Table 23.1). When comparing SWL to PCNL for stones < 3 cm in the Lower Pole I study [1], KUB stone-free rate (SFR) is considerably higher for PCNL (95%) than SWL (37%, p < 0.001). These effects were also seen with stones < 1 cm, with SFR for PCNL 100% and SWL at 63%. In fact, this is the only size range where SWL demonstrated SFR > 50%. Quality of life assessments and complications rates are similar for both modalities.
Table 23.1 Surgical outcomes for lower pole kidney stones
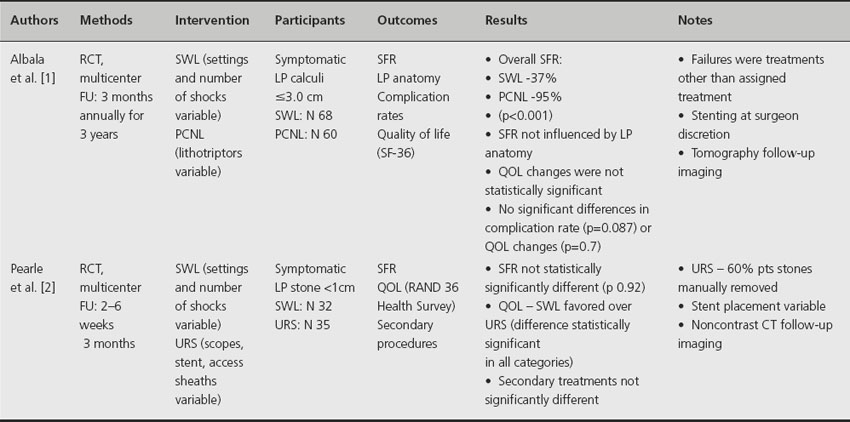
When considering URS for treatment of symptomatic LP stones < 1 cm (Lower Pole II study [2]), no statistically significant difference in computed tomography SFR was seen when compared to SWL. This remains true for ureteroscopy patients who had residual stone fragments manually extracted or left in place to spontaneously pass. In addition, there was no difference in the need for secondary procedures between URS and SWL cohorts. Operative time, hospital stay, and quality of life measures significantly favored patients treated with SWL.
Comment
These multicenter studies demonstrate the lack of standardization in SWL treatment. Variability occurs in the number of shocks and power settings used. Similarly, ureteral stent placement during the procedures was at surgeon discretion and not standardized. The imaging modality used for follow-up must be carefully considered, as patients in the Lower Pole II study underwent noncontrast CT scan [2] while patients in the Lower Pole I study had traditional abdominal imaging [1]. The increased sensitivity of CT compared to other imaging techniques lowers the stone free rates, 20–30% compared to less sensitive ultrasound or abdominal imaging and makes extrapolation to previous studies more difficult. Due to methodological inconsistencies, the quality of evidence is rated a Level B.
In summary, no recommendation can be given regarding small lower pole stone clearance since PCNL, SWL or URS are all reasonable options that lead to acceptable SFR. PCNL provides the highest SFR at the expense of being more invasive and associated with higher postoperative morbidity. Quality of life measures favor the less invasive approach with SWL. Ureteroscopy and laser lithotripsy with or without manual extraction of stone fragments offer a less invasive alternative to PCNL with SFR similar to SWL. Developments in ureteroscope technology are ongoing and may lead to further improvements in SFR.
Clinical question 23.2
What is the effect of adjuvant therapies following surgery for kidney stones?
Literature search
Relevant studies were retrieved from electronic databases including Cochrane Central Register of Controlled Trials, Medline 1996–current, and EMBASE 1980–current. Reference lists were also made from urology and nephrology textbooks, review articles and relevant studies as well as electronic communications seeking information about unpublished or incomplete studies to investigators known to be involved in previous studies. Search terms included all forms and abbreviations of “percussion, diuresis, and inversion (PDI),” “PCNL,” SWL,” “URS,” “lithotripsy,” “nephrolithiasis,” “medical,” “therapy,” “niruri.”
The evidence
Evidence that ureteral stone clearance may be enhanced with medication has been increasing for several years, and indeed multiple RCTs comparing SFR of SWL with or without tamsulosin in the setting of ureteral stones have now been performed [3–8]. Evidence for adjuvant therapy following kidney stone surgery has also demonstrated a benefit in SFR following SWL using adjuvant alpha-blocker therapy, dietary supplements (P. niruru) or mechanical assistance.
Gravina et al. [9] reported the first and most convincing evidence for adjunctive tamsulosin following SWL for kidney stones. Their group studied 130 patients who were randomized to standard therapy alone (control) or in combination with tamsulosin for a total of 12 weeks or until another intervention occurred. They report higher KUB SFR and less pain and analgesic use in the tamsulosin group compared to controls. Subjects with larger diameter renal stones (> 10 mm) benefited most from therapy (81% vs 55%, p = 0.009) compared to stones ≤ 10 mm (75% vs 68%, p > 0.05). Incidence of repeat SWL or ureteroscopy (31% total) was less in the tamsulosin group but not statistically significant (p > 0.05). In this trial, subjects were not randomized to placebo pills, which may have affected self-reporting. Most recently, Naja et al. [10] reported a very similar study design to that of Gravina. Following randomization to SWL only or SWL with tamsulosin, patients had SWL done every 3 weeks for up to 12 weeks or until radiographic success. Success rates after the first, second and third SWL sessions increased more in the tamsulosin arm (53%, 78%, 94%) than in controls (31%, 52%, 75%; p = 0.016, p = 0.004, p = 0.005 respectively), but overall success at study end was similar across groups. In addition to earlier clearance of fragments, subjects on tamsulosin required fewer SWL sessions, had less pain, and developed fewer episodes of steinstrasse than controls.
In 2007, Bhagat et al. [7] reported higher KUB SFR after randomizing patients with both ureteral and renal stones to tamsulosin (96.6%) or placebo (79.3%) after SWL, although analgesic administration between the groups was similar. Subgroup analysis revealed that patients with stones > 10 mm had significantly higher SFR (93.3% vs 58.3%, p = 0.03) compared to stones ≤ 10 mm (100% vs 94.1%, p = 0.35). Methods for analgesic dosing in the study were unclear, and location of stone clearance was not evaluated.
Micali et al. [11] hypothesized that the plant Phyllanthus niruri would improve SFR after SWL in patients with calcium oxalate stones. P. niruri
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








