Kathleen Sarmiento and Andrew Kitcher
Pregnancy causes dynamic physiologic changes in multiple organ systems including the lungs. These changes can adversely impact preexisting pulmonary disease and increase the likelihood of developing new disorders. Moreover, the normal diagnostic and therapeutic tools of the pulmonologist may be limited in the pregnant patient due to fetal safety concerns.
Pulmonary physiologic changes of pregnancy include increases in (a) the level of the diaphragm (3–4 cm); (b) the anterior-posterior and transverse diameters of the chest (2 cm); and (c) the subcostal angle (68°–103°). These changes take place earlier than can be accounted for by the enlarging uterus itself. Progesterone, estrogen, prostaglandin, corticosteroid, and cyclic nucleotide levels rise during the course of pregnancy. While the multiple functional consequences of these alterations are not clear, increased progesterone is thought to be responsible for the hyperventilation observed during pregnancy. Elevated estrogen levels and capillary engorgement from mucosal edema and hyperemia frequently cause symptoms of rhinitis.
Pulmonary function tests reflect the mechanical changes of pregnancy: diaphragmatic elevation causes a decrease in functional residual capacity (FRC) of 10% to 30%, which is associated with an 8% to 20% fall in expiratory reserve volume and a 7% to 25% fall in residual volume. Flow rates and total lung capacity (TLC) are typically normal throughout most of pregnancy. At term, patients may experience a slight drop in TLC, which may be more pronounced in obese patients. Forced vital capacity (FVC) may increase slightly (4%) after 14 to 16 weeks gestation. The increase tends to be higher in multiparous women than in primigravid women, which suggests that the pregnancy-associated increase in FVC persists following delivery. Diaphragmatic and inspiratory muscle strength are preserved, and inspiratory capacity increases 5% to 10%. Minute ventilation (VE) increases 20% to 50% compared to nonpregnant values, which is primarily attributable to a 30% to 50% increase in tidal volume. Consequently, the resting Paco2 drops to 27 to 34 mmHg, with compensatory increased renal excretion of bicarbonate and fall in serum bicarbonate to 18 to 22 mEq/L to maintain normal pH. The decline in Paco2 leads to a rise in Pao2. DLCO decreases after the first trimester. It increases appropriately with exercise, but it does not increase in the supine position as it does in normal nonpregnant individuals. This results in a significant reduction in Pao2 of 10 mmHg in the supine position in late pregnancy.
Dyspnea is a common complaint in healthy pregnant women and may affect 60% to 70% of gravid women in late pregnancy (>30 weeks gestation). Dyspnea, however, must be evaluated carefully to distinguish more serious conditions from the dyspnea that occurs physiologically during pregnancy. Although VE and chemosensitivity are both increased, the sensation of dyspnea is not due to a difference in progesterone levels, which are similar between dyspneic and nondyspneic pregnant women. Dyspnea usually improves near term, which suggests that the mechanical effect of the gravid uterus itself is not responsible. It appears instead to be related to an increased awareness of the drive to breathe.
Pregnant women suffer from respiratory diseases more than their age-matched, nonpregnant counterparts. Pregnancy does not increase the risk of bacterial pneumonia itself, but it does increase the risk of pneumonia complications, including respiratory failure requiring mechanical ventilation, empyema, bacteremia, and preterm delivery. Community acquired pneumonia is predominantly due to organisms such as Streptoccocus pneumonia, Haemophilus influenza, and Mycoplasma pneumonia, just as it is in nonpregnant patients. Viral pneumonia is a serious concern in pregnancy, as reflected by the increased mortality of pregnant women (up to 50%) in the influenza pandemic of 1918, as well as the increased morbidity and mortality noted with the more recent epidemic of H1N1 influenza in 2009. Influenza vaccination using the inactivated killed virus is recommended for nearly all pregnant women. It is safe for the fetus and effective in stimulating an immunologic response in the mother. Pregnancy itself is not currently an indication for pneumococcal vaccination, unless there are other recognized indications for receiving it. Varicella pneumonia is also associated with increased mortality in pregnant women compared to nonpregnant adults. Assessment of varicella immunity by history or by IgG titers is recommended prior to pregnancy. If it is indicated, varicella vaccination can be administered 1 to 3 months before pregnancy or in the postpartum period. Disseminated Coccidioides infection complicates 1/5,000 pregnancies in the southwestern United States. Neither tuberculosis nor fungal pneumonias are particularly associated with or influenced by the course of pregnancy. The major implication for pregnancy is that it limits the therapeutic options in tuberculosis and fungal pneumonias due to teratogenic effects of medications. Finally, aspiration pneumonitis due to the increased intra-abdominal pressure and the relaxing effect of progesterone on the esophageal sphincter is also a recognized cause of morbidity and mortality in pregnant women.
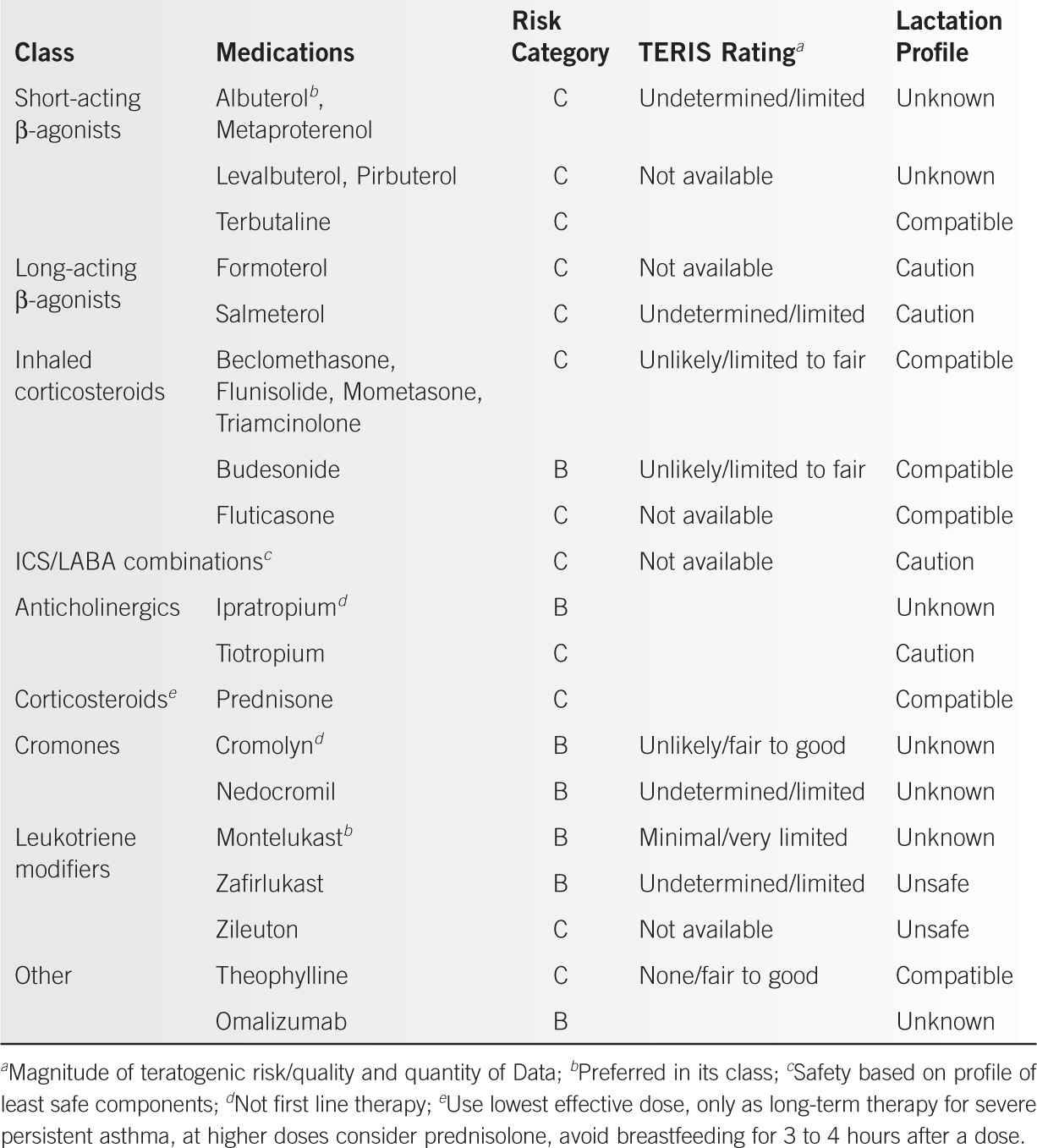
Asthma affects up to 8% of pregnant women and can have a variable course during pregnancy. In a review of 2,186 pregnant women with asthma, 39% experienced no change in their disease during pregnancy, 29% improved, 30% worsened, and 2% were undefined. Asthma, especially severe asthma, is associated with worse pregnancy outcomes, including increased risk of preeclampsia, preterm birth, intrauterine growth restriction, and perinatal death. Most medications used to treat asthma (Table 29-1) are considered safe, but individual drug profiles should be considered when selecting individual therapies. It is clear, however, that untreated asthma has a more deleterious effect on the outcome of pregnancy than the judicious use of these drugs. Known triggers should be avoided, and counseling on smoking cessation and second-hand smoke avoidance should be provided.
Infiltrative lung diseases are rare in women of reproductive age, but they can be related to connective tissue disorders, pulmonary vasculitis, sarcoidosis, lymphangioleiomyomatosis (LAM), idiopathic interstitial pneumonias, eosinophilic pneumonias, drug-induced lung disease, and other rare conditions. Pleural effusions, infiltrates, and acute respiratory distress syndrome (ARDS) have been reported to occur following administration of drugs used in ovarian hyperstimulation. The role of sex hormones in LAM remains controversial, since pregnancy is believed to accelerate disease progression due to increased estrogen levels. Pulmonary complications of LAM during pregnancy include pneumothorax, preterm birth, chylous effusion, and decline in lung function. Sarcoidosis tends to improve or remain unchanged during pregnancy. In general, the risk of pulmonary complications related to pregnancy increases with progressive impairment of baseline pulmonary function. Women with infiltrative lung disease should be counseled prior to conception about the risks of pregnancy. Successful maternal and fetal outcomes are possible with careful planning and a multidisciplinary approach.
Asthma/COPD Medications |
Cystic fibrosis (CF) reduces female fertility through a variety of mechanisms, but as care has improved patients are surviving longer and pregnancy has become increasingly common. Up to 4% of female CF patients of childbearing age are pregnant at any given time. Prepregnancy FEV1 and BMI are important predictors of maternal and fetal outcomes, with FEV1 less than 60% and BMI less than 20 kg/m2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



