This article discusses the tension-free vaginal tape (TVT) procedure, which attempts to recreate urethral support at the level of the pubourethral ligaments by placing a polypropylene sling at the midurethra as opposed to the bladder neck. The procedure has the proposed advantage of being done under local anesthesia and being an outpatient surgery and can be performed transvaginally or suprapubically.
The first sling operation was reported by Von Giordano in 1907. Von Giordano used a gracilis muscle flap in a patient with epispadias. In 1970, the Goebell-Frankenheim-Stoekel procedure was described during which the perimedalis muscle and rectus fascia was plicated beneath the urethra. In 1942, Aldridge incorporated the use of rectus fascia and used a separate vaginal incision to incorporate the rectus fascia sling. In addition to muscle and rectus fascia, inorganic materials also have been used for sling grafts. Suburethral slings have been modified by changing the sling material and the anchoring point of the sling. Even with modifications, however, slings basically adhere to the principle of supporting the proximal urethra or bladder neck in a hammock-like fashion, providing a backboard against increases in abdominal pressure.
In 1995, Petros and Ulmsten reported on a new ambulatory surgical procedure for the treatment of genuine stress incontinence. The procedure eventually evolved into the tension-free vaginal tape (TVT) procedure. This procedure attempts to recreate urethral support at the level of the pubourethral ligaments by placing a polypropylene sling at the midurethra as opposed to the bladder neck. This synthetic sling is not tied or attached to any other structures. The procedure has the proposed advantages of being done under local anesthesia and being an outpatient surgery.
Technique
Transvaginal Approach
In the operating room, the patient is placed in the dorsal supine lithotomy position and prepped and draped in the normal, sterile fashion. The authors routinely have given preoperative antibiotics in the form of first-generation cephalosporin, although randomized data to support this approach are lacking. The bladder is drained with a transurethral 16-Fr Foley catheter. The location of the suprapubic stab incisions is marked with a marking pencil. These incisions should be at the level of the pubic symphysis just lateral to the midline. Placing these incisions too far laterally brings them in close proximity to the pubic tubercle, which potentially risks injury to the ilioinguinal nerves. The skin is infiltrated with 1% lidocaine with epinephrine. The infiltration is initially submucosal and then continues along the backside of the pubic symphysis. Approximately 10 mL of 1% lidocaine with epinephrine is used on either side.
Hydrodissection of the mid to distal anterior vaginal wall is performed with the same solution (approximately 8–10 mL). A 1-cm incision is made in the midurethra. It is sometimes helpful to feel the bladder neck with the Foley bulb in place to insure that the incision and subsequent placement of the sling is in the midurethra. Allis clamps are placed on the lateral edges of the incision, and Mayo or Metzenbaum scissors are used to create tunnels laterally toward the inferior pubic ramus ( Fig. 1 ). While creating the tunnels, the scissors should be pointed and dissecting toward the ipisilateral shoulder. The tunnel should be no bigger than the diameter of the scissors. The scissors should not penetrate the urogenital diaphragm, as this area is important for fixation of the Prolene sling. Because the TVT needle is passed blindly through the retropubic space, a clear understanding of retropubic anatomy is important in avoiding injury to important structures.
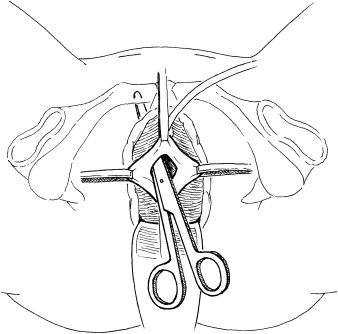
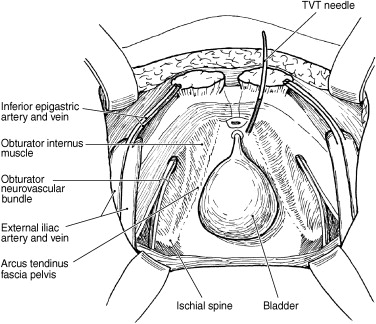
Fig. 2 demonstrates the anatomy of the retropubic space. The pubic symphysis is oriented at the 12 o’clock position. Under the pubic symphysis, the urethra is visible coming back to the bladder neck. The arcus tendinous fascia pelvis extends from the back of the pubic symphysis to the ischial spine and is the origin of the levator ani muscles. Above this area, the obturator internus muscle, lateral to the pubic symphysis, is seen, and above the arcus, the obturator neurovascular bundle is seen. Approximately 40% of the time, the obturator artery comes from the external iliac vessels, which exit just under the inguinal ligament into the lower limb. The remaining portion of the time, the obturator artery comes from the anterior division of the obturator artery. Another important blood vessel is the inferior epigastric vessel, which originates from the external iliac and proceeds medially and cephalad toward the rectus abdominus muscles. Muir and colleagues described the relationship of these vessels to a properly placed TVT needle in 10 fresh cadavers. Distances were measured from the needle to the vessel and from the midpubic bone to the vessel ( Table 1 ).
| Vessels | TVT Needle | Midpubic Bone |
|---|---|---|
| Superficial epigastric | 3.9 (0.9–6.7) | 7.2 (4.4–9.3) |
| Inferior epigastric | 3.9 (1.9–6.6) | 7.4 (4.8–10.0) |
| External iliac | 4.9 (2.9–6.2) | 8.3 (6.5–10.9) |
| Obturator | 3.2 (1.6–4.3) | 6.9 (5.2–8.4) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






