Fig. 9.1
The long stem of endo-GIA allows to easily staple the splenic hilum by using only one hand
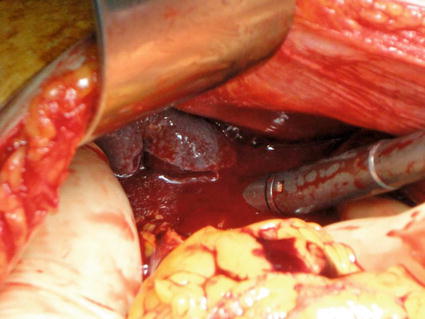
Fig. 9.2
Endo-GIA stapling the splenic hilum, while the left hand of the operating surgeon is holding the spleen, encircling the organ, and protecting the surrounding structures from the staple line
9.5.8 Role of Laparoscopy and Other Minimally Invasive Surgical Procedures
Minimally invasive surgery up to now has a limited role in trauma setting. When the indication for splenectomy is hemodynamic instability, laparoscopy and pneumoperitoneum are strongly contraindicated. In selected cases (stable patients with presumable isolated splenic injuries and evidence of ongoing bleeding despite multiple blood transfusions, after failed or ineffective angioembolization, and in presence of appropriate laparoscopic skills of the operating surgeon as well as of the possibility of a quick conversion to open procedure), a minimally invasive approach can be considered, keeping in mind the limitations of laparoscopic exploration of intra-abdominal organs for blunt and penetrating abdominal trauma. The best indication for laparoscopy is for a diagnostic purpose in case of a penetrating stab wound in the left upper quadrant with suspicion of diaphragmatic tear. Control of bleeding from the splenic surface with the use of hemostatic agents and gauze compression is easy and feasible laparoscopically. Splenorrhaphy and partial splenectomy are technically demanding procedures and should not be attempted in trauma. Small series of successful laparoscopic treatment of isolated blunt splenic injuries with either mesh wrapping or total splenectomy have been reported [25]. When attempting a laparoscopic splenectomy, the anterior approach with patient in supine position is strongly advisable in case of need of immediate conversion to open surgery. The use of 45 or 60 mm endo-stapler with vascular reloads, in hands of experienced surgeons with laparoscopic skills and in case of stable patients, showed to be able to obtain an effective division of hilar and short gastric vessels and achieve a rapid splenectomy [26].
Hand-assisted laparoscopic technique [27] may be a safe alternative to both open and totally laparoscopic splenectomy.
Single-incision laparoscopic emergency splenectomy has been occasionally reported [28]. The case reported is of a patient with doubtful hemodynamic stability and transient response to resuscitation, and several criticisms are to be addressed to this approach. In our opinion, single-incision technique in trauma seems to date nothing more than a potentially life-threatening surgery experiment and is not currently justified.
9.6 Drainage
Drainage of the splenic bed is advisable after splenectomy and after trauma laparotomy. Drains may allow early detection of a significantly postoperative bleeding, as well as onset of complications from injuries to the next organs. Particularly, spleen injuries may easily occur combined with lesions involving the tail of the pancreas. Pancreatic injuries assessment may not always be reliable during damage control laparotomy and distal ductal injuries may be evident and detected postoperatively. Preferably, a closed-suction drain should be placed or a soft corrugated drain.
References
1.
Di Saverio S, Moore EE, Tugnoli G, Naidoo N, Ansaloni L, Bonilauri S, Cucchi M, Catena F (2012) Non operative management of liver and spleen traumatic injuries: a giant with clay feet. World J Emerg Surg 7(1):3. doi:10.1186/1749-7922-7-3 PubMedCentralPubMedCrossRef
2.
3.
4.
5.
Peitzman AB, Richardson JD (2010) Review surgical treatment of injuries to the solid abdominal organs: a 50-year perspective from the Journal of Trauma. J Trauma 69(5):1011–1021PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







