Fig. 26.1
U-shaped articulating holding system
Operative Proctoscope
The operating proctoscope is available in a standard 4 cm diameter. A variety of lengths are available (i.e., 7.5, 15, and 20 cm), which are typically selected depending on lesion location. The tip of the proctoscope is either straight or beveled and is introduced into the rectum using an appropriately sized obturator. The handle can then be secured to the holding system. The working faceplate of the device (see Fig. 26.2) contains the attachment for the telescope and three working channels. These include two smaller channels for 5 mm instruments and one larger channel that can accommodate up to 12 mm instruments. If needed, a stapler can then be introduced through the large working channel. Automatic sealing valves are used to prevent the loss of insufflation during the procedure and instrument exchanges. The proctoscope also has additional connectors for CO2 insufflations and evacuation. High flow CO2 insufflation through the proctoscope is initiated at 8 mmHg and can be increased up to 16 mmHg if required.


Fig. 26.2
Disposable working faceplate – the silicone sealing insert with the three channels covered with sealing caps is attached to the metallic faceplate
Optics
There are two options for imaging with the TEM. The original concept utilized a binocular with 30-degree optics (see Fig. 26.3). Visualization is through an attached eyepiece, and the binocular format gives a 3-D view for the surgeon, though not for the assistants. The binocular telescope can also be substituted for a 10 mm laparoscope with a corresponding sheath for rinsing and insufflation thus permitting on-screen visualization similar to laparoscopy [16]. The telescope is inserted through the appropriate optic port and spans the entire length of the proctoscope. The lens can be cleaned intraoperatively by instilling irrigation fluid through a Luer-Lok connector.
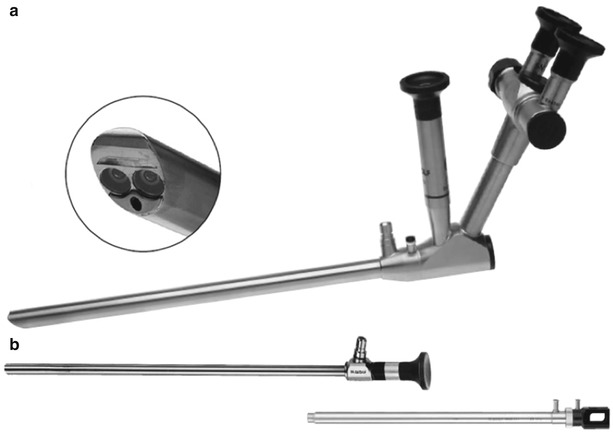
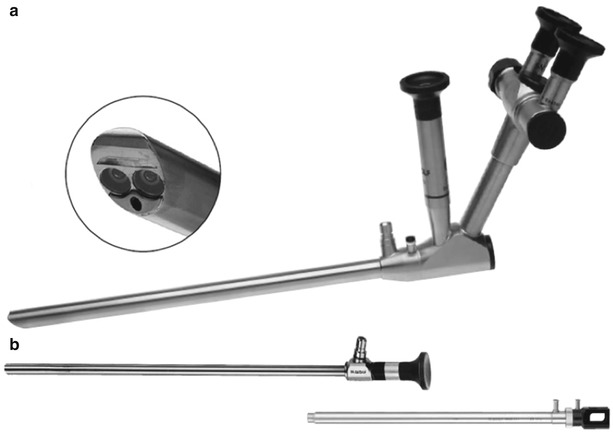
Fig. 26.3
Optics – (a) 30° binocular, 3D stereoscopic telescope with adjustable eyepiece. (b) 10 mm angled laparoscope with a corresponding sheath
Operating Instruments
A variety of long operating instruments are available for use with the transanal operating platform (see Fig. 26.4). These include various 5 mm forceps and scissors with either straight or offset downward tips. The instruments are available in both 36 and 43 cm working lengths and are equipped with interchangeable handles with or without a connector pin for unipolar coagulation. Various double-curved or straight cautery and suction/cautery devices are also available. The available 5 mm ports also allow for the use of standard needle drivers and energy devices. The larger 12 mm port allows for the use of a stapling device and a 10 mm clip applier.
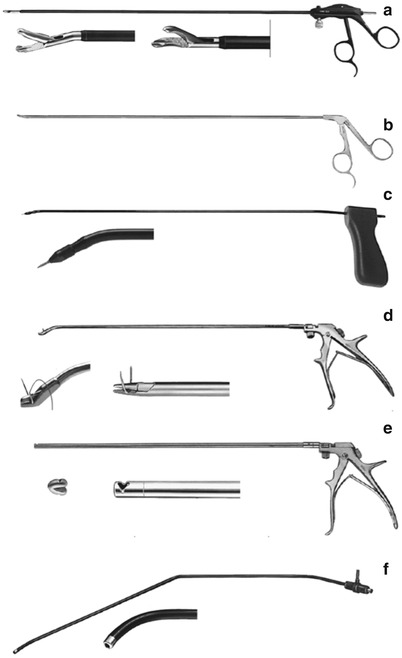
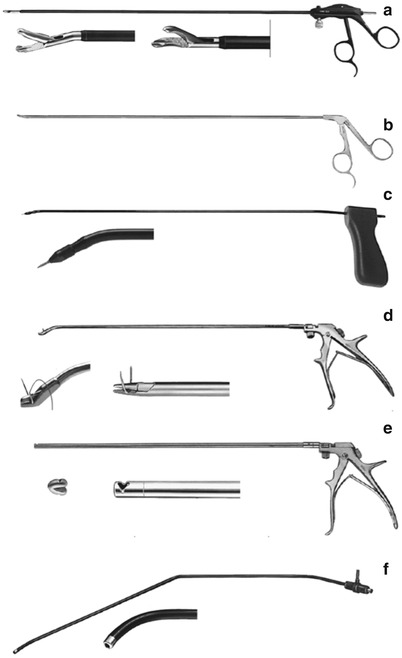
Fig. 26.4
Operating instruments – (a) grasping forceps with connection for monopolar cautery, angled and non-angled grasping tips are seen; (b) scissors; (c) needle tip monopolar knife; (d) needle holder, angled and non-angled tips are seen; (e) suture clip forceps, the silver suture clip is seen next to an enlarged image of the forceps tip; (f) angled coagulation/suction tube
Lesion excision is commonly performed with a monopolar cautery device. Routine laparoscopic ultrasonic shears or electrothermal bipolar vessel sealing systems may also be used if preferred by the operating surgeon.
Partial-Thickness Excision
Partial thickness (i.e., submucosal excision) may be utilized in the setting of benign disease as an alternative to a full-thickness resection. This may be particularly advantageous inlocations where full-thickness excision may be associated with increased risk of perforation or morbidity, or where healing complications are of concern [15]. These locations include: (1) the anterior proximal rectum where intraperitoneal perforation is particularly possible, although it does not increase morbidity [16]; (2) the anterior lower rectum in females, due to the increased risk of vaginal injury and a rectovaginal fistula; and (3) the very distal rectum in order to limit the risk of damaging the underlying sphincter mechanism, particularly in females.
Importantly, submucosal transanal excision should not be performed in the setting of a rectal malignancy or a malignant polyp, due to the risk of incomplete resection and increased local recurrence rates. It is, however, particularly suitable in the setting of large, benign, carpet-like sessile lesions [17] that may be difficult to resect in a full-thickness fashion, due to the risk of luminal stenosis or a difficult closure under tension.
Due to the risk of unexpected malignancy on final pathology, partial-thickness excision should be reserved for cases in which the likelihood of malignancy is very low. Such cases include biopsy-proven benign lesions with no visually concerning features such as ulceration and no evidence of submucosal invasion on endorectal ultrasound or other imaging. However, when an occult malignancy is identified on final pathology, the options for a full-thickness TEM resection or routine transabdominal resection remain, given that the TEM planes are essentially undisrupted.
Operative Steps (Table 26.1)
Table 26.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Establishing access and pneumorectum | 2 |
2. Marking | 3 |
3. Dissection and excision | 6 |
4. Removal of specimen | 2 |
5. Closure | 8 |
Establishing Access and Pneumorectum
The anus is dilated with three fingers prior to the insertion of the TEM platform. The bullitt obturator is locked into the proctoscope and well lubricated. It is inserted per anus as far as possible and the obturator removed. A faceplate with an insufflation and light cord attachment is used to identify the lesion to be excised and reexamine it to ensure its amenability to TEM excision. The proctoscope can then be attached to the table-mounted arm and the multiport faceplate attached. The bevel of the TEM cannula should be oriented to center on the lesion as much as possible.
Marking
One centimeter margins are marked circumferentially around the lesion using electrocautery on a “soft coag” setting (see Fig. 26.5, Video 26.1). A lifting solution consisting of a mix of saline, methylene blue, or indigo carmine with or without the addition of epinephrine is then injected into the submucosal space (see Video 26.2). Accurate injection into the submucosal space is crucial in order to obtain an adequate lift of the mucosal lesion, thus facilitating submucosal dissection. To allow for adequate lift, the injection may be started as the mucosa is punctured. This may improve the odds of infiltration of the lift solution at the proper submucosal space, as opposed to at the deeper layers. The quality of the lift should then be assessed, as non-lifting segments of the lesion may imply areas of deeper invasion and indicate the need of a full-thickness resection. Prior biopsies or tattooing of the lesion can result in a submucosal reaction, which may also manifest in a non-lifting segment and should be taken into consideration. For lesions oriented on the far side of a fold or very tangential to the scope, it may be helpful to first inject and lift the proximal margin in order to tilt it toward the endoscope.


Fig. 26.5
A resection margin of 1 cm is marked around the lesion using electrocautery (From the Oregon Clinic)
Dissection and Excision
Dissection and resection of the lesion begins by circumferentially incising the mucosa along the marked margins – usually starting with the proximal portion first if at all possible. A submucosal plane is established, and the leading edge of the segment that is to be resected is grasped and elevated away from the underlying circular muscle layer (see Fig. 26.6). This traction facilitates better delineation of the correct dissection plane in the deep submucosa along the circular muscle layer. The submucosal dissection then proceeds proximally (see Video 26.3).


Fig. 26.6
Dissection is performed in the submucosal plane (From the Oregon Clinic)
Removal of Specimen
Following the resection, the specimen is removed and must be mounted appropriately on a cork or wax board and submitted for pathologic examination (see Fig. 26.7).
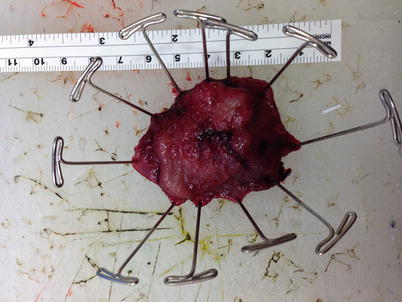
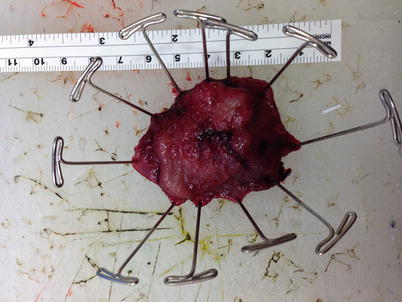
Fig. 26.7
Mounting of specimen for pathologic examination
Closure
Once the lesion has been excised, the site is inspected for bleeding or areas of full-thickness resection. A yellow color may be seen at the defect related to small amount of fat in the submucosal plane. This does not necessarily indicate a full-thickness perforation. Areas of full-thickness excision can be sutured closed. Areas of mucosal resection may be closed or left open at the surgeons’ discretion and according to the size of the defect and the perceived risk of bleeding.
Full-Thickness Excision
Full-thickness resection is the technique most commonly utilized during the TEM procedure and is applied for all known or suspected malignant lesions. In fact, full-thickness excision can also be utilized for a benign lesion and may obviate the need for further excision if an occult malignancy is identified on final pathology of a presumed benign lesion. It has been well documented that resections with entry into and closure of the peritoneum are acceptable and well tolerated with good endoluminal closure techniques [18].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








