Fig. 21.1
Port configuration. Hand port left or right hand, L1 working port, L2 optional working port
Box 21.1 Tip
An advanced technique utilizing only one working port through a planned ileostomy site will be described in the following single-port chapter; a “clockwise” mobilization can be combined with the hand port through a Pfannenstiel incision.
The hand port typically serves as the extraction site. It can be placed in the Pfannenstiel incision, which has the benefit of reduced incisional hernia rates. A lower midline incision has the benefit that it can be easily converted into a midline laparotomy if necessary. Both of these extraction sites allow easy access for an ileorectal anastomosis.
Operative Steps (Table 21.1)
Table 21.1
The operative steps of a hand-assisted laparoscopic colectomy
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Exploratory laparoscopy and insertion of the hand port | 1 |
2. Mobilization of the cecum and ascending colon and ligation of the ileocolic vessels | 3 (medial to lateral) |
2 (lateral to medial) | |
3. Mobilization of the hepatic flexure and transverse colon and ligation of the middle colic vessels | 5 (inferior) |
2 (superior) | |
4. Mobilization of the sigmoid colon, descending colon, and splenic flexure and ligation of the inferior mesenteric artery | 4 (medial to lateral) |
3 (superior) | |
2 (lateral to medial) | |
5. Transection of the colon, anastomosis, and reinspection | 3 |
The operative steps of a hand-assisted laparoscopic colectomy are similar to the steps described previously in the total laparoscopic chapter. It essentially combines a right, transverse, and left hemicolectomy.
Exploratory Laparoscopy and Insertion of the Hand Port
Pneumoperitoneum is established with carbon dioxide gas and maintained at 15 mmHg. After exploration of the abdominal cavity, additional 5-mm trocars are placed on either side of the umbilicus or in the RLQ and LLQ. A thorough exploration of the abdominal cavity is then completed.
After feasibility of a laparoscopic approach is confirmed, a Pfannenstiel incision is performed two fingerbreaths above the pubis. Dissection is carried out through the subcutaneous tissue down to the fascia. The fascia is opened transversely and subfascial planes are developed superiorly and inferiorly. The midline is identified and opened. The pneumoperitoneum is evacuated. The hand-assisted device is inserted and secured in placed.
Mobilization of the Cecum, Ascending Colon, and Hepatic Flexure and Ligation of the Ileocolic Vessels
Pneumoperitoneum is reestablished and the patient is placed in the reverse Trendelenburg, right lateral decubitus position. Typically the surgeon stands between the patient’s legs and uses the left hand for intra-abdominal retraction and the right for the energy device or bowel grasper through the LLQ port L2. The camera operator is typically on the left side of the patient with a 30-degree 5 mm laparoscope. The ligament of Treitz is identified, and the small intestine is evaluated in its entirety in patients with inflammatory bowel disease. By doing so the small bowel is placed in the left upper quadrant away from the operating field, thus facilitating the initial mobilization of the ileocolic vascular pedicle.
The surgeon moves to the patient’s left side next to the camera operator, the assistant stands on the patient’s left side, and the patient is placed in steep Trendelenburg and left lateral decubitus position. The ileocolic vascular pedicle is then identified, placed under tension with the left hand through the suprapubic hand port. The right hand can then dissect, divide, and ligate the pedicle with a vessel-sealing device after identification of the duodenum (see Fig. 21.2 and Video 21.1). Next, medial to lateral mobilization of the ascending colon is completed all the way up to the hepatic flexure in the submesenteric avascular plane (see Fig. 21.3 and Video 21.2). Attention is then turned to the lateral peritoneal attachments, which are taken down from the hepatic flexure to the cecum (see Video 21.3). The terminal ileum is completely mobilized to allow a tension-free anastomosis (see Video 21.4).
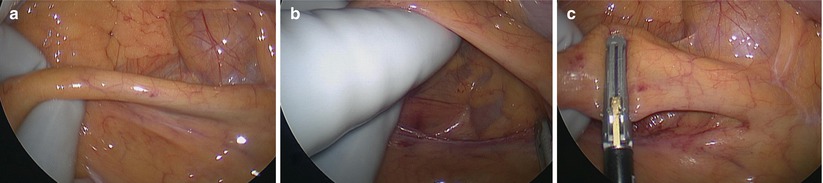
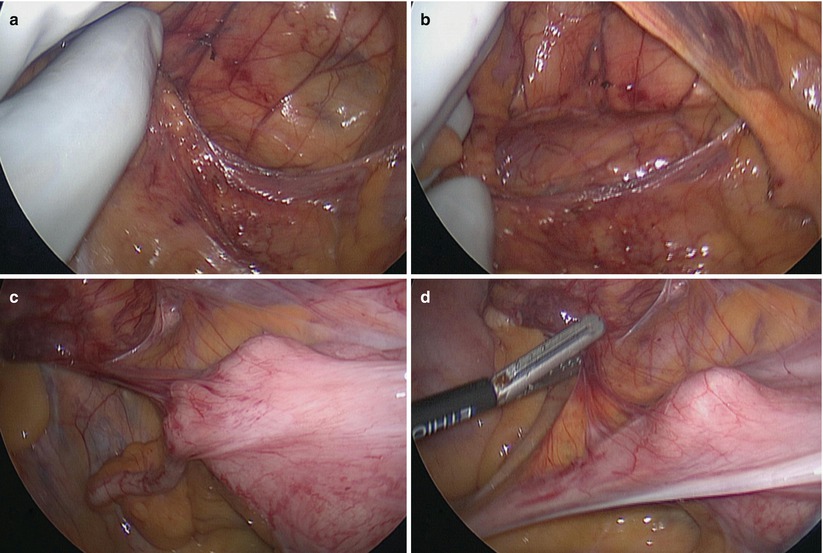
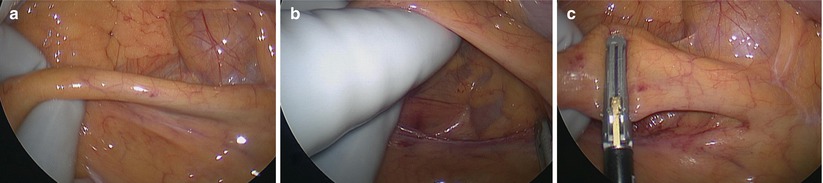
Fig. 21.2
Ileocolic division (a–c)
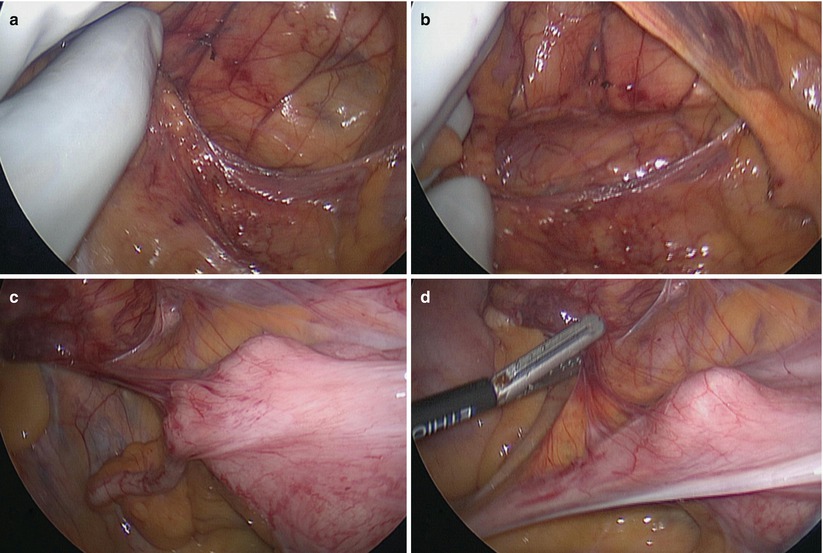
Fig. 21.3
Cecal mobilization (a–d)
Occasionally, preservation of the ileocolic pedicle for the ileoanal pouch is desired. In this case a lateral mobilization of the entire cecum, ascending colon, and hepatic flexure can be performed from lateral to medial. In this case the surgeon uses the right hand through the suprapubic hand port to retract and dissect with a left-handed instrument through the RLQ port L1. Sometimes, the surgeon can use the left hand for retraction and finger dissection along the line of Toldt similar to open surgery. The assistant can divide the peritoneal attachments through the RLQ port L1. The mesentery of the cecum is then divided close to the bowel wall.
Mobilization of the Transverse Colon and Ligation of the Middle Colic Vessels
With the surgeon now on the patient’s right side, the operating table is placed in reverse Trendelenburg and the transverse colon is mobilized from the hepatic (see Fig. 21.4 Video 21.5) to the splenic flexure by sequentially dividing and ligating the greater omentum just distal to the gastroepiploic arcade and the transverse mesocolon (see Video 21.6) (Boxes 21.2 and 21.3). The right hand retracts the transverse colon inferiorly and left laterally, while a left-handed instrument through the RLQ port L1 enters the lesser sac and subsequently divides the omentum. The omentum is taken with the specimen, thus facilitating and expediting the dissection. The transverse colon mesentery is taken close to the bowel wall in benign cases from the superior approach. The mesentery is located under the omentum as the next plane. For malignant cases isolation of the middle colic trunk from an inferior approach may be necessary. Therefore, an additional trocar may be needed for adequate retraction and exposure as described in a previous chapter (“Ole maneuver”).
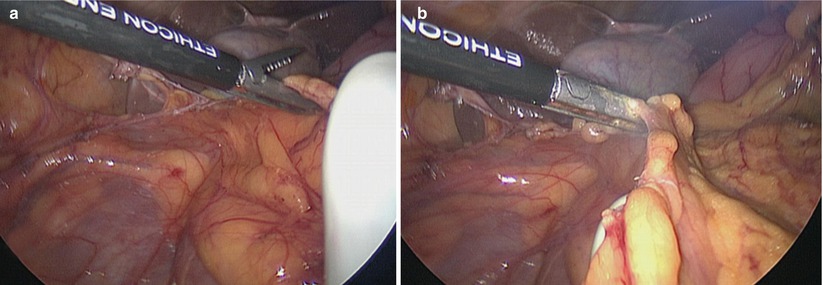
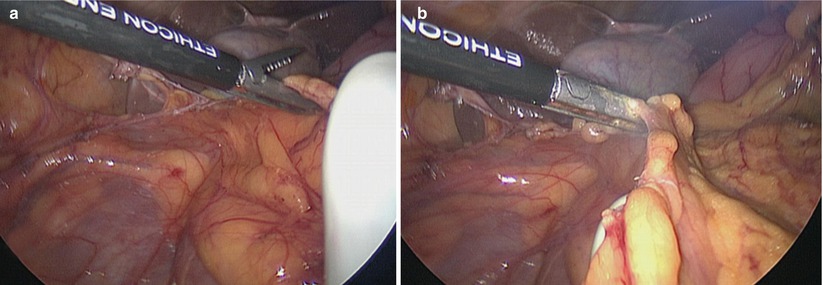
Fig. 21.4
Transverse colon mobilization (a, b)
Box 21.2 Tip
The hand facilitates dissection in the lesser sac exposing the omentum. At the same time the colon wall can be palpated to avoid injury from the energy device.
Box 21.3 Caveat
Identify the transverse colon mesentery versus small bowel mesentery at all times to avoid a devastating complication.
Mobilization of the Sigmoid Colon, Descending Colon, and Splenic Flexure and Ligation of the Inferior Mesenteric Artery
The splenic flexure is taken down bluntly and sharply usually in a superior fashion. Continuous, but careful downward, traction of the colon allows for division of the splenocolic ligament through the RLQ port and continuation along the line of Toldt. The colon mesentery is divided close to the bowel wall (see Video 21.7).
In difficult cases, especially with limited instrument reach from the right, a combination of superior (from the transverse colon) and lateral to medial (from the descending colon) mobilization is sometimes needed (see Fig. 21.5). In this scenario the surgeon is operating between the patient’s legs. The sigmoid and descending colon is mobilized all the way to the level of the rectosigmoid junction by sequentially dividing and ligating the lateral attachments and the mesentery through the LLQ port. The inferior mesenteric artery is typically preserved to maintain good vascularization of the distal stump for the anastomosis specifically in benign cases. For malignant cases a high ligation of the IMA is performed. This follows the medial to lateral technique described in a previous chapter of hand-assisted laparoscopic sigmoid resection. The surgeon’s right hand is retracting the sigmoid colon, while an instrument through the RLQ port L1 allows for dissection, isolation, and division of the IMA pedicle.
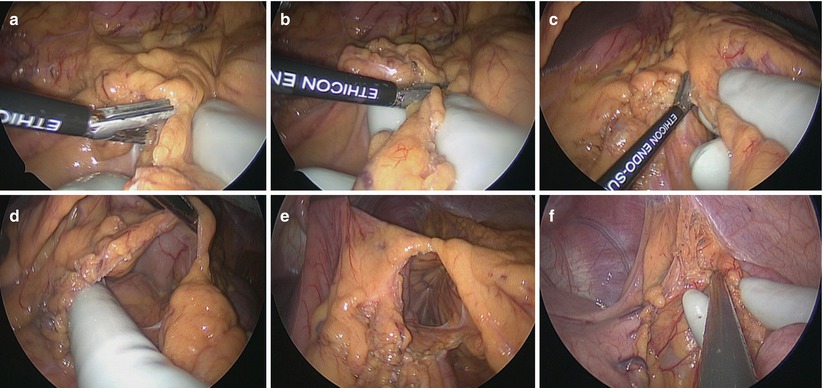
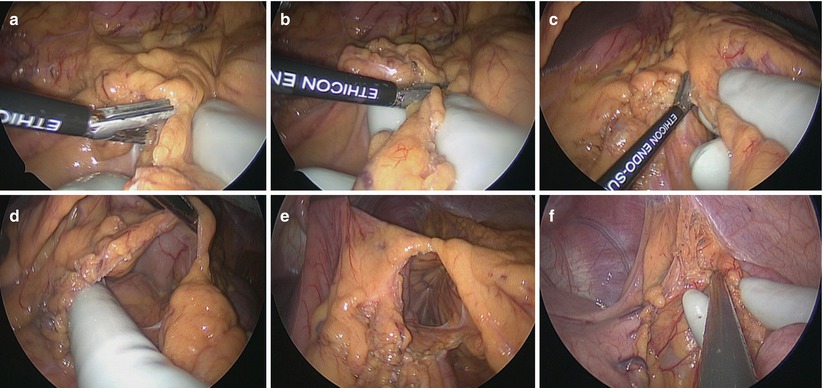
Fig. 21.5
Splenic flexure mobilization (a–f)
Transection of the Colon, Anastomosis, and Reinspection
At this point pneumoperitoneum is evacuated, and with a wound protector in place, the specimen is exteriorized through the Pfannenstiel incision (see Fig. 21.6). The terminal ileum is dissected off of the mesentery and divided with a GIA stapler. The ileal staple line can be reinforced with 4-0 nonabsorbable sutures.










