CHAPTER 5 Storage disorders and incontinence
INTRODUCTION
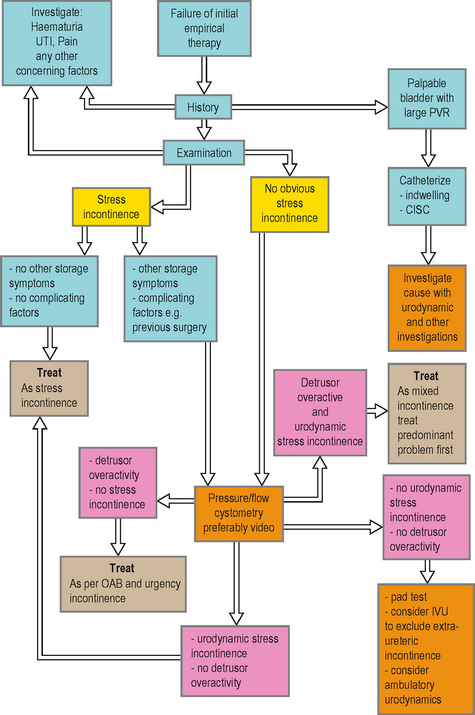
However, many successful treatments are available for these conditions; therefore it is important that sufferers are offered a suitable treatment and frequently urodynamics are required to determine the most appropriate management choice. A simple algorithm for the investigation of incontinence is shown in Figure 5.1.
OVERACTIVE BLADDER SYNDROME AND URGENCY INCONTINENCE
CLINICAL NOTES: PATIENT EVALUATION OF STORAGE DISORDERS AND INCONTINENCE
OAB can be further categorized as:
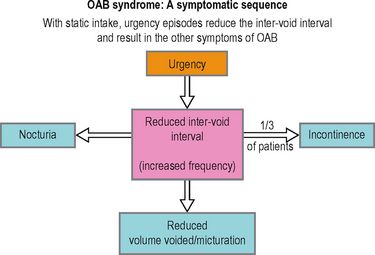
It is believed that the driving force within OAB is the symptom of urgency, defined as ‘the complaint of a sudden compelling desire to pass urine, which is difficult to deter’ (Figure 5.2). Urgency may compel the sufferer to void more frequently than normal and to wake from sleep to void. Increased frequency can also partly be a result of an adaptive or coping mechanism to suppress urgency. If urgency is severe and the patient has little warning or is not able to reach a toilet in time, then urgency incontinence may occur. Approximately 30% of patients with OAB have urgency incontinence, although the prevalence increases significantly in the elderly with multiple co-morbidities.
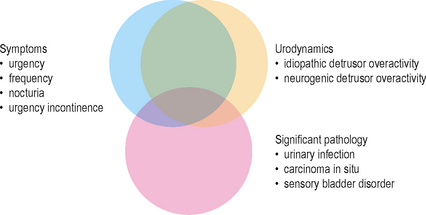
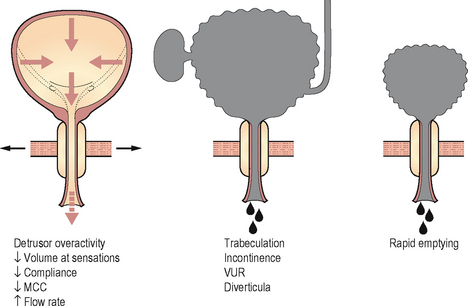
As urgency is frequently associated with detrusor overactivity (DO) during cystometry, it had been previously hypothesized that the pathology was due to dysfunction in the efferent motor innervation of the bladder. However, significant emerging evidence suggests that the dysfunction (or its central nervous system interpretation) is at least partly (if not wholly) due to afferent sensory dysfunction and this would be in concordance with the pivotal symptom of urgency being an essentially sensory symptom (Figure 5.3). Though the majority of OAB and urgency incontinence patients are classified as ‘idiopathic’, a number of clinical causes should be considered:
Management of OAB and urgency incontinence
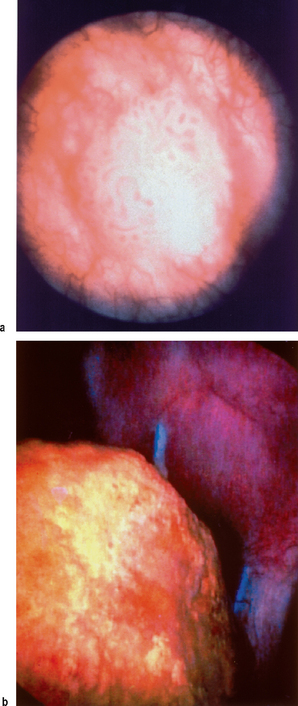
A large number of patients are treated empirically often by their primary care physician. If successfully managed and if important pathologies such as bladder carcinoma (Figure 5.4) and UTI have been excluded then there is often little need for further investigations. Frequently however the patient may have equivocal symptoms or the condition may not respond to initial therapy; in such circumstances the patient should be referred to secondary care for a more detailed evaluation and a greater range of management options. Successful management of OAB requires that the condition is accurately diagnosed and differentiated from other lower urinary disorders such as stress incontinence.
Available and emerging treatment choices include:
 Sacral neuromodulation (mechanism unknown but may act to stimulate the Aδ myelinated fibres, especially at the S3 level. Probably enhances sphincter/pelvic tone and may inhibit the detrusor reflex)
Sacral neuromodulation (mechanism unknown but may act to stimulate the Aδ myelinated fibres, especially at the S3 level. Probably enhances sphincter/pelvic tone and may inhibit the detrusor reflex)Urodynamics in OAB and urgency incontinence
1-hour pad test
Useful in patients strongly suspected of urinary incontinence but who have failed to demonstrate any leakage on other investigations such as video urodynamic pressure/flow studies (Figure 5.5). Approximately 30% of patients with urgency incontinence have a normal pressure/flow study. The test also gives a quantification of the degree of incontinence, as patients are usually inaccurate when asked to quantify the leakage.
Uroflowmetry
Not a particularly useful test in this condition, although may be beneficial in ruling out voiding dysfunction as a cause of the storage symptoms, such as in men with mixed LUTS. Should be performed prior to pressure/flow cystometry to give a more representative indication of the voiding pattern than is possible during invasive cystometry.
Urodynamic findings in OAB and urgency incontinence Table 5.1)
Detrusor overactivity
The characteristic finding of DO during pressure/flow cystometry is shown in Figure 5.6. In patients with a known neurological cause for the lower urinary tract dysfunction this is described as neurogenic detrusor overactivity (NDO; see Chapter 9), whereas when the aetiology is unknown it is described as idiopathic detrusor overactivity (IDO). DO was previously called detrusor instability and NDO was previously called detrusor hyperreflexia.
Table 5.1 Possible findings during urodynamic testing of patients with OAB or urgency incontinence.
| Possible findings during urodynamic testing of patients with OAB or urgency incontinence | |
|---|---|
| Voiding diaries | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|