Background
Nephrolithiasis occurs with an estimated overall prevalence of 5.2% and there is evidence that stone disease is on the rise [1]. However, many stones in the kidney go undetected because they cause no symptoms or obstruction. Conversely, ureteral stones rarely remain silent, and they have greater potential for causing pain and obstruction. As such, ureteral stones that fail to pass spontaneously require surgical intervention. Although the introduction of medical expulsive therapy (MET, the use of pharmacological agents to promote spontaneous stone passage) has changed the natural history of ureteral stone disease [2], not all ureteral stones respond to MET. Indications for surgical intervention to remove ureteral calculi include stones that are unlikely or fail to pass spontaneously with or without MET, stones that cause unremitting pain regardless of the likelihood of spontaneous passage, stones associated with persistent, high-grade obstruction, stones in patients with an anatomically or functionally solitary kidney or in those with renal insufficiency or stones in patients for whom their occupation or circumstances mandate prompt resolution (i.e. pilots, frequent travelers, etc.).
Once the decision has been made to intervene surgically for a patient with a ureteral stone, treatment options include shock-wave lithotripspy, ureteroscopy, percutaneous antegrade ureteroscopy and open or laparoscopic ureterolithotomy. Although special cirumstances may dictate the application of percutaneous antegrade ureteroscopy or ureterolithotomy (large, impacted stones, stones in patients with urinary diversions or stones that fail less invasive approaches), the two most widely practiced treatment modalities for ureteral stones are shock-wave lithotripsy (SWL) and ureteroscopy (URS). Both are associated with high success rates and low morbidity. However, the optimal treatment for ureteral stones remains controversial because of passionate advocates on both sides of the controversy. Proponents of SWL cite the noninvasiveness, high patient satisfaction and ease of treatment, while URS advocates favor the short operative times, high success rates and short time interval to become stone free. This chapter weighs the evidence in favor of SWL or URS for the treatment of ureteral stones, and also explores some of the nuances of each treatment that have evidence-based support.
Clinical question 24.1
What is the optimal surgical management for proximal, middle, and distal ureteral calculi (SWL versus URS)?
The optimal treatment modality for ureteral calculi depends on the size, location and composition of the stone, as well as the availability of equipment and expertise of the practitioner. For example, cystine stones respond poorly to SWL; consequently, URS is the preferred treatment for cystine ureteral calculi [3]. Likewise, proximal ureteral stones in a male patient may be difficult to access with a semi-rigid ureteroscope; therefore, practitioners without access to a flexible ureteroscope might not choose URS for the treatment of a proximal ureteral calculus in a male patient. Extenuating circumstances aside, however, the optimal treatment modality for noncystine, nonuric acid stones in patients with normal ureteral anatomy who are otherwise appropriate candidates for either treatment modality will be considered. Of note, however, stone size and location are important variables that affect treatment outcomes for both URS and SWL.
Literature search
A search of the Medline database was performed using the terms “ureteral calculi,” “shock-wave lithotripsy,” “ureteroscopy” and “randomized, controlled trials (RCTs).” The search was limited to the English-language literature published between 1948 and 2008 and focused primarily on RCTs comparing SWL and URS.
The evidence
Despite extensive literature reporting outcomes of single-institution series of SWL or URS for the treatment of patients with ureteral calculi, as well as retrospective series comparing the two treatment modalities, only five RCTs have directly compared SWL and URS. While three RCTs focused exclusively on patients with distal ureteral calculi, only a single trial each addressed patients with proximal ureteral calculi and middle/distal ureteral stones (Table 24.1).
Table 24.1 Randomized controlled trials of URS versus SWL for ureteral calculi
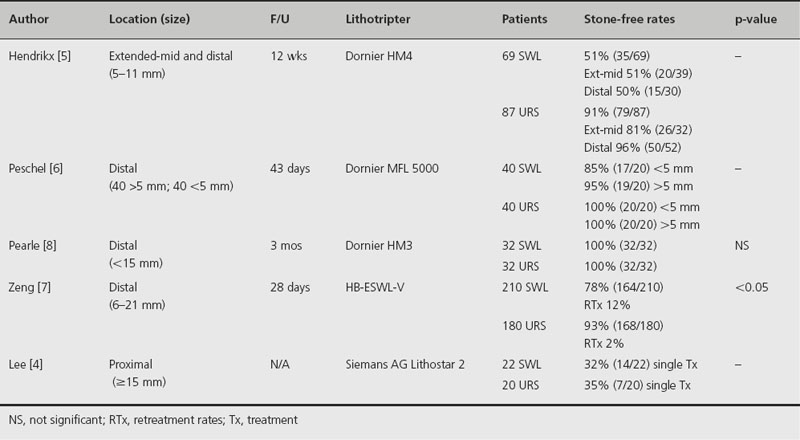
Lee and colleagues randomized 42 patients with large (> 15 mm) proximal ureteral calculi to undergo SWL (N 22) or URS (N 20) [4]. Single-procedure stone-free rates for both SWL and URS were poor, at 32% and 35%, respectively, Complication rates were higher in the URS group (70%) than in the SWL group (9%). Among the URS complications were five ureteral perforations and one ureteral stricture, perhaps as a result of using a semi-rigid ureteroscope. Hospital stay (1.8 versus 4.7 days), visual analog pain scores (1.86 versus 4.35) and patient satisfaction scores (4.12 versus 3.86) all favored SWL over URS, although only length of stay reached statistical significance. Of note, the degree of hydronephrosis correlated negatively with SWL success (p = 0.005). The authors concluded that in the absence of hydronephrosis, both SWL and URS were reasonable therapies for large proximal ureteral stones. However, with the use of current small, flexible ureteroscopes, it is likely that the outcomes would be substantially different, since ureteral perforation, inaccessible stone and retrograde stone migration accounted for the majority of URS failures. Such factors are now routinely overcome with the use of a flexible ureteroscope.
Hendrikx and associates randomized patients with extended-middle and distal ureteral calculi to SWL (N 69) or URS (N 87) [5]. Overall, URS was associated with higher stone-free and lower retreatment rates than SWL (91% and 9%, respectively, for URS versus 51% and 45%, respectively, for SWL). This held true when outcomes were stratified by stone location: stone-free rates for URS and SWL were 81% versus 51%, respectively, for extended-middle ureteral calculi and 96% versus 50%, respectively, for distal ureteral calculi. On the other hand, complication rates and hospital length of stay favored SWL (4.3% and 2.2 days for SWL versus 25.2% and 4.4 days for URS). Although stone-free and retreatment rates strongly favored URS, the lower complication rate and shorter length of stay make SWL a reasonable alternative, particularly for smaller stones.
A total of three RCTs compared SWL and URS for the management of distal ureteral calculi. Peschel and colleagues randomized 80 patients with distal ureteral stones that failed to pass to SWL (N 40) or URS (N 40) [6]. Although stone-free rates were high in both groups (90% for SWL versus 100% for URS), the authors recommended URS over SWL for distal ureteral calculi because the time to become stone free was shorter in the URS group (1.8 days) compared with the SWL group (10 days).
Zeng and co-workers also favored URS for the treatment of distal ureteral calculi based on their RCT comparing 180 patients treated by URS to 210 patients treated with SWL [7]. The stone-free rate was higher for URS than SWL (93% versus 78%, respectively, p < 0.05), and the retreatment rate was fivefold higher for SWL than URS (11.9% versus 2.2%, retrospectively, p < 0.05).
In contrast, Pearle and colleagues, in a multicenter study, randomized 64 patients with distal ureteral calculi to URS or SWL using an HM3 lithotripter (N 32 for each group) [8]. Stone-free rates were 100% in both groups, but secondary outcomes, including operating time (p < 0.05), outpatient procedure rate and patient satisfaction, favored SWL. As such, although SWL was more costly than URS at their institution, the authors recommended HM3 SWL over ureteroscopy since it was equally efficacious, more efficient, and less morbid.
Using these five RCTs, Nabi and colleagues performed a meta-analysis using stone-free rate, retreatment rate, need for auxiliary procedures, efficiency quotient, length of stay, complications, and patient satisfaction as endpoints [9]. Their analysis revealed lower stone-free rates in the SWL arm compared to the URS arm (RR 0.84, 95% confidence interval (CI) 0.70–0.98, p = 0.03). In addition, the retreatment rate was lower but not significantly so in the URS group (RR 2.28, 95% CI 0.53–14.71, p = 0.23), complication rate was lower in the SWL group (RR 0.45, 95% CI 0.21–0.92, p = 0.03), and hospital length of stay was shorter for SWL treatment (RR –2.10, 95% CI –2.55 to –1.64, p < 0.00001). The authors concluded that URS is associated with a higher stone-free rate, but at a cost of a higher complication rate and a longer length of stay. It should be noted, however, that combining the treatment arms of these studies may be problematic because of the heterogeneity of patient groups (i.e. stone location differs in the studies, one study included only patients with > 15 mm stones, lithotripters were different in each study). Consequently, conclusions should be interpreted with caution.
Perhaps a more applicable analysis comparing SWL and URS for the treatment of ureteral calculi can be gleaned from the 2007 American Urological Association (AUA)/European Association of Urology (EAU) Clinical Guidelines for the Management of Ureteral Calculi [10,11]. These guidelines were derived from analysis of 348 articles published between 1996 and 2006, of which 244 contained extractable data suitable for inclusion in the meta-analysis. Despite the lack of a large number of RCTs, this analysis is less susceptible to the inherent biases associated with smaller series and provides the best available evidence to guide surgical treatment decisions for ureteral calculi.
Overall, median stone-free rates for SWL and URS were 82% versus 81%, respectively, for proximal ureteral calculi, 73% versus 86%, respectively, for middle ureteral calculi and 74% versus 94% for distal ureteral calculi (Table 24.2). The more distal the stone, the greater the gap in outcomes between the two treatment modalities, in favor of URS. When stratified by stone size (≤ 10 mm and > 10 mm), stone-free rates were consistently higher for smaller than larger stones: 90% and 68%, 84% and 76%, and 86% and 74%, respectively, for proximal, middle and distal ureteral calculi. URS stone-free rates showed less stringent size dependence: 80% and 79% for proximal ureteral stones, 91% and 78% for middle ureteral stones, and 97% and 93% for distal ureteral stones ≤ 10 and > 10 mm, respectively. Notably, sample size for middle ureteral stones, particularly when stratified by stone size, was small, only 1607 overall for SWL and 1024 for URS. The number of patients treated with SWL for ≤ 10 mm stones was only 44 and those with > 10 mm stones was only 15. Likewise, only 80 and 73 patients comprised the ≤ 10 and > 10 mm URS groups, respectively. Consequently, the stratified data for middle ureteral calculi may not be as reliable as the overall outcome data.
Table 24.2 Stone-free rates for SWL and URS of ureteral calculi from the 2007 Ureteral Stones Clinical Guidelines [7,8]
Tx, treatment
| Stone location/size | Stone-free rate (primary Tx) Median (95% CI) | |
| SWL | URS | |
| Distal ureter | 74% (73–75) | 94% (93–95) |
| < 10 mm | 86% (81–90) | 97% (96–98) |
| > 10 mm | 74% (57–87) | 93% (88–96) |
| Middle ureter | 73% (66–79) | 86% (81–89) |
| < 10 mm | 84% (65–95) | 91% (81–96) |
| > 10 mm | 76% (36–97) | 78% (61–90) |
| Proximal ureter | 82% (79–85) | 81% (77–85) |
| < 10 mm | 90% (85–93) | 80% (73–85) |
| >10 mm | 68% (55–79) | 79% (71–87) |
Taking into account the total number of procedures per patient associated with treatment of the target stone, including the primary procedure (and retreatments), secondary procedures to remove stones and auxiliary, nonstone removal procedures, the number is not remarkably different between SWL and URS (1.62 versus 1.45 for proximal ureteral stones, 1.52 versus 1.2 for middle ureteral stones and 1.37 versus 1.4 for distal ureteral stones, respectively). However, the number of primary procedures (the intended treatment modality) was fewer for URS compared to SWL at all ureteral locations, indicating higher retreatment rates for SWL.
Complication rates were low with both treatment modalities and largely involved infection and obstruction with SWL and infection and ureteral injury/stricture with URS.
Comment
Data derived from individual RCTs and from the 2007 AUA/EUA Ureteral Stone Clinical Guidelines Panel provide Grade 1B evidence that both SWL and URS are reasonable first-line treatment options for ureteral stones not amenable to medical therapy. Success rates are sufficiently high and morbidity rates acceptably low to recommend either treatment modality in most cases. However, URS is associated with higher stone-free rates overall in each ureteral location and for most size stratifications. Furthermore, the number of primary procedures required to achieve a stone-free state is lower for URS than SWL, although the total number of procedures is comparable between the two treatments, likely because stent removal constitutes an additional procedure required for most URS patients. Consequently, a conditional recommendation for URS can be made based on moderate-quality (Grade 2B), evidence, particularly for middle and distal ureteral calculi and for large proximal ureteral calculi.
Clinical question 24.2
Is postprocedure stenting mandatory after ureteroscopy?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








