Fig. 12.1
Port configuration. C: 5-mm or 12-mm camera port, L1-4: 5-mm working ports (inferior approach), L1-3: 5-mm working ports (superior approach)
Box 12.2. Tip
Placing another 5-mm trocar can often provide additional retraction and make the laparoscopic approach much easier. Whether it is a bulky omentum or small bowel loop that will not stay in place out of the way, the added retractor will go a long way facilitating success.
Given the complexity and difficulty of a laparoscopic transverse colectomy, some have advocated using a hand-assisted laparoscopic approach to facilitate the operation [8, 9]. This can be accomplished by placing the hand-assisted GelPortTM (Applied Medical, Rancho Santa Margarita, CA) device through a periumbilical midline incision or a Pfannenstiel incision, if an extracorporeal transverse colon to rectum or ileorectal anastomosis is performed. The surgeon’s hand placed inside the GelPortTM device can aid significantly in the retraction and blunt dissection of the colon. Reports have demonstrated a decrease in operative time compared to straight laparoscopic approaches [8, 9].
Operative Steps (Table 12.1)
Table 12.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Exploratory laparoscopy | 1 |
2. Omental division or resection | 3 |
3. Hepatic flexure mobilization | 4 |
4. Splenic flexure mobilization | 5 |
5. Identification and ligation of the middle colic vessels | 6 (inferior) |
5 (superior) | |
6. Extracorporeal anastomosis, closure, and re-inspection | 1 |
Exploratory Laparoscopy
Upon entry and adequate insufflation, a thorough inspection of the abdomen should be performed with emphasis on identifying the area of interest. Only when a transverse colectomy is the only operation should the ports be changed relative to this structure. Otherwise, the ports should be placed based on the entire operation as above and the operation will commence. The patient should be placed in a reverse Trendelenburg position to facilitate small bowel to fall into the pelvis and help isolate the transverse colon. Based on the flexure, the patient may be placed in a right-side down (splenic) or left-side down (hepatic) position. An oral gastric tube is placed by anesthesia and kept on low intermittent suction, as this will cause the stomach to collapse and provide better visualization.
Omental Division or Resection
The greater omentum may be resected with the specimen or removed off the colon and preserved (Box 12.3). For the latter, it is best to place it over the top of the transverse colon in the upper abdomen. Occasionally the falciform ligament will obstruct this and may need to be partially divided. The colon is retracted caudally and the omentum is held up to facilitate exposure of the avascular plane adjacent to the bowel wall. This may be divided with an energy device or endoscissors/electrocautery. When it is resected with the specimen, it can be divided from the greater curvature of the stomach with the use of an energy-based vessel-sealing device, such as a Ligasure, Enseal, or Harmonic scalpel, by going directly through the omentum itself (see Fig. 12.2). In this situation, the omentum should be left draping over the bowel wall initially. After identifying the transverse colon and anterior stomach, an energy device or electrocautery can be used to divide the omentum, leading directly into the lesser sac. Care should be made to avoid inadvertent damage to the gastroepiploic vessels.


Fig. 12.2
Entering lesser sac
Box 12.3. Tip
A large redundant colon will be very difficult to keep oriented properly. Divide the omentum first and follow with resection of the mesentery in a stepwise fashion.
Hepatic Flexure Mobilization
The hepatic flexure is mobilized by having the surgeon stand on the patients left side or in between the legs. The surgeon will have an atraumatic bowel grasper in the inferior left port and a dissector or bipolar vessel-sealing device in the upper left port. The assistant will have two atraumatic bowel graspers and will provide the appropriate exposure and retraction by standing on the patient’s right side or in between the legs. Using a lateral approach, the right lateral peritoneal edge around the hepatic flexure is divided and proceeds along the upper boarder of the transverse colon. Care must be taken to divide any adhesions to the gallbladder. The surgeon who is standing on the patient’s left side is grasping the colon carefully or preferably an epiploica and retracting the hepatic flexure towards the left lower quadrant via the left lower trocar. As the retraction continues and the hepatic flexure becomes more redundant, care must be taken to identify the underlying “C-loop” of the duodenum (see Fig. 12.3). This is of utmost importance that the duodenum be visualized clearly and kept away safely from any energy source and potential of injury.
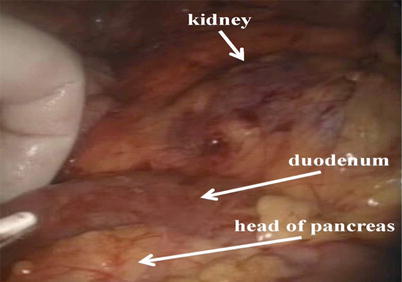
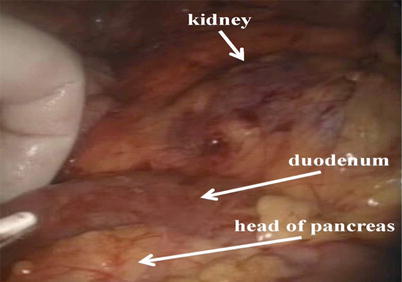
Fig. 12.3
Hepatic flexure mobilization
Splenic Flexure Mobilization
The splenic flexure is mobilized in a similar manner. The surgeon now stands on the patient’s right side or in between the legs and uses both right-sided ports for retraction and dissection. The assistant is on the opposite side, the left side of the patient, with two bowel graspers holding and retracting the colon appropriately. The surgeon starts out by mobilizing the lateral peritoneal attachments along the left colon. The lienocolic attachments can be carefully divided with the energy-based vessel-sealing device. The surgeon and the assistant must always be on the lookout not to vigorously retract the splenic flexure as this will lead to tears of the splenic capsule and can often cause significant bleeding and the potential of necessitating an emergent splenectomy. All adhesions to the spleen should be carefully ligated with minimal traction (see Fig. 12.4). As the splenic flexure is mobilized and becomes redundant, the surgeon should be able to visualize the tail of the pancreas. Visualizing the boarder of the tail of the pancreas will be an important landmark, as the duodenum was with the hepatic flexure (see Fig. 12.5).










