Truncal Vagotomy with Antrectomy and Billroth II Reconstruction
Michael W. Mulholland
Truncal vagotomy and antrectomy is usually performed in the treatment of complications of peptic ulcer disease. Indications include perforation, hemorrhage, and obstruction. The elucidation of the pathogenic role of Helicobacter pylori in the development of peptic ulceration has decreased the need for operative treatment of peptic ulceration. In addition, the wide availability of proton pump inhibitors and histamine-2 receptor blockers has further diminished the need for truncal vagotomy, an operation designed to permanently suppress gastric acid production.
When truncal vagotomy and antrectomy is used, the first goal is safety from immediate surgical complications and avoidance of long-term undesirable side effects. The second goal is repair of associated anatomic defects, such as pyloric obstruction.
Preparation for elective antrectomy should seek to optimize physiologic status. Electrolyte imbalances, common with gastric outlet obstruction, should be corrected. Retained food and particulate matter may also accumulate within an obstructed stomach. These materials can cause bacterial overgrowth and should be evacuated preoperatively. Scrupulous attention to general nutrition, anemia, and associated comorbid conditions is also required preoperatively.
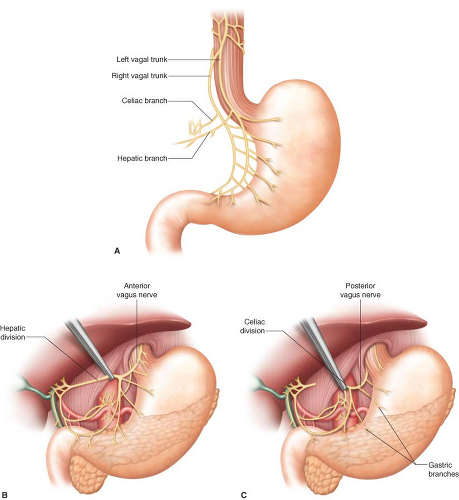
Vagal Anatomy
The vagal nerves form a plexus which surrounds the intrathoracic esophagus. The nerve trunks coalesce within the thorax before entering the abdomen through the esophageal
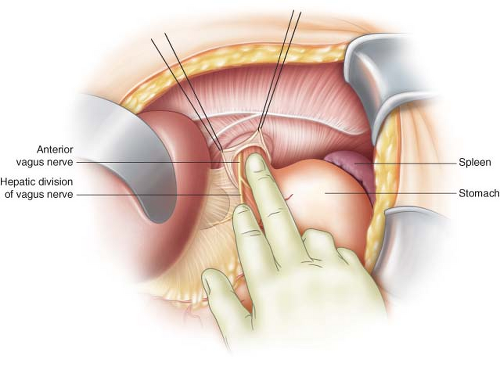
hiatus. The anterior (left) vagus nerve is positioned in immediate contact with anterior wall of the esophagus. The posterior vagal trunk has greater variability but is usually positioned between the posterior-medial wall of the esophagus and the right diaphragmatic crus. The anterior vagus nerve forms a hepatic division which separates from the anterior trunk at the level of the esophageal junction and passes between the avascular leaves of the gastrohepatic ligament. Fibers within the hepatic division innervate the gallbladder, biliary ducts, and liver.
hiatus. The anterior (left) vagus nerve is positioned in immediate contact with anterior wall of the esophagus. The posterior vagal trunk has greater variability but is usually positioned between the posterior-medial wall of the esophagus and the right diaphragmatic crus. The anterior vagus nerve forms a hepatic division which separates from the anterior trunk at the level of the esophageal junction and passes between the avascular leaves of the gastrohepatic ligament. Fibers within the hepatic division innervate the gallbladder, biliary ducts, and liver.
The posterior vagal trunk gives rise to a celiac division which crosses the right diaphragmatic crus in parallel to the left gastric artery. The celiac division is usually
larger than the hepatic division. Branches of the celiac division pass through the celiac ganglion. The anterior and posterior gastric divisions of the vagal trunks parallel the lesser curvature of the stomach and are contained within the gastrohepatic omentum. They run approximately 0.5 to 1 cm from the wall of the stomach along the lesser curvature. Small gastric branches terminate within the gastric fundus, body, and antrum (Fig. 5.1).
larger than the hepatic division. Branches of the celiac division pass through the celiac ganglion. The anterior and posterior gastric divisions of the vagal trunks parallel the lesser curvature of the stomach and are contained within the gastrohepatic omentum. They run approximately 0.5 to 1 cm from the wall of the stomach along the lesser curvature. Small gastric branches terminate within the gastric fundus, body, and antrum (Fig. 5.1).
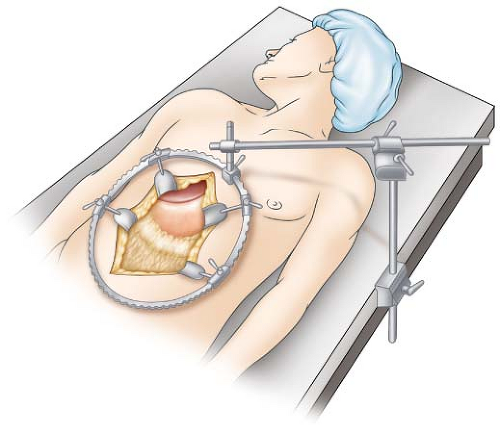
Position
The patient is positioned supine on the operating table. A vertical midline incision extending from the xyphoid inferiorly provides exposure of the upper abdomen for truncal vagotomy performed via laparotomy. Exposure is provided by a self-retaining retractor. The costal margins should be retracted superiorly and elevated. A moderate amount of reverse Trendelenburg position is often helpful in shifting the omentum and other abdominal contents inferiorly and in improving exposure of the upper abdomen (Fig. 5.2).
Truncal Vagotomy
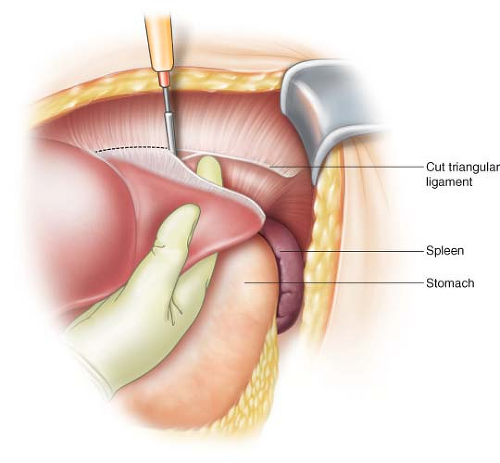
Exposure of the intra-abdominal esophagus can usually be obtained without mobilization of the left lateral segment of the liver. If the left lateral segment of the liver is hypertrophic or enlarged due to fatty infiltration, mobilization of this segment can sometimes improve exposure of the intra-abdominal esophagus. To do this, the surgeon places the right hand under the left lateral segment, palm upward, and retracts the liver inferiorly. The left triangular ligament is often thin and translucent. The fingers of the surgeon’s hands are usually visible through the peritoneum (Fig. 5.3).
The left triangular ligament can be divided without cautery using this exposure. As the line of division proceeds medially, care must be taken to expose the anterior and posterior leaves of the triangular ligament separately. The peritoneal layers and the tissue between them may be divided individually using electrocautery. The inferior phrenic vein is often close to the posterior peritoneal edge of the triangular ligament,
and care must be taken not to injure this vessel. This can be avoided by proper exposure. Mobilization of the left triangular ligament need not extend beyond the midline (Fig. 5.4).
and care must be taken not to injure this vessel. This can be avoided by proper exposure. Mobilization of the left triangular ligament need not extend beyond the midline (Fig. 5.4).
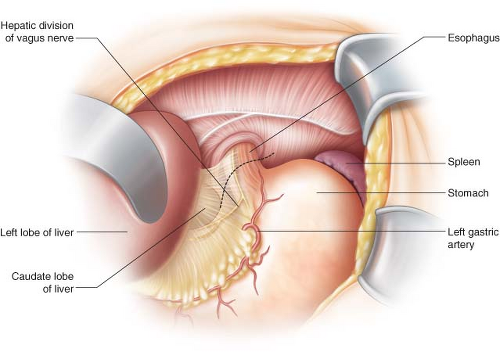
With the left lateral segment of the liver retracted and protected, the anterior surface of the intra-abdominal esophagus can be appreciated visually and also by palpation of a previously placed nasogastric tube. The peritoneum overlying the esophagogastric
junction is divided transversely using electrocautery. In doing so, the hepatic branch of the anterior vagus nerve is sometimes visible in the leaves of the gastrohepatic ligament and should be preserved (Fig. 5.5).
junction is divided transversely using electrocautery. In doing so, the hepatic branch of the anterior vagus nerve is sometimes visible in the leaves of the gastrohepatic ligament and should be preserved (Fig. 5.5).
After division of the peritoneum, the anterior vagus nerve can usually be seen on the anterior surface of the esophagus. The nerve can also be palpated with an index finger passed along the anterior surface of the esophagus. Retraction of the stomach caudally aids in the palpation of the vagal trunk by placing it on gentle tension (Fig. 5.6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree