I. THE KIDNEY FUNCTION AND BLOOD PRESSURE IN NORMAL PREGNANCY.
The anatomy and function of the kidneys and lower urinary tract are altered during gestation. Physiologic alterations in volume homeostasis and blood pressure (BP) control also occur, and recognizing this is a prerequisite for the appropriate interpretation of data from pregnant patients with renal disease or hypertension (
Table 14-1).
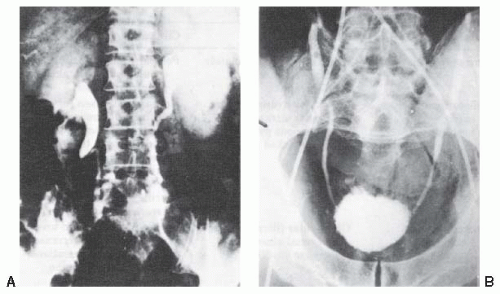
A. Anatomic and Functional Changes in Urinary Tract. Kidney length increases approximately 1 cm during normal gestation. The major anatomic alterations of the urinary tract during pregnancy, however, are seen in the collecting system, where calyces, renal pelves, and ureters dilate often giving the erroneous impression of obstructive uropathy. The dilation is accompanied by hypertrophy of ureteral smooth muscle and hyperplasia of its connective tissue, but whether bladder reflux is more common in gravidas is unclear. The cause of the ureteral dilation is disputed. Some researchers favor hormonal mechanisms, whereas other researchers believe that it is obstructive in origin. Clearly, as pregnancy progresses, assumption of a supine or upright posture may cause ureteral obstruction when the enlarged uterus entraps the ureters at the pelvic brim (
Fig. 14-1). These morphologic changes result in stasis in the urinary tract and a propensity of pregnant women with asymptomatic bacteriuria to develop pyelonephritis, especially in women with a history of prior urinary tract infection (UTI).
Acceptable norms of kidney size increase should be by 1 cm if estimated during pregnancy or the immediate puerperium, and reductions of renal length noted several months postpartum need not be attributed to renal disease. Rarely, ureteral dilation is of sufficient magnitude to cause a “distension” syndrome (characterized by abdominal pain, and on occasion small increments in serum creatinine levels presenting in late gestation; these resolve with the placement of ureteral stents). Also, because dilation of the ureters may persist until the 12th postpartum week, elective ultrasonographic or radiologic examination of the urinary tract should be deferred, if possible, until after this time.
B. Renal Hemodynamics. The changes in renal hemodynamics in gestation are the most striking and clinically significant of all the urinary tract alterations of pregnancy.
1. Glomerular filtration rate (GFR) and renal plasma flow (RPF) increase to levels 30% and 50%, respectively, above nongravid values during pregnancy. Increments in GFR that are already present during the early days after conception reach a maximum during the first trimester. The basis for the increase in GFR and RPF is unknown. Animal studies suggest that renal vasodilation [mediated by nitric oxide (NO)] leading to increased glomerular plasma flow is a contributing, but not the sole, factor. RPF is greatest at midgestation, declining somewhat in the third trimester. Although increments in GFR measured by the infusion of inulin appear to be sustained until term, 24-hour creatinine clearance declines during the last 4 weeks of pregnancy, accompanied by increases in serum creatinine levels of 15% to 20%.
The increase in GFR has important clinical implications. Because creatinine production is unchanged during pregnancy, increments in its clearance result in decreased serum levels. Using the Hare method, one group of investigators observed that true serum creatinine, which averaged 0.67 mg/dL in nongravid women, decreased to 0.46 mg/dL during gestation [to convert to SI units (µmol/L), multiply serum creatinine (mg/dL) by 88.4]. In studies that also measured creatinine chromogen (which yielded results resembling those reported in most clinical laboratories), values were 0.83 mg/dL in nonpregnant women and decreased to 0.74, 0.58, and 0.53 mg/dL in the first, second, and third trimester
of pregnancy, respectively. Therefore, values considered normal in nongravid women may reflect decreased renal function during pregnancy. For example, in gravid women, concentrations of serum creatinine exceeding 0.8 mg/dL or of serum urea nitrogen that are greater than 13 mg/dL suggest the need for additional evaluation of renal function.
2. Other Consequences of the Increased Renal Hemodynamics. Increased GFR and RPF also alter urinary solute content. For example, excretion of glucose, most amino acids, and several water-soluble vitamins increases, and these increments in the nutrient content of urine may be a factor in the enhanced susceptibility of gravidas to UTIs. Urinary protein excretion also increases during gestation, but the fate of albumin excretion is more complex and disputed.
C. Acid-Base Regulation in Pregnancy. Renal acid-base regulation is altered during gestation. The bicarbonate threshold decreases, and early morning urines are often more alkaline than those in the nongravid state. In addition, plasma bicarbonate concentrations decrease approximately 4 µmol/L, averaging 22 µmol/L. This change most likely represents a compensatory renal response to hypocapnia, because pregnant women hyperventilate and their PCO2 averages only 30 mmHg. The mild alkalosis (arterial pH averages 7.44) found in pregnancy is in accord with this view. Because steadystate PCO2 and HCO3 levels are already diminished, pregnant women are, in theory, at a disadvantage when threatened by sudden metabolic acidosis [e.g., lactic acidosis in preeclampsia, diabetic ketoacidosis, or acute kidney injury (AKI)]; however, they respond with appropriate increments in urinary titratable acid and ammonia after an acid load, and proton regeneration is already evident at blood pH levels higher than those in similarly tested nonpregnant women. Finally, when managing gravidas with pulmonary disorders, it should be noted that a PCO2 of 40 mmHg, normal in nonpregnant women, signifies considerable carbon dioxide retention in pregnancy.
D. Water Excretion. After conception, a rapid decrease in plasma osmolality levels of 5 to 10 mOsm/kg below that of nongravid subjects occurs. If this decrease occurred in a nonpregnant woman, she would cease secreting antidiuretic hormone and enter a state of water diuresis; however, gravidas maintain this new osmolality, diluting and concentrating urine appropriately when the woman is subjected to water loading or dehydration. This suggests a resetting of the osmoreceptor system, and, indeed, clinical studies demonstrate that the osmotic thresholds for both thirst and arginine vasopressin (AVP) release are decreased in pregnant women. Furthermore, the plasma of pregnant women contains large quantities of a placental enzyme (vasopressinase) capable of destroying substantial quantities of AVP in vitro; moreover, the in vivo production and metabolic clearance of AVP hormone are increased fourfold after midgestation.
The changes in osmoregulation and AVP metabolism may be responsible for two unusual syndromes of transient diabetes insipidus that complicate pregnancy. One, in which polyuria is responsive to both AVP and deamino-8-D-arginine vasopressin (dDAVP), probably occurs in women with unapparent partial central diabetes insipidus whose disease is brought to the fore by the increment in hormonal disposal rates during late gestation. The other disorder, in which the marked polyuria continues despite large doses of AVP, is responsive to dDAVP, an analog resistant to inactivation by
vasopressinase. These gravidas may have excessively high circulating levels of this aminopeptidase enzyme due to increased activation.
E. Volume Regulation. Most healthy women gain approximately 12.5 kg during the first pregnancy and 1 kg less during subsequent pregnancies. Most of the increment is fluid, with total body water increasing 6 to 8 L, 4 to 6 L of which is extracellular. Plasma volume increases 50% during gestation, the largest rate of increment occurring during midpregnancy, whereas increments in the interstitial space are greatest in the third trimester. A gradual cumulative retention of approximately 900 mEq of sodium occurs in pregnancy; this is distributed between the products of conception and the maternal extracellular space. These alterations in maternal intravascular and interstitial compartments produce apparent hypervolemia, yet the gravida’s volume receptors sense these changes as normal. Therefore, when salt restriction or diuretic therapy limits this physiologic expansion, maternal responses resemble those in salt-depleted nonpregnant women. This is one compelling reason for the reluctance to recommend sodium restriction or diuretics during pregnancy. Pregnant women are now advised to salt their food to taste, and some researchers believe that a liberal sodium intake is beneficial during gestation. Another physiologic adaptation that appears to influence sodium balance during pregnancy is the marked stimulation of the renin-angiotensin-aldosterone system. Aldosterone levels are markedly increased during pregnancy, despite normal BP and normal potassium balance. It is likely that the increased aldosterone secretion is a compensatory mechanism to counteract the increase in sodium excretion that would be expected as a result of the large increase in GFR and RPF. Arterial vasodilation that causes relative arterial underfilling, as occurs in pregnancy, is known to stimulate the renin-angiotensin-aldosterone system. Moreover, increases in aldosterone balance the natriuretic effects of the large increases in progesterone during pregnancy.
F. BP Regulation. Mean BP starts to decrease early in gestation, with diastolic levels in midpregnancy averaging 10 mmHg less than measurements postpartum. In later pregnancy, BP increases, gradually approaching nonpregnancy values near term. Because cardiac output rises quickly in the first trimester and remains relatively constant thereafter, the decrease in pressure is due to a marked decrement in systemic vascular resistance. The slow rise toward nonpregnant levels after a midtrimester nadir is interesting, because it demonstrates that increasing vasoconstrictor tone is a feature of late gestation in healthy women as well as in women in whom preeclampsia is developing. The cause of the decrease in systemic vascular resistance during pregnancy is obscure. Studies of arterial compliance in pregnancy demonstrate early rises, perhaps due to alterations in vessel ground substance. Elevations of plasma estrogen and progesterone to concentrations that may relax smooth muscle occur, and increments in vasodilating prostaglandins and relaxin are also present during gestation. Hormonally mediated increases in endothelial NO production may also contribute to the vasodilation in pregnancy. With the lower BP, the levels of all components of the renin-angiotensin system are increased during pregnancy. Exaggerated hypotensive responses to converting enzyme inhibition in normal gravidas suggest that the increased renin-angiotensin system in pregnancy is a normal physiologic response to decreased BP and increased sodium excretion.
Lack of awareness of the fluctuation in BP during normal gestation may lead to diagnostic errors. For example, women with mild essential hypertension often experience a decrease in BP during early pregnancy, and BP may even approach normal levels. They may then be erroneously labeled preeclamptic in the last trimester, when frankly elevated pressures occur.
G. Mineral Metabolism. Serum calcium levels decrease in pregnancy, in conjunction with a decrement in circulating albumin concentrations. Ionized calcium levels, however, remain in the normal nonpregnant range. Striking changes relating to calcium regulatory hormones also occur during normal pregnancy. Production of 1,25-dihydroxyvitamin D3 increases as early as the first trimester, reaching circulating levels that are approximately twice the nonpregnant values. Gastrointestinal absorption of calcium increases, resulting in an “absorptive hypercalciuria,” with 24-hour urine excretion often exceeding 300 mg/day (in appropriately nourished individuals). Intact parathyroid hormone levels are lower during normal pregnancy.
II. CLINICAL EVALUATION OF RENAL FUNCTION IN PREGNANCY
A. Examination of the Urine. The association of proteinuria with eclampsia was first noted in the 1840s, and the science of prenatal care advanced dramatically when physicians began to systematically examine the urine of gravidas, primarily for albuminuria. In certain instances, latent renal disease is first uncovered by the detection of excessive protein excretion or microscopic hematuria during a routine prenatal evaluation.
Healthy nonpregnant women excrete considerably less than 100 mg of protein in the urine daily, but due to the relative imprecision and variability of testing methods used in hospital laboratories, proteinuria is not considered abnormal until it exceeds 150 mg/day. During pregnancy, protein excretion increases, and excretion up to 300 mg/day may still be normal. On occasion, a healthy gravida can excrete more than that amount. In pregnancy, the gold standard for evaluation of abnormal proteinuria is the 24-hour urine protein measurement. A 24-hour protein excretion of greater than 300 mg is abnormal in pregnancy and correlates with a urine dipstick 1+ protein measurement. Although commonly used to detect proteinuria, urine dipstick testing is susceptible to error due to variations in urine concentration; therefore, if the level of suspicion is high, 24-hour urine testing should be performed. Total protein/creatinine ratio has been shown to accurately estimate 24-hour urine protein excretion in nonpregnant patients. In pregnancy, however, the urine protein/creatinine ratio does not adequately exclude the equivalent of 0.3 g per 24-hour proteinuria and underestimates severe proteinuria.
Few attempts have been made to quantitate the urine sediment in pregnancy. The excretion of both red and white blood cells may increase during normal gestation, and one to two red blood cells per high-power field is acceptable in a urinalysis.
B. Renal Function Tests. The clearance of endogenous creatinine, the most satisfactory approximation of GFR in nongravid subjects, is equally useful for assessing renal function in gravidas. Gravidas, as well as nonpregnant women, show little variation (approximately 10% per day) in urinary
creatinine excretion and, presumably, in creatinine production, which in a given woman is similar both during and after gestation. The lower limit of normal creatinine clearance during gestation should be 30% greater than the average of 110 to 115 mL/minute for nongravid women. Calculation of GFR by serum creatinine-based formulae is confounded by increasing maternal weight which is not muscle weight, and neither Modification of Diet in Renal Disease (MDRD) nor Cockroft-Gault GFR estimates have been validated in pregnancy.
Acid excretion and urinary concentration and dilution are similar in gravid and nonpregnant women. Therefore, tests such as ammonium loading (rarely indicated in gestation) give values similar to those in nongravid women. When examining urinary diluting ability, the clinician should be aware that supine posture can interfere with this test. Therefore, studies to detect minimal urinary osmolal concentrations should be performed with the patient lying on her side. However, although lateral recumbency is the required position for prenatal measurement of most renal function parameters, this posture interferes with tests of concentration. For example, a urine osmolality that was 800 mOsm/kg after overnight dehydration may decrease to 400 mOsm/kg within 1 hour through fluid mobilization from the extremities during bed rest, thereby resulting in volume-induced inhibition of AVP secretion, a mild osmotic diuresis, or both. These observations demonstrate the importance of upright posture, such as quiet sitting, when maximum urinary concentration is measured in pregnancy.
C. Role of Renal Biopsy in Pregnancy. Percutaneous renal biopsy is performed infrequently during gestation. In fact, pregnancy was once considered a relative contraindication to the procedure because of early reports of excessive bleeding and other complications in gravid women. It is now evident that if the renal biopsy is performed in women with well-controlled BP and normal coagulation indices, morbidity is similar to that of nonpregnant patients. Renal biopsy should be considered only when renal function suddenly deteriorates remote from term and no obvious cause is present. This is because certain forms of rapidly progressive glomerulonephritis, when diagnosed early, may respond to aggressive treatment such as steroid pulses and, perhaps, plasma exchange. Another situation in which biopsy may be recommended is symptomatic nephrotic syndrome. Although some might consider a therapeutic trial of steroids in such cases, it may be prudent to determine beforehand whether the lesion is likely to respond to steroids, because pregnancy is itself a hypercoagulable state prone to worsening by such treatment. Biopsy can usually be deferred when proteinuria alone develops in a normotensive woman with well-preserved renal function who has neither marked hypoalbuminemia nor intolerable edema. These women can usually be evaluated at more frequent intervals, and monitored for signs of either deterioration in renal function or development of superimposed preeclampsia, and renal biopsy deferred to the postpartum period. Similarly, there is rarely a need for renal biopsy during pregnancy in women with normal renal function and asymptomatic microscopic hematuria, when neither stone nor tumor is suggested by ultrasonography. Later in pregnancy (after 30 weeks) biopsy is rarely indicated and almost always should be deferred until after delivery.
III. RENAL DISEASE IN PREGNANCY
A. Asymptomatic Bacteriuria. UTI is the most common renal problem occurring in pregnancy. The urine of gravidas supports bacterial growth better than that of nonpregnant women because of its increased nutrient content. This, as well as ureteral dilation, stasis, and occasional obstruction, would be expected to increase the susceptibility of pregnant women to UTI. Surprisingly, this is not the case and, with the exception of certain high-risk groups (diabetic patients and gravidas with sickle cell trait), the prevalence of asymptomatic bacteriuria during gestation varies between 4% and 7%, a value similar to that in sexually active nonpregnant women. The natural history of asymptomatic UTIs is, however, quite different in pregnancy.
Although in the nonpregnant state asymptomatic bacteriuria is quite benign, progression to overt cystitis or pyelonephritis occurs in up to 40% of affected gravidas. Therefore, screening all pregnant women for the presence of asymptomatic bacteriuria and treating those with positive urine cultures are important.
1. Method of Urine Collection. Pregnant women contaminate midstream urine specimens more frequently. The incidence can be reduced by the use of multiple vulval washings combined with carefully supervised collection procedures. In some women, suprapubic aspiration is required to differentiate contamination from true infection. Pregnancy is not a contraindication to this procedure.
If the urine is sterile at the beginning of pregnancy, it usually remains so until term. Still, a small number (1% to 2%) of gravidas whose original urine cultures are negative subsequently have bacteriuria. Abnormal urinalysis and the presence of dysuria do not differentiate between contamination and true infection. For example, dysuria occurs in 30% of gravidas whose urines are sterile, and the urine may be infected and still contain fewer than two leukocytes per high-power field.
2. Method of Treatment. The optimum way to manage asymptomatic UTI in pregnancy has not been precisely defined. In the earlier literature, some authors recommended continuous antibiotic treatment from the time the bacteriuria was detected until delivery. This was based on the belief that the relapse rate was high, and that most bacteriuric women have renal parenchymal involvement as opposed to bladder infection. However, it is now apparent that one-half of these infections involve only the bladder, and most of these patients are cured by standard shortcourse (or even single-dose) therapy. More than 90% of the uropathogens involved are aerobic gram-negative rods, usually Escherichia coli, and the physicians recommend a 4- to 7-day course of the antibiotic to which the cultured organism is sensitive, preferably a short-acting sulfa drug, nitrofurantoin, amoxicillin, a cephalosporin, or a single dose of fosfomycin. This approach, when combined with surveillance for recurrent bacteriuria, has been shown to be quite effective.
3. Importance of Postpartum Evaluation. Asymptomatic UTI has been linked to premature labor, hypertension, and anemia during gestation, but these assertions have not been proved. On the other hand, an
increased incidence of occult urinary tract pathology is present in these gravidas. Therefore, women with bacteriuria during pregnancy may benefit from evaluation of their urinary tract postpartum, especially those in whom the infection is resistant to therapy.
B. Symptomatic Bacteriuria. The clinical approach to symptomatic UTI during gestation differs from that for asymptomatic bacteriuria.
1. Acute Pyelonephritis. Pyelonephritis was a cause of maternal death in the preantibiotic era, and 3% of pregnant patients in a more recently reported series developed septic shock. At one time, symptomatic UTIs complicated almost 2% of all gestations, but prenatal screening combined with rapid treatment of asymptomatic bacteriuria has reduced this incidence to approximately 0.5%. The bacteriology of these infections resembles that in asymptomatic patients (predominantly E. coli), and most cases present after midpregnancy. The clinical presentation of pyelonephritis in pregnancy can be dramatic. As noted in the preceding text, the disease caused maternal deaths in the preantibiotic era, and upper UTIs in gravidas are associated with exaggerated effects of endotoxemia, including shock, respiratory distress syndrome, marked renal dysfunction, and hematologic and liver abnormalities. Symptomatic UTIs have also been implicated in the etiology of intrauterine growth restriction, prematurity, congenital anomalies, and fetal demise; however, most studies reporting these associations were not adequately controlled for potential confounders. The treatment of pyelonephritis should be aggressive and is best performed in the hospital.
Most patients with pyelonephritis respond quickly, with defervescence within 48 to 72 hours. Once afebrile for 48 hours, oral therapy may be started and continued to complete 10 to 14 days of treatment. Continuous low-dose suppressive therapy during the remainder of pregnancy is recommended because of the high rate of recurrence. An alternative approach, frequent surveillance for recurrent infection with prompt treatment when significant bacteriuria is identified, has been claimed to be as effective as suppressive therapy.
2. Perirenal abscess and renal abscess formation or carbuncle, although infrequent complications of gestation, should be considered in the differential diagnosis of postpartum fever. It is important to recognize that a high incidence of positive urine cultures occurs in the postpartum period—perhaps 17% to 20% in the first few days after delivery, decreasing to 4% after the third postpartum day. These cases, which resolve spontaneously, may reflect a temporary breakdown in the normal host antibacterial mechanisms in the immediate postpartum period rather than true infection.
3. Antibiotic Use in Pregnancy. The first-choice antibiotic for symptomatic infections changes from decade to decade because of the rapid emergence of resistant strains, thereby resulting in the use of drugs that have not yet withstood the test of time for safety in pregnancy. The physicians continue to recommend starting treatment with cephalosporins, because a significant percentage of community-acquired E. coli infections are resistant to ampicillin. For routine cystitis, nitrofurantoin is often effective and is acceptable during pregnancy.
The physician should also be aware of problems specific to the use of antibiotics in obstetrics and anticipate the potential fetal toxicity of agents that cross the placental barrier. (Information concerning drug safety during pregnancy is listed in the Physicians’ Desk Reference, which is updated annually.) In brief, sulfa drugs should not be used near term, because they may precipitate kernicterus in the newborn. The anti-folic acid activity of trimethoprim has been associated with anomalies such as cleft palate in animals, and this combination drug should also be avoided, at least before midpregnancy.
Aminoglycosides such as gentamicin may be used in pregnancy. Fluoroquinolones cross the placenta and should be avoided if possible. Tetracyclines are contraindicated because they deposit in fetal bones and teeth and may cause severe reactions in the mother, including hepatic failure. Nitrofurantoin is contraindicated at term because of risk of hemolytic disease in the newborn.
C. Acute Kidney Injury
1. Incidence. Before 1970, the incidence of AKI in pregnancy severe enough to require dialytic therapy was estimated at between 1 in 2,000 and 1 in 5,000 gestations, and it represented a considerable proportion of cases reported in large series. Since then, the number of patients with AKI from obstetric causes has declined markedly, and the incidence is now estimated to be less than 1 in 20,000 pregnancies. This trend, attributed to the liberalization of abortion laws and improvement of prenatal care, has not been shared by the poorer and less industrialized nations. In the developing world, the incidence of AKI in pregnancy has been estimated to be as high as 20% and is a significant cause of fetal and maternal morbidity and mortality.
The frequency distribution of AKI during gestation was bimodal, with one peak early in pregnancy (12 to 18 weeks) comprising most of the cases associated with septic abortion, and a second peak between gestational week 35 and the puerperium, primarily due to preeclampsia, sepsis, and bleeding complications, especially placental abruption.
2. Causes. AKI in pregnancy can be induced by any of the disorders leading to renal failure in the general population, such as acute tubular necrosis (ATN). Early in pregnancy, the most common problems are prerenal disease due to hyperemesis gravidarum, and ATN resulting from a septic abortion. Several different uncommon disorders can lead to AKI later in pregnancy. Mild to moderately severe preeclampsia is not usually associated with renal failure, because renal function is generally maintained in the normal or near-normal range for a nonpregnant woman. A variant of preeclampsia, the
Hemolysis,
Elevated
Liver
Enzymes, and
Low
Platelet count (HELLP) syndrome (see
Section VI.B), may be associated with significant renal dysfunction, especially if not treated promptly.
a. Thrombotic Microangiopathy (TMA). TMA is characterized by fibrin and platelet aggregates in the microvasculature, particularly in the kidney and the brain. Histologic features include endothelial cell swelling, accumulation of protein in the endothelial cell layer, and sometimes splitting of the glomerular basement membrane.
TMA affecting primarily the kidney is termed hemolytic uremic syndrome (HUS), whereas TMA characterized by profound thrombocytopenia and neurologic disturbances is called thrombotic thrombocytopenic purpura (TTP). TTP is caused by an acquired or inherited disorder of a metalloproteinase ADAMTS13 that cleaves ultralarge multimers of von Willebrand factor, whereas HUS is caused by dysregulation and uncontrolled activation of the complement system.
An important and difficult differential diagnosis is that of AKI in late pregnancy in association with microangiopathic hemolytic anemia and thrombocytopenia. Pregnancy is considered to be a risk factor for TTP/HUS. However, whether the pathogenesis of these disorders in pregnancy is similar to that in nonpregnant individuals is unclear. TTP/HUS is rare in pregnancy, and must be distinguished from the HELLP variant of preeclampsia, a much more common condition. The distinction of these syndromes is important for therapeutic and prognostic reasons, but considerable overlap exists in their clinical and laboratory features. Features that may be helpful in making the diagnosis include timing of onset and the pattern of laboratory abnormalities, which in TTP may include decreased levels of a von Willebrand cleaving protease. Preeclampsia typically develops in the third trimester, with only a few cases developing in the postpartum period, usually within a few days of delivery. TTP usually occurs antepartum, with many cases developing in the second trimester, as well as the third. HUS is usually a postpartum disease. Symptoms may begin antepartum, but most cases are diagnosed postpartum.
Preeclampsia is much more common than TTP/HUS, and it is usually preceded by hypertension and proteinuria. Renal failure is unusual even with severe cases, unless significant bleeding or hemodynamic instability, or marked disseminated intravascular coagulation (DIC) occurs. In some cases, preeclampsia develops in the immediate postpartum period, and when thrombocytopenia is severe, it may be indistinguishable from HUS. However, preeclampsia spontaneously recovers, whereas HUS only infrequently improves.
In contrast to TTP/HUS, preeclampsia may be associated with mild DIC and prolongation of prothrombin and partial thromboplastin time. Another laboratory feature of preeclampsia/HELLP syndrome that is not usually associated with TTP/HUS is marked elevations in liver enzymes. The presence of fever is more consistent with a diagnosis of TTP than preeclampsia or HUS. The main distinctive features of HUS are its tendency to occur in the postpartum period and the severity of the associated renal failure. Treatment of preeclampsia/HELLP syndrome is delivery and supportive care. More aggressive treatment is rarely indicated. Treatment of TTP/HUS includes plasma infusion or exchange and other modalities used in nonpregnant patients with these disorders, although clinical trials of these modalities in pregnancy have not been performed.
b. Renal Cortical Necrosis. Renal cortical necrosis (RCN) occurs in 1.5% to 2% of all causes of AKI in developed countries and in 3% to 7% of all causes of AKI in developing countries. The primary
inciting events for RCN are obstetric complications (septic abortions, abruptio placenta, and DIC). Affected patients typically present with oliguria or anuria, hematuria, and flank pain. Ultrasonography or computed tomographic scanning may demonstrate hypoechoic or hypodense areas in the renal cortex. Most patients require chronic dialysis, but 20% to 40% have partial recovery of renal function.
c. Acute Pyelonephritis. Some pregnant women may develop AKI in association with pyelonephritis.