Colon cancer
Rectal cancer
Detection and removal of metachronous adenomas
Detection and removal of metachronous adenomas
Diagnosis of early metachronous cancer
Diagnosis of early metachronous cancer
Diagnosis of anastomotic and/or endoluminal recurrencesa
7.3 How Frequent Should Endoscopic Follow-Up Be?
Endoscopic FU is an established procedure in the surveillance protocols for patients operated on for CRC. However, despite the published guidelines, there is a high variability in the use of endoscopic surveillance following CRC surgery [15–19, 38–41]. Some studies have reported a suboptimal endoscopic FU, which has been related to patient characteristics like older age, presence of comorbidity, different ethnicity, and advanced stage of CRC [40–42]. Other studies have shown that many physicians have little familiarity with the published guidelines, with subsequent overuse or underuse of endoscopic FU [15–17, 19]. Besides the variable patterns of surveillance, the alarming data is that approximately 30 % of CRC survivors do not undergo any endoscopic FU within 3 years from surgery [41].
There is a certain variability about the timing of endoscopic FU after CRC surgery among the most recent published guidelines, which all recommend performing the first surveillance colonoscopy 1 year after surgery (Table 7.2) [4, 7, 12–14]. This recommendation originates from several studies that reported a high frequency of both metachronous advanced adenomas and cancer within the first 2 years after CRC surgery [4, 9, 31–35, 43, 44]. Moreover, the observation that local recurrences of rectal cancer occur within 30 months from surgery supports the need of intensive endoscopic FU of the anastomosis, starting at 6 months after rectal cancer surgery [7, 24, 44]. Recent studies have confirmed that the best interval between the first colonoscopy and CRC surgery is 1 year, provided that appropriate clearing of the colon has been achieved in the perioperative period [45–47].
Table 7.2
Summary of the latest guidelines for surveillance colonoscopy among CRC survivors
Recommending agency | Timing of first colonoscopy | Subsequent colonoscopies |
|---|---|---|
American Cancer Society | 1 year after surgery or 1 year after postoperative clearing colonoscopy | at 4 and 9 years after surgery; then every 5 years |
American Society of Gastrointestinal Endoscopy | 1 year after surgery or 1 year after postoperative clearing colonoscopy | at 3 and 5 years after surgery; then every 5 years |
European Society of Gastrointestinal Endoscopy | 1 year after surgery or 1 year after postoperative clearing colonoscopy | at 3 years after surgery; then every 5 years |
While the time of the first endoscopic FU has been clearly established, there is still uncertainty about the appropriate interval between subsequent colonoscopies for CRC survivors. Initial reports suggested that intensive endoscopic FU was beneficial for CRC survivors, improving their overall survival rate [48–50]. However, the results of several studies have shown that intensive endoscopic FU with frequent surveillance colonoscopies does not give a clear clinical benefit to CRC survivors, and therefore a reduction in frequency of the endoscopic FU after CRC surgery is appropriate [25, 51–55]. These observations support the recommendation of the current guidelines which suggest either surveillance colonoscopies at 3 and 5 years after the first normal endoscopic FU at 1 year from surgery or an interval of 3 and then 5 years after subsequent normal surveillance colonoscopies, following the first examination performed 1 year after surgical resection of CRC [4, 7, 12–14] (Table 7.2).
Recently, it has been proposed that endoscopic FU should be tailored for CRC survivors according to factors associated with an increased risk for metachronous cancer and/or local recurrence [56]. Some risk factors are related to the patient like older age, obesity, cigarette smoking, and alcohol intake, while others are linked to CRC like its distal location, microsatellite instability, and the presence of synchronous lesions [31–33, 57–59]. The only significant risk factor for metachronous advanced adenomas and/or cancer is the presence of synchronous adenomas at the time of perioperative colonoscopy [31–33, 57, 58]. According to these data, patients who undergo curative resection for CRC and have no synchronous neoplasms or have synchronous tubular adenomas without advanced features (Table 7.3) are at lower risk of developing metachronous adenomas and/or cancer [32, 57, 58]. For these patients a less intensive colonoscopic surveillance program may be appropriate, with a surveillance colonoscopy every 5 years, after the first normal endoscopic FU [4, 12, 52]. On the contrary, the presence of advanced synchronous adenomas at the time of perioperative colonoscopy carries a high risk of subsequent advanced metachronous neoplasia during the endoscopic FU, which therefore should be more frequent [32, 57]. These patients should undergo surveillance colonoscopy at 3 and 5 years after the first normal endoscopic FU, provided that no high-risk metachronous adenomas are diagnosed [7]. If this is the case, CRC survivors should undergo subsequent FU colonoscopy 1 year after the diagnosis of advanced adenoma, while the diagnosis of low-risk metachronous adenomas is indication for a 3-year repeat colonoscopy [9, 12, 53, 60]. Therefore, the findings at the time of surveillance colonoscopies will further tailor the endoscopic FU, modifying it according to the presence or the absence of metachronous adenomas and to their features [9, 12, 14, 32, 55].
Table 7.3
Features of colorectal adenomas
Low-risk adenomas | High-risk adenomas |
|---|---|
No more than three adenomas | Multiple adenomas (≥3) |
Size < 1 cm | Size > 1 cm |
Tubular histology | Villous or tubulovillous histology |
Low-grade dysplasia | High-grade dysplasia |
Patients with prior rectal cancer should undergo a tailored endoscopic FU, which is based on the type of surgery and the administration of neoadjuvant chemoradiation. Postoperative surveillance sigmoidoscopy is not recommended in patients treated with neoadjuvant chemoradiation and mesorectal excision, given the decreased likelihood of local cancer recurrence [7]. These patients should undergo standard endoscopic FU. On the contrary, an intensive endoscopic FU with sigmoidoscopy ± EUS every 3–6 months, for the first 3 years after surgery, is highly recommended for patients with rectal cancer who have undergone surgery without mesorectal excision and neoadjuvant chemoradiation [7, 60]. This intensive endoscopic FU helps to identify resectable local recurrences; however, it has not been shown to improve patient’s survival, and its only rationale is the high rate of local recurrences within the first 2–3 years from rectal surgery [4, 7, 24, 61]. Finally, a tailored approach is mandatory for patients with inherited syndromes of CRC. Hereditary non Polyposis Colorectal Cancer (HNPCC) patients diagnosed with CRC should undergo proctocolectomy, because of the high risk of metachronous cancer, which is 25 % after segmental colectomy and 8% after total colectomy with ileorectal anastomosis [62–64]. However, many HNPCC patients still undergo either segmental colectomy or total colectomy with ileorectal anastomosis, and therefore they require yearly surveillance colonoscopy or rectoscopy to remove premalignant adenomas [62–64]. Similarly, patients with Familial Adenomatous Polyposis (FAP) require strict endoscopic FU of the rectal stump or the ileal pouch [62, 65, 66]. Rectal cancer has been reported in 17 % of FAP patients with ileorectal anastomosis and in 8 % of cases with an ileal pouch [65]. These data confirm the recommendation that FAP patients should undergo intensive endoscopic FU, which forecast a proctosigmoidoscopy every 6–12 months, according to the number of adenomas detected [62, 65, 66].
7.4 How Long Should Endoscopic Follow-Up Last?
According to the natural history of CRC, FU should be discontinued 5 years after surgery [67]. However, the published guidelines recommend long-term endoscopic surveillance of CRC survivors because they have a lifelong risk of developing metachronous CRC [4, 7, 8, 10–14, 34, 68–73]. A retrospective study reported that metachronous CRCs occur in approximately 30 % of patients 5 years after the resection of the primary CRC [34]. The authors of another retrospective study calculated that the cumulative risk of metachronous CRCs ranges from 2 %, for 5 years CRC survivors, to 7 % for those patients who are alive 20 years after colorectal surgery [73]. Therefore, the risk of developing metachronous CRCs seems to increase continuously over time, after surgical resection of the primary CRC. Metachronous CRCs occur from 1 to 25 years after surgery among various studies, and this data justifies a lifelong endoscopic FU [34, 68–73]. The latter may explain the high rate of resectable metachronous CRCs which are diagnosed at an early stage, as compared to the general population [72, 73]. However, endoscopic FU does not prevent the occurrence of metachronous cancers in CRC survivors, probably because patients with a history of CRC cancer may differ biologically from patients with adenomatous polyps and are at higher risk for metachronous cancer [69]. This hypothesis is supported by the observation that the incidence rate of metachronous cancer in CRC survivors is 6.8 times higher than that observed among patients in the National Polyp Study Group [69]. Another possible explanation is a suboptimal adenoma detection rate during surveillance colonoscopy, due to several factors which are mainly related to the quality of bowel preparation , the cooperation of the patients during the exam, and the skills of the endoscopist [74]. All these factors reflect the imperfect nature of endoscopic FU and its possible failure to always accurately examine the entire colon at the time of a surveillance colonoscopy.
Provided that long-term endoscopic FU is mandatory and must be continued after the first 5 years of surveillance, CRC survivors should undergo a colonoscopy every 5 years, if the exam is normal, until the benefit is outweighed by comorbidity [14]. Indeed, the potential benefit of the endoscopic FU should be weighed against the potential risks of diagnostic and operative colonoscopy. Given bleeding and perforation risks of 2.0 and 0.38 %, respectively, and a 5-year cumulative prevalence of non-advanced adenomas of 56.6 %, it has been estimated that 4 % of the CRC survivors will suffer from a major complication after 3 subsequent surveillance colonoscopies [75, 76]. This complication rate should be weighed against the substantially reduced potential survival benefit granted to elderly CRC survivors from removal of metachronous adenomas [77]. Elderly patients often have significant concomitant illnesses which increase the risk of death. These competing causes of death can overwhelm any benefit of endoscopic FU for CRC survivors older than 65 years of age [78]. Therefore, discontinuation of endoscopic FU should be considered in elderly CRC survivors and/or in presence of comorbidities according to the physician’s judgment [4, 7, 12, 13].
7.5 Is Endoscopic Follow-Up Cost-Effective?
The potential benefits of endoscopic FU after surgical resection of CRC include improved overall survival , better monitoring of outcomes , identification of other treatable colorectal lesions diagnosed during surveillance, and greater psychological support of the patients [5, 9, 78, 79]. These benefits must be carefully weighed against the potential negative physical, financial, and psychological consequences of postoperative surveillance of CRC survivors; moreover, cost/benefit ratio of the FU should be sufficiently favorable to justify its routine use [80].
According to an estimate of the British National Health System, endoscopic FU included in a postoperative surveillance regimen lasting 5 years is not cost-effective because of its uncertain benefit [14]. On the other hand, two recent retrospective studies reported that CRC survivors who undergo endoscopic FU appear to have improved survival, providing the strongest evidence to date of the effectiveness of endoscopic surveillance for CRC survivors [5, 9]. As previously stated, the number of colonoscopies needed to detect a metachronous cancer in CRC survivors, irrespectively of the time of diagnosis, is 157, with a relatively high cost of endoscopic FU [4, 12]. However, the possibility of diagnosing metachronous CRCs leads to significant improvement in life expectancy of CRC survivors, and this compensates for the relatively high costs of endoscopic FU [35]. Similarly, using a decision model analysis, it has been demonstrated that performing colonoscopy 1 year after colorectal surgery for CRC is a cost-effective option [35]. Therefore, endoscopic FU seems to be a highly cost-effective strategy in terms of metachronous CRCs detection and cancer-specific death prevention.
7.6 Conclusion
Endoscopic FU is a crucial component of postoperative surveillance of patients operated on for CRC. It has been shown to be cost-effective because it is capable of improving survival of CRC survivors at a relatively affordable economic and social cost. Despite the published guidelines, its timing is still uncertain and most likely the best strategy is to tailor endoscopic FU, according to the findings of both perioperative colonoscopy and surveillance endoscopies (Figs. 7.1 and 7.2).
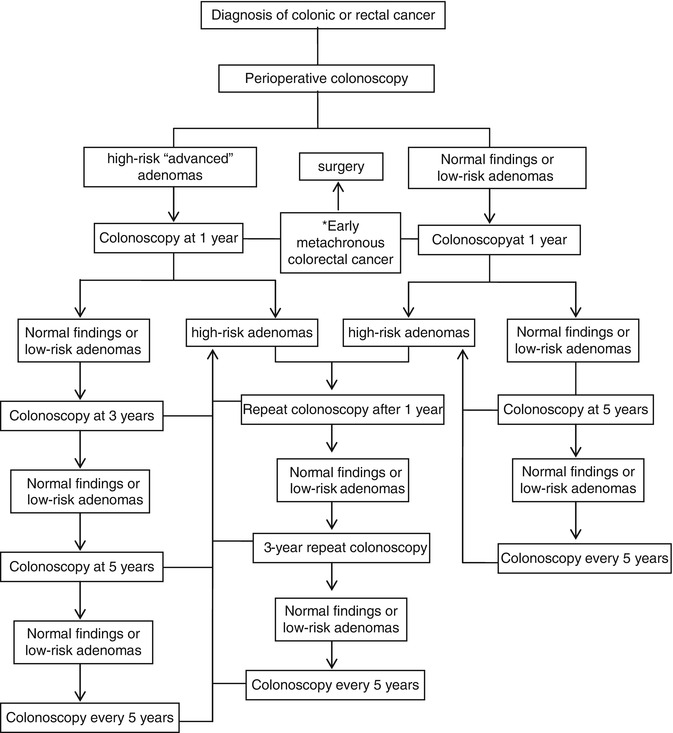
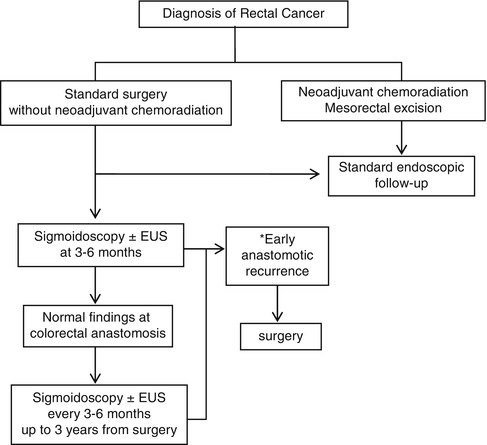
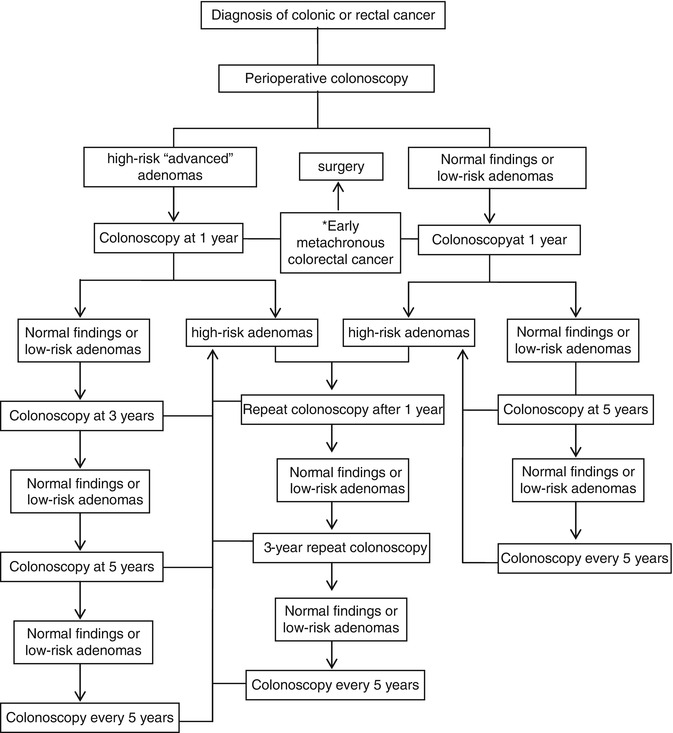
Fig. 7.1
Proposed algorithm for a tailored endoscopic follow-up of CRC survivors. *The diagnosis of early metachronous cancer is indication for surgery at any time during endoscopic follow-up. HNPCC patients who undergo segmental colectomy require yearly surveillance colonoscopy. Endoscopic FU will be continued until the benefit is outweighed by comorbidity
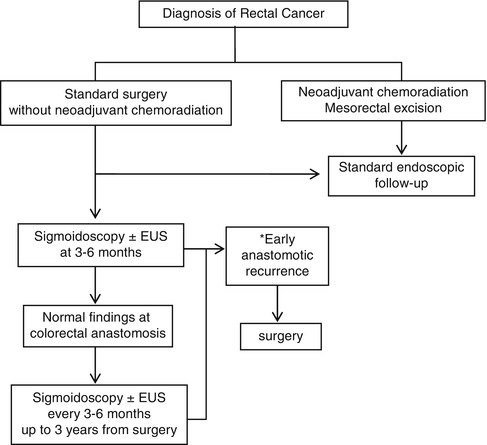
Fig. 7.2
Proposed algorithm for additional tailored endoscopic follow-up of CRC survivors after rectal surgery. *The diagnosis of early anastomotic recurrence is indication for surgery at any time during endoscopic follow-up. HNPCC patients who have undergone total colectomy with ileorectal anastomosis require yearly surveillance proctoscopy. Operated FAP patients require strict endoscopic FU of the rectal stump or the ileal pouch. FAP patients should undergo proctosigmoidoscopy every 6–12 months, based on the number of adenomas detected during the exam
Acknowledgements
The authors are grateful to Dr. Alessandra Trocino, Librarian at the National Cancer Institute and G Pascale Foundation of Naples, Italy, for her bibliographic assistance.
References
1.
Brawarsky P, Neville BA, Fitzmaurice GM (2013) Surveillance after resection for colorectal cancer. Cancer 119:1235–1242PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








