forward of the endoscope; (ii) The use of CO2 as the insufflation gas during ESTD also has an effect of blunt dissection and could work as a gas cushion since the CO2 increases the distance between the mucosa and the muscularis propria. (iii) Since the dissection is conducted during a tunnel, the submucosally injected solutions are well maintained in the submucosal layer and thus minimizing the amount of injection solutions and increasing the efficiency and safety of dissection. (iv) During submucosal dissection in the tunnel, the traction of the two sides of the tunnel avoids the effects of contraction and obstruction of resected mucosa, and contributes to keeping clear operative view and dissecting the submucosal layer. (v) In the procedure, blood vessels expose well and can be preventive coagulation, which reduces the incidence of bleeding and the time of hemostasis. Therefore, the operative view is clear and the speed of the operation improves accordingly.
The ESTD procedure in different locations described as following.
6.1 ESTD in Superficial Esophageal Neoplasms
6.1.1 Definition
The superficial esophageal neoplasms mainly include early cancer and precancerous lesions in the esophagus. Early esophageal cancers are defined as esophageal cancer with invasion limited into mucosa or submucosa and without lymphatic metastasis. Large ones refer to those more than 2 cm in length and with a circumferential extent of more than one third of the esophageal circumference, but not circular.
6.1.2 Indications
(i) Large superficial esophageal neoplasms; (ii) Circular superficial esophageal neoplasms with length more than 2 cm. In addition, the superficial esophageal neoplasms meet at least one of the following requirements: (i) Preoperative biopsy demonstrates high-grade intraepithelial neoplasia or early cancer; (ii) Preoperative biopsy demonstrates low-grade intraepithelial neoplasia without disappearing on the repeat follow-up; (iii) The endoscopy and pathology demonstrate Barrett esophagus, flat polyps or heterotopic gastric mucosa and the patients request endoscopic treatment; (iv) Preoperative biopsy doesn’t demonstrate high-grade intraepithelial neoplasia or early cancer, but iodine staining combined magnified NBI highly indicates high-grade intraepithelial neoplasia and early cancer.
6.1.3 Contraindications
(i)
EUS examination demonstrates the depth of the lesion exceeded the submucosa.
(ii)
EUS, CT or PET-CT demonstrates the lesion with lymphatic or distant metastasis.
(iii)
Advanced cancer or undifferentiated tumor.
(iv)
For those patients with contraindications to gastroscopy or anesthesia.
6.1.4 Preoperative Preparation
Endoscopic equipment and accessories: Single-accessory channel endoscope(GIF-Q260J; Olympus), NBI-magnifying endoscope( GIF-FQ260Z; Olympus), transparent cap (D-201-11804; Olympus),high-frequency generator (ICC-200; ERBE), an argon plasma coagulation unit (APC 300; ERBE), injection needle (INJ1-A1; Medwork), Dual knife (KD-650Q; Olympus), Insulated-tip (IT) knife (KD-611 L; Olympus), Hook knife (KD-620LR; Olympus), and hemostatic forceps (FD-410LR; Olympus); Hybrid knife (ERBE). Carbon dioxide insufflation was used during the procedure. Submucosal injection solution is normal saline with 0.1 % methylene blue and 0.5 % epinephrine. Compound iodine solution is used to spray for observation.
Patient Preparation: First take supine position with head back for tracheal intubation. Then change to left lateral position and undergo general anesthesia.
Preoperative Evaluation of the Lesion: The lesion is observed under light endoscopy combined with magnified-NBI and chromoendoscopy with iodine staining. Then the lesion is evaluated preliminarily and the area of the lesion is determined.
6.1.5 Esophageal ESTD Procedures (Figs. 6.3 and 6.4)
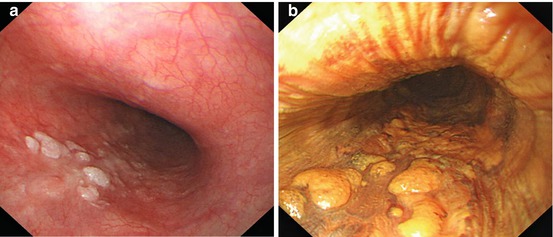
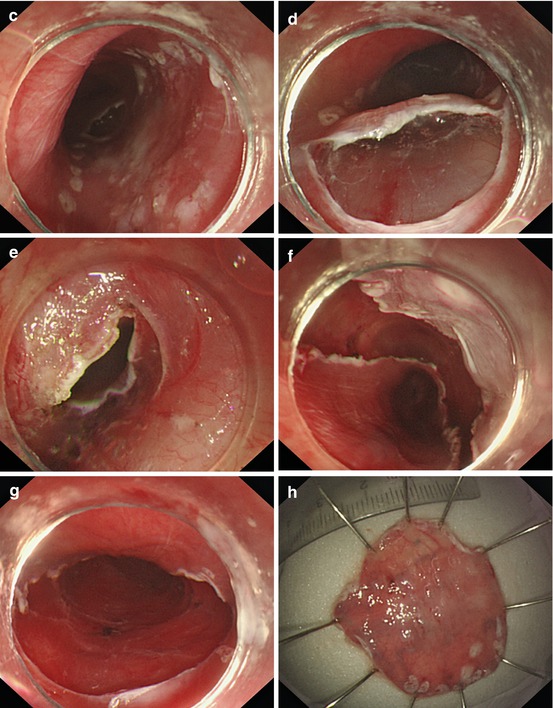
Fig. 6.3




ESTD for large esophageal neoplasms. (a) Observe under light endoscopy. (b) Observe under chromoendoscopy with iodine. (c) Anal incision after marking the margin of the lesion. (d) Oral incision. (e) Submucosal dissection from oral incision to anal incision to create one submucosal tunnel. (f) Bilateral resection. (g) The artificial ulcer after en-bloc resection of the lesion. (h) The resected specimen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








