Fig. 16.1
Magnetic guided capsule endoscopy (MGCE) equipment
Capsule Maneuverability
The patient lies in the magnetic guidance equipment, with a stable stomach position allowing maximal force for navigation of the capsule. The capsule can be moved with five independent mechanical degrees of freedom: two rotational and three translational (i.e., in three dimensions) (Fig. 16.2). It can be tilted (equivalent to the large steering-wheel movements of an endoscope tip) and it can be rotated (equivalent to the small steering-wheel movements). The tilting command allows the position of the capsule at a fixed point to be oriented. The MGCE can be navigated at a water surface in the stomach or can be made to dive to the bottom of the stomach (Fig. 16.3). In close-up, a clear magnified view of the mucosal pattern is seen because of refraction by the water and the fixed-focus imaging. When the capsule is lying on the stomach wall, it can be made to crawl, and if the capsule is blocked between gastric folds it can be dislodged by being made to “jump” (Video 16.1).
Fig. 16.2
Technical maneuverability
Fig. 16.3
Overall drawing of magnetic guided capsule endoscopy
Imaging System
As with the small bowel capsule, the patient is equipped with multiple antennas in order to record the images from the capsule. The MGCE capsule is 31 mm long and 11 mm in diameter, weighs 2.7 g and has two image sensors. The images are visualized and recorded at 4 frames/s. Standard imaging is done in real time. The images from both sensors are displayed simultaneously on a dual-monitor panel with one screen for each sensor.
MGCE Navigation
The practitioner stands in front of the dual monitors that show the images from both sensors and that display the possible capsule maneuvers and settings (forward, backward, rotating, diving, tilting, jumping). The physician responsible for guiding the device chooses which screen should be the “active” one for directing the capsule, and controls the motion of the capsule by means of two joysticks (Video 16.2).
Operator Learning Curve and Initial Pilot Study
Initially the operators gained in vitro experience in using the technology. The use of plastic “stomachs” with labeled areas or of pig stomachs allowed them to understand how the basic handling worked and to become familiar with the technical capability of the guided video capsule. This stage also provided information about the effectiveness of low level magnetic field guidance and its limitations as well as safety for patients. This stage was completed using simulation software as the practitioners were not familiar with joystick handling.
During the first month of the trial, 26 patients had been included in a pilot study that achieved 24 complete examinations of patients with conventional gastroscopy followed by capsule examinations. The capsule operators were aware of the gastroscopy findings and tried to identify the known lesions using the capsule. Initially, because of the unfamiliar appearance of the uninflated stomach, it was difficult to identify some structures, such as the closed cardia, for example. The operators also had to learn how to navigate through the human stomach, how to deal with gastric contractions and how to get rid of mucus that was stuck on the capsule sensors.
Studies Protocol
Clinical Protocol
Gastric examination with the MGCE was carried out using the following protocol. After overnight fasting, patients drank 500 ml of clear water at room temperature. One hour later, they drank another 400 ml of clear water at room temperature. Then after light exercise for approximately 15 min, in order to obtain a clean stomach, patients drank a further 400 ml of clear water near body temperature (35 °C). This was done to create enough space in the stomach for capsule navigation.
At that point, image-receiving antennae were attached to the patient’s body and the patient was settled inside the magnetic guidance system. The patient position on the table was predetermined to allow for optimal gastric imaging and maximal magnetic force for capsule navigation. Capsule imaging was initiated and the patient ingested the capsule in a sitting position before lying down in the guidance system when the capsule had reached the stomach by esophageal gravity and esophageal motility.
MGCE Examination
At the beginning of the examination the position of the patient was left lateral; this was then changed to supine and finally right lateral. When it was difficult to move or navigate the capsule in a particular position, the patient was moved into another position. If necessary, additional water was ingested during the examination to create optimal conditions, as the MGCE requires an air–water interface for guidance. The visualization of the gastric surface in the antrum, body, and fundus, and identification of the two well-known landmarks of the cardia and pylorus were checked by the examiners. High definition gastroscopy under propofol sedation was considered as the “gold standard.”
Evaluation of Outcomes and Data Analysis
The overall evaluations of stomach visualization, including all stomach areas, were documented immediately on a report sheet by the operator (Fig. 16.4). The examiner assessed these subjectively. Examination time and abnormal findings were also recorded.
Fig. 16.4
Data collection chart
The main outcome parameters were percentage of patients in whom there was complete visualization of the gastric surface in the antrum, body, and fundus, and identification of the cardia and pylorus. Further parameters were examination time, and the percentage of abnormal findings seen on gastroscopy that were reproducible by capsule endoscopy and vice versa.
Guided Capsule Data
Three Clinical Studies Have Been Performed
First Study
Twenty-four patients and 29 volunteers were included in order to assess the feasibility of a clinical trial comparing conventional gastroscopy and MGCE. Maneuverability of the two sensors’ video capsule was obtained with water interface in the human stomach and a low level magnetic guidance equipment [7].
Second Study
Seventy-one patients were enrolled for the comparative blinded study and examinations were completed in 61 patients (39 men, 22 women; mean age 52.7 years, range 21–75). The capsule was swallowed and water ingested (overall volume 1,300 ml as described in the protocol) without problem in all but two patients. A few patients (n = 5) needed to drink additional water at body temperature to keep the stomach distended. No technical defect occurred and we were able to analyze complete comparative examinations in 61 patients. No premedication was given or felt to be necessary for any patient. On follow-up, one patient had temporary abdominal pain, which subsided spontaneously and has not recurred. In another patient, left lower quadrant pain was diagnosed with recurrent sigmoid diverticulitis [8].
As mentioned, in close-up view, the mucosal pattern could be seen clearly as it was magnified because of refraction by the water and the fixed-focus imaging (Fig. 16.5). When the capsule was lodged between folds on the gastric wall, we could navigate the capsule using the jumping and floating functions. Impaired visualization caused by gastric mucus or remaining debris in the water could be overcome by turning the patient or in a few cases by further ingestion of water.


Fig. 16.5
Detailed aspect of abnormal gastric mucosa
Figures 16.5, 16.6, and 16.7 show various gastric images obtained by capsule navigation. Visualization of the gastric pylorus, antrum, body, fundus, and cardia was felt to be complete in 88.5 %, 86.9 %, 93.4 %, 85.2 %, and 88.5 % of patients, respectively (Fig. 16.8). Incomplete visualization was due to resistant mucus in 7 cases, excessive gastric motility in 2 cases, early pyloric passage of the capsule in 4 cases, and incomplete distension of gastric walls in 2. Capsule examination was achieved in a mean total examination time of 17.4 min (range 9.9–26.4). Capsule endoscopy examination time became shorter with increasing skill at navigation but also as new knowledge was gained such as subsequent visualization of the lesser curve or closed cardia.

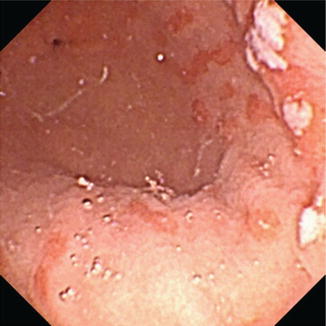

Fig. 16.6
Panoramic view of lesser curve with pylorus (left) and cardia (right)
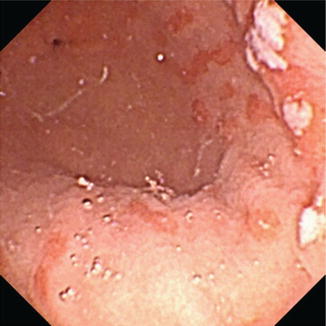
Fig. 16.7
Multiple antral ulcerations
Fig. 16.8
Gastric visualization with overall results, and results related to patient position
A total of 108 pathological findings were detected. Of these, 63 were identified by both conventional gastroscopy and capsule endoscopy: these included 44 cases of diffuse inflammation or erosion, 8 polyps, 3 ulcers (Figs. 16.5 and 16.7), 4 cases of atrophy, 2 cases of antral metaplasia, 1 case of external compression, and 1 case of fundic varices. Gastroscopy detected 14 additional lesions not identified at capsule endoscopy: 2 polyps, 1 case of inflammation, 2 angiodysplasias, 2 ulcers, 2 cases of atrophy, 1 case of important bile reflux, 2 cases of hypertrophic folds, and 2 of antral metaplasia. On the other hand, 31 lesions were detected only by capsule endoscopy and missed by conventional endoscopy: 11 polyps, 10 cases of inflammation, 1 angiodysplasia, 5 ulcers, 1 metaplasia, 2 bleeding lesions, and 1 hiatal hernia.
Third Study
The latter was blinded and randomized [10]: 215 patients were initially included, but 25 had to be excluded due to subsequent refusal for study participation (n = 14), capsule impaction in the esophagus during scanning time (n = 3), technical problems (n = 5), protocol violation (n = 2), and inability to swallow the capsule (n = 1). The remaining 189 patients (105 males, 84 females, mean age 53.0 ± 13.7 years) with an indication for upper GI endoscopy such as upper abdominal pain and/or anemia were included into the study. Twenty-three major lesions were found in 21 patients and included 2 adenocarcinomas (tumor sizes 1.2 and 10 cm, both located in the gastric body), 4 submucosal lesions (size/location 1.5 cm, 0.8 cm in the gastric body, 0.9 cm in the cardia and 1.0 cm in the antrum), 9 gastric ulcers (mean size 0.8 cm, [0.5–1.5 cm], location: cardia n = 2, fundus n = 1, antrum n = 6), 3 single hyperplastic polyps with a maximum size of 5 mm (location: fundus n = 2, pylorus n = 1), and 5 focal angiodysplasia (location: antrum = 2, gastric body n = 2, cardia n = 1). Two patients were found to have 2 lesions (both cases with 1 ulcer and 1 hyperplastic polyp each). Minor lesions were marked inflammatory changes with erosions (n = 165), multiple fundic gland polyps (n = 55), gastric atrophy (n = 16), and miscellaneous (n = 7) (Table 16.1).
Table 16.1




Accuracy values of capsule gastroscopy compared with gastroscopy as the final gold standard for the diagnosis of major lesions on a per-patient (n = 21) and per-lesion (n = 23) basis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








