Surgery for Gastrinoma
E. Christopher Ellison
Gastrinoma, also known as the Zollinger–Ellison syndrome (ZES), is a rare cause of ulcer disease. The incidence is about one case per million per year. The disease usually occurs between the ages of 30 and 70, although cases in children and the elderly have been reported. Sporadic cases dominate, accounting for 75% of all cases. Familial cases occur in 25% of patients and are usually part of the multiple endocrine neoplasia type 1 (MEN1) syndrome. It is very important to establish whether the patient has sporadic gastrinoma or MEN1, as the surgical treatment is different.
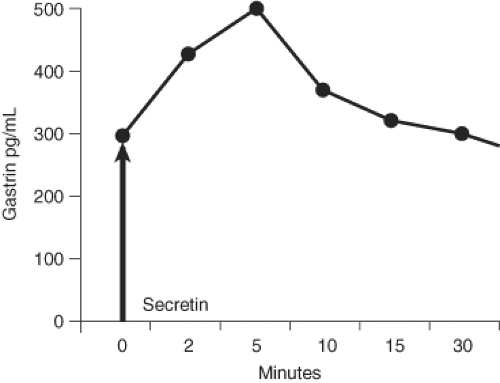
The diagnosis of gastrinoma is suggested by fasting hypergastrinemia off proton pump inhibitors (PPIs) in a patient with refractory ulcer disease, gastroesophageal reflex, or diarrhea. The most common causes of hypergastrinemia are achlorhydria associated with atrophic gastritis and chronic use of PPIs. PPIs induce achlorhydria, and hence, in the absence of negative feedback on the G cells in the gastric antrum, more gastrin is released. To establish that the fasting hypergastrinemia is caused by gastrinoma, it is necessary to check for the presence of gastric acid. If the patient has a gastric pH of 7 off PPIs, then ZES is excluded. If the patient has acid in the gastric aspirate, then a secretin provocative test is indicated. In a patient with gastrinoma, secretin will cause an increase in the gastrin. A positive test is defined as an increase of gastrin greater than 110 pg/mL over the baseline value (Fig. 23.1).
The contemporary surgical approach to gastrinoma is directed at tumor excision, and no gastric procedure is performed. Surgery is recommended only after the diagnosis is clearly established and imaging has localized the tumor.
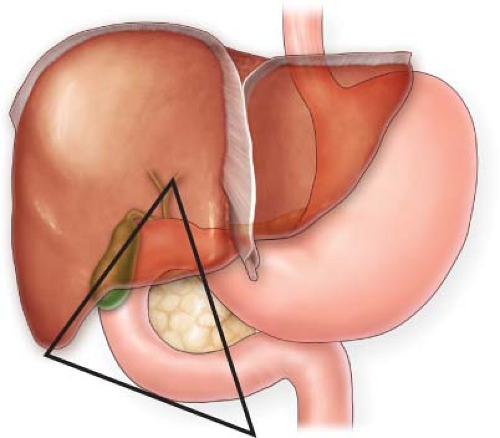
Two-thirds of gastrinomas are located in the gastrinoma triangle shown (Fig. 23.2). This applies to both sporadic and MEN1 patients. In sporadic gastrinoma, the tumors are located either in the duodenum (about half the cases) or the pancreas (nearly half the cases), or both. Gastrinomas may also occur primarily in lymph nodes. About one half of sporadic patients have tumors in both the duodenum and the pancreas. In those with MEN1, there is a propensity for multiple tumors, and duodenal tumors are found in
nearly all of these patients. The gastrin-producing pancreatic tumors are usually in the head of the pancreas. Although many patients have tumors in the body and tail of the pancreas, most of these are nonfunctional.
nearly all of these patients. The gastrin-producing pancreatic tumors are usually in the head of the pancreas. Although many patients have tumors in the body and tail of the pancreas, most of these are nonfunctional.
Preoperative localization tests should be performed. Somatostatin scintigraphy and CT scan are the initial tests. This may be supplemented with endoscopic ultrasound, MRI, and selective arterial secretin stimulation. In one-third of cases these tests will be negative. Exploration is clearly warranted in patients with positive localization tests. An individualized approach is recommended for those with negative localization tests and for patients with MEN1.
Outline of the Surgical Procedure
The operative procedure is divided into three unique major steps and is based on the principle of the gastrinoma triangle: step 1 is pancreatic exposure and management of pancreatic tumors; step 2 is assessment for and resection of duodenal tumors; and step 3 is sampling of lymph nodes in the gastrinoma triangle.
Step 1: Pancreatic Exposure and Management of Pancreatic Tumors
The operation begins after entering the abdomen through a midline incision and performing a manual exploration. The surgeon next performs a wide Kocher maneuver to fully expose the duodenum and allow palpation of the head of the pancreas. Next is the exposure of the pancreas through the lesser sac. This is followed by bimanual palpation of the pancreas and then by intraoperative ultrasound. Next is local excision of any pancreatic tumors. Pancreatic resection, either distal pancreatectomy or pancreaticoduodenectomy, is sometimes needed depending on the location and size of the tumor and in particular if the pancreatic duct is involved.
Step 2: Assessment for Duodenal Tumors and Resection
Intraoperative esophagogastroduodenoscopy and transillumination of the duodenum may be done to try to localize a duodenal tumor. However, the preferred technique is creation of a longitudinal duodenotomy to permit palpation of the duodenal mucosa. This is the most reliable method to identify duodenal tumors. If a tumor is found then it is removed by either enucleation or a full thickness local resection of the duodenal tumor if it is located in the lateral duodenum.
Step 3: Sampling of Lymph Nodes in the Gastrinoma Triangle
Details of Surgery for Gastrinoma
The operation is usually done as an open procedure; however, with improved preoperative localization a laparoscopic or robotic technique may be suitable for some patients.
Positioning
The patient is placed in the supine position. The left arm is tucked and the right arm is placed on an arm board.
Patient
A peripheral IV is started. Central venous access is used in selected cases. After induction of general endotracheal tube anesthesia, a nasogastric tube and Foley catheter are placed.
Equipment
In addition to a general laparotomy set, the following equipment should be available:
Intraoperative ultrasound transducer (10 MHz) and an ultrasound unit
An endoscopy cart and an adult upper endoscope
A bipolar coagulating device
Incision
A midline incision is made, and the abdomen is manually explored. The round ligament is divided. A self-retaining retractor is placed.
Pancreatic Exposure and Management of Pancreatic Tumors
Kocherization of the Duodenum
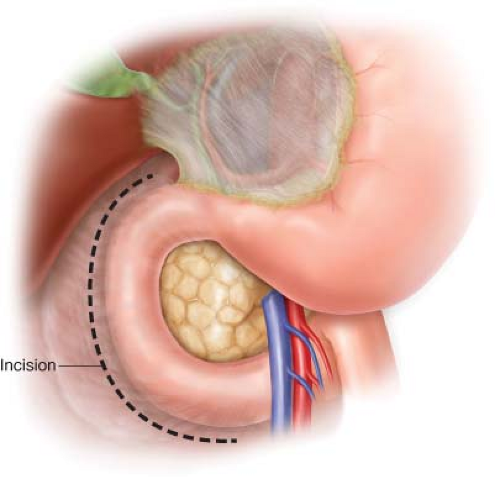
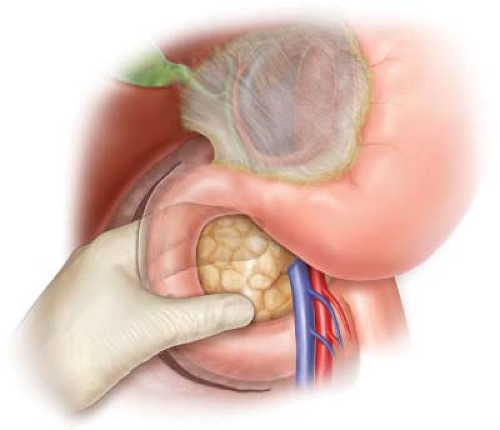
The peritoneum along the second portion of the duodenum is incised sharply. Medial retraction on the duodenum by the assistant facilitates the mobilization. The Kocher maneuver is complete when the left renal vein is seen. The duodenum and head of the pancreas are palpated (Figs. 23.3 and 23.4).
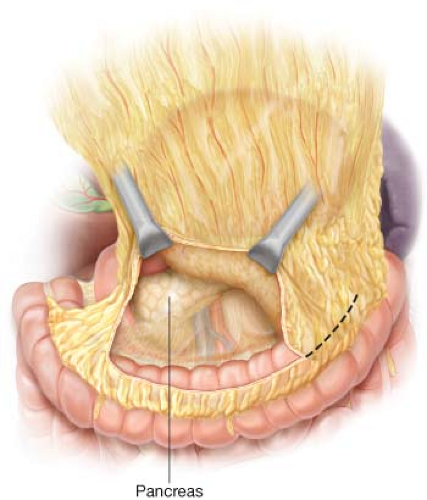
Exposure of the Pancreas
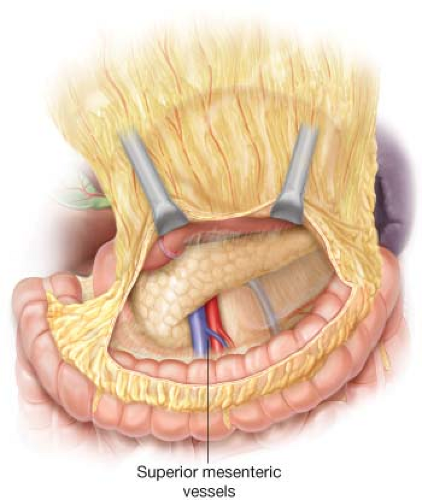
The lesser sac is entered by sharply dividing the omentum from the transverse colon. This is carried widely (Fig. 23.5). The body and tail of the pancreas are exposed. The attachments between the posterior wall of the stomach and the anterior surface of the pancreas are incised with electrocautery. The neck and anterior surface of the head of
the pancreas are exposed by continued dissection of the omentum in order to expose the vascular groove and the anterior portion of the superior mesenteric vein (Fig. 23.6). In some cases to provide enhanced exposure the gastroepiploic vein is ligated with 2-0 silk and divided. Bimanual palpation of the pancreas is performed.
the pancreas are exposed by continued dissection of the omentum in order to expose the vascular groove and the anterior portion of the superior mesenteric vein (Fig. 23.6). In some cases to provide enhanced exposure the gastroepiploic vein is ligated with 2-0 silk and divided. Bimanual palpation of the pancreas is performed.
Ultrasound of the Pancreas
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree