Testicular Cancer
Testicular cancers are rare overall, yet they are the most common solid tumor of young adult males. There are approximately 8,400 new cases annually, with 380 deaths in the United States. Primarily because of effective cisplatin-based chemotherapy, they have become the most curable of all cancers. Germ cell tumors (GCTs) account for 90% to 95% of all primary testicular neoplasms. No clear etiologic or genetic factors have been defined; however, four risk factors have been established: cryptorchidism, family history of testicular cancer, a personal history of testicular cancer, and intratubular germ cell neoplasia (ITGCN), i.e., carcinoma in situ. Ten percent of patients with GCT have a prior history of an undescended testis, 50% of which were intra-abdominal. Testis cancers will be bilateral in 2% of cases, either concurrent or in succession. A finding of microlithiasis on ultrasound in the contralateral testis of a man with a history of GCT is associated with an increased risk of ITGCN in that testis. However, the significance of microlithasis in the absence of a history of GCT is unclear.
PATHOLOGY
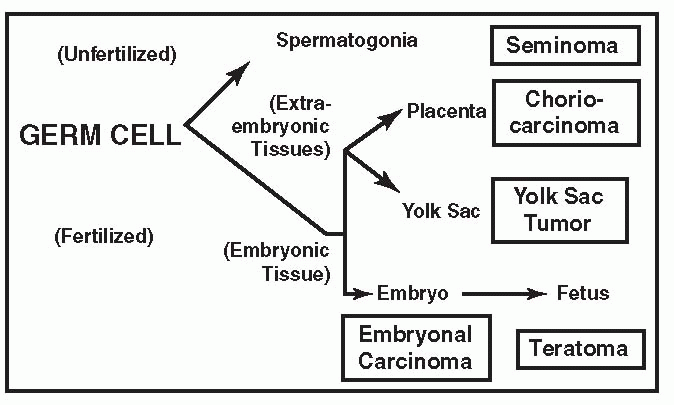
Testis tumors are broadly classified as either seminomas or nonseminomas (NSGCT) and arise from ITGCN. NSGCT include embryonal carcinoma, yolk sac tumors, choriocarcinoma, and teratocarcinoma and generally occur as combinations of mixed GCT. Except for seminoma, there is generally a rapid growth rate, with doubling times of 10 to 30 days.
CLASSIFICATION OF HISTOLOGIC TYPES
Sixty percent of GCTs are of a single cell type, whereas 40% will be mixed. GCT types tend to parallel their normal developmental counterparts as illustrated below.
|
Single Cell Type (60%)
▪ Seminomas (35%)
Seminomas tend to grow in sheets of cells at a slower rate than other GCTs. At presentation 75% will be confined to the testis, 15% will involve regional lymphatics, and 10% will have already spread to distant lymph nodes or viscera. Overall survival is 85%, with >90% survival when the tumor is confined to the testis. The tumor is very radiosensitive. Human chorionic gonadotropin (hCG) is produced by 5% to 10%, but no pure seminoma produces α-fetoprotein (AFP). An elevated AFP excludes the diagnosis of pure seminoma.
Three Subtypes
Classic seminoma (85%)
Anaplastic seminoma (10%)—generally considered a more aggressive tumor with greater metastatic potential
Spermatocytic seminoma (1%)—do not arise from ITGCN, are generally considered benign, and are cured with orchiectomy alone.
▪ Embryonal Carcinoma (20%)
Embryonal carcinoma is a grayish-white fleshy tumor, often with extensive hemorrhage and necrosis. It produces both hCG and AFP.
▪ Teratomas (5%)
Teratomas contain derivatives of all three cell layers: ectoderm (squamous epithelium or neuronal tissue), endoderm (gastrointestinal or respiratory tissue), and mesoderm (bone, cartilage, or muscle). They appear as clear or mucinous cystic areas
interspersed with solid tissue, including bone, muscle, or cartilage. Immature and more mature varieties are differentiated. They have a somewhat less malignant potential. Pure teratomas do not produce hCG and are resistant to chemotherapy.
interspersed with solid tissue, including bone, muscle, or cartilage. Immature and more mature varieties are differentiated. They have a somewhat less malignant potential. Pure teratomas do not produce hCG and are resistant to chemotherapy.
▪ Choriocarcinomas (<1%)
Choriocarcinomas are highly malignant and appear as small grayish-white tumors with central areas of hemorrhage. Both syncytiotrophoblasts and cytotrophoblasts must be demonstrated histologically to make the diagnosis. High titers of hCG are always present. Pure forms do not produce AFP. They often metastasize early via hematogenous routes.
▪ Yolk Sac Tumor (<1%)
Also known as endodermal sinus tumor or orchioblastoma, this tumor occurs in a pure form primarily in children, whereas in adults it can frequently occur in combination with other histologic types. It is the most common testicular neoplasm in infants and children. AFP is produced in high titers.
Mixed Cell Types (40%)
▪ Teratocarcinoma (20%)
Teratocarcinoma is a combination of teratoma and embryonal carcinoma. It is the most frequent mixed cell type and usually produces AFP and/or hCG.
▪ Other Combinations (20%)
In mixed cell tumors, the prognosis becomes that of the most malignant element. Combinations with seminomas are treated as nonseminomatous tumors.
METASTASES
More than half of patients with NSGCT and 15% of pure seminomas present with metastatic disease.
Local Metastases
Local metastatic spread is generally predictable and progresses in a systematic pattern to the regional lymphatics at the level of the renal hilum. Left-sided drainage is primarily to the paraaortic and preaortic areas at the level of L2 (left to right crossover has not
been reported). Right-sided drainage is primarily to the interaortocaval, precaval, and preaortic areas at the level of L2 (right to left crossover is common). Retrograde spread to ipsilateral common and external iliac nodes can occur with advanced disease.
been reported). Right-sided drainage is primarily to the interaortocaval, precaval, and preaortic areas at the level of L2 (right to left crossover is common). Retrograde spread to ipsilateral common and external iliac nodes can occur with advanced disease.
Distant Metastases
Distant metastatic spread is most commonly hematogenous to the lungs, liver, brain, bones, and kidney.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree