Surgical Approaches to Crohn’s Disease
Sanda A. Tan
Robert W. Rout
INTRODUCTION
In the past, Crohn’s patients were almost certain to require surgical intervention at some point in their lives. Recent advances in the medical management of Crohn’s disease have reduced and/or delayed surgical intervention in Crohn’s patients, but surgery is still required for over 70% of these people (1). Furthermore, 45% of Crohn’s patients will require repeat surgery within 10 years of their initial surgery (1).
REASONS FOR SURGERY
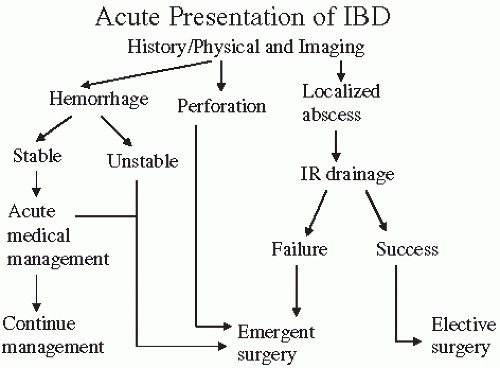
Surgical intervention can be divided into emergent or elective operations, and further, into intra-abdominal or perianal surgical procedures. Emergent surgery is usually indicated for patients who have developed a severe hemorrhage or a bowel perforation. Elective surgery is typically performed for patients suffering from complications such as neoplasia, growth retardation, bowel stricture, and extraintestinal manifestations, for example perianal abscesses or fistula. Refractory disease or intolerance of medical therapy is also a valid indication for elective surgery.
Most frequently, Crohn’s patients present to clinicians complaining of a bowel obstruction (Fig. 10.1). If the evaluation reveals a complete obstruction, an emergent bowel resection is required. However, if the obstruction is partial, patients can initially be managed by conservative approaches such as bowel resection and nasogastric decompression. Small bowel obstructions usually result from strictures of the bowel and eventually will require stricturoplasty or small bowel resection. Large bowel obstructions require further evaluation with colonoscopy to rule out any malignancy, as Crohn’s is a preneoplastic disease and the risk for colon cancer in Crohn’s patients is 4 to 20 times higher than that in a controlled population. The incidence rate of colon cancer in Crohn’s patients is between 1.4% and 1.8% (2).
Similarly, Crohn’s patients with perianal diseases can be divided into those who need emergency surgery and those who have chronic disease requiring elective surgery. Surgical intervention is needed in these patients, either for drainage of the abscess or for the diversion of the fecal stream.
EMERGENCY SURGERY
Bowel perforation and severe hemorrhage are rare, occurring in less than 1% of patients with Crohn’s disease (3), yet these patients require emergent abdominal surgery to stabilize their conditions. A subtotal colectomy with end ileostomy is usually performed initially, while a completion proctectomy is typically performed at a later date once the patient’s clinical condition has improved and if the patient’s condition requires it.
EMERGENT SURGERY FOR PERIANAL DISEASE
Emergent surgery for perianal disease commonly involves abscess drainage by making a small incision over the abscess. A small flexible drain is usually placed
into the abscess to maintain a patent opening until the inflammation subsides. A more definite treatment can be implemented once inflammation has resolved.
into the abscess to maintain a patent opening until the inflammation subsides. A more definite treatment can be implemented once inflammation has resolved.
ELECTIVE SURGERY FOR INTRA-ABDOMINAL DISEASE
Elective abdominal surgery is commonly offered to Crohn’s patients following failure of medical therapy. This is also true for patients on steroid therapy who experience severe side effects from steroids or who have been on steroids for more than 6 months.
Elective surgery is also indicated for patients who have a bowel stricture as a result of Crohn’s disease. Crohn’s patients have a predilection for developing partial bowel obstructions. Additionally, the dilation of the proximal bowel as a result of stricture causes chronic abdominal pain, nausea, and intolerance of oral intake. Some patients, who initially respond to medical management using newer therapies, including antibody-based therapy, begin to develop a resistance to the prescribed medications. In addition, many of these strictures will not respond to medical treatment if fibrosis has developed in the bowel, and patients who have failed medical management under these conditions will require surgical intervention.
Patients with localized abscesses may also be candidates for elective surgery. Those who present in stable condition with a localized abscess can be managed conservatively with abscess drainage and antibiotic therapy. Evaluation for elective surgery can occur at a later time once the abscess has resolved and inflammation has subsided. However, if symptoms persist or if the patient’s condition deteriorates, emergent surgery will be required.
TIMING OF SURGERY
Determining the appropriate time for surgical intervention is one of the more important decisions that will need to be made. Crohn’s disease is a lifelong condition, and many patients will require repeat surgery during their lives. Some patients choose to delay the initial surgery as long as possible, but clinicians have a responsibility to help patients understand that excessive delay carries risk as well.
ENDOSCOPIC DILATION
One of the most pertinent factors that a surgeon must account for before considering performing surgery on a patient with chronic strictures is the assurance that the patient’s nutritional status is optimized prior to the procedure. Specifically, malnourished patients are at an elevated risk for anastomotic breakdown and poor wound healing, particularly during steroid therapy. Nutritional markers, such as albumin, prealbumin, and transferrin, are sometimes useful, but a careful history and physical examination trump even the most sophisticated testing. If the patient’s nutritional status is poor, interventions, which may include intravenous feeding or placement of a feeding tube past the strictured area to supplement with enteric feeding, should be implemented. (Nutrition in inflammatory bowel disease [IBD] is discussed further in Chapter 14.)
If the patient has a short-segment stricture causing the obstruction, endoscopic dilation of the stricture could serve as a bridge until surgical intervention can be safely undertaken. Endoscopic dilation can decompress the obstruction and allow enteric feeding, which will help improve the nutritional status prior to surgery. In select patients, endoscopic dilation may allow surgery to be delayed or even avoided. Data are scant for the role of stent placement (4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree