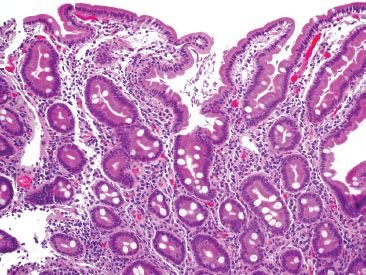
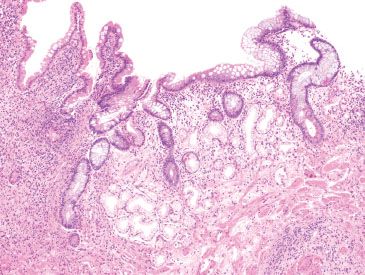
e-Figure 3.1
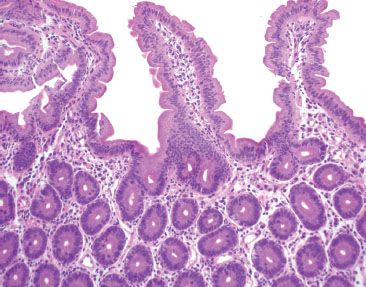
This biopsy was taken from the duodenum. The structure pictured is:
A. A small neuroma, a diagnosis that can be confirmed with a positive S100 protein immunostain.
B. A small neuroma, a diagnosis that can be confirmed with an eosinophilic staining on a PAS stain.
C. A crushed Brunner gland, a diagnosis that can be confirmed with basophilic staining on an Alcian Blue stain.
D. A crushed Brunner gland, a diagnosis that can be confirmed with eosinophilic staining on a PAS stain.
E. A Peyer patch, a diagnosis that can be confirmed with a positive LCA immunostain.
Answer: A crushed Brunner gland, a diagnosis that can be confirmed with eosinophilic staining on a PAS stain (D).
Brunner glands are found the proximal duodenum and stain intensely eosinophilic on PAS stain, but not with Alcian Blue (C). Crush artifact may cause them to be mistaken for neural tumors (A and B), but PAS stain will confirm their phenotype. Peyer patches are lymphoid aggregates found in the terminal ileum (E).
E-QUIZ QUESTION 3 (e-FIG. 3.2)
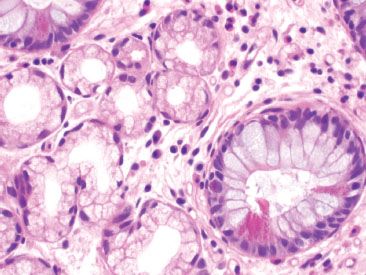
e-Figure 3.2
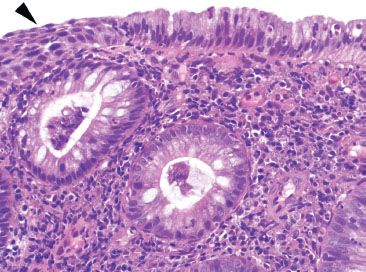
This patient presented with clinically significant diarrhea, nonresponsive to diet modification. The clinical evaluation for celiac disease and pertinent microbiologic studies were negative. Select the best diagnosis for this duodenal biopsy:
A. Autoimmune enteropathy (AIE)
B. Giardiasis
C. Celiac disease
D. Whipple disease with classic histologic features
Answer: Autoimmune enteropathy (AIE) (A).
The biopsy shows a complete lack of goblet cells (Paneth cells were also absent), raising concerns for AIE (A). Antienterocyte and antigoblet cell antibodies were identified and the patient responded to steroid-based therapies, supporting a clinicopathologic diagnosis of AIE. Luminal Giardia forms would be easy to see at low power but are not identified (in addition, the question stem details that microbiologic studies were negative, making Giardia clinically unlikely) (B). The villous architecture is intact and pertinent clinical studies for celiac disease were negative, making Celiac disease unlikely (C). Whipple disease with classic histologic features disease is characterized by villous blunting, lamina propria expansion by numerous foamy macrophages, scattered dilated lacteals, and fat droplets, features that are not present on this biopsy (D).
E-QUIZ QUESTION 4 (e-FIG. 3.3)
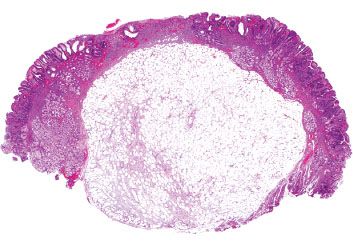
e-Figure 3.3
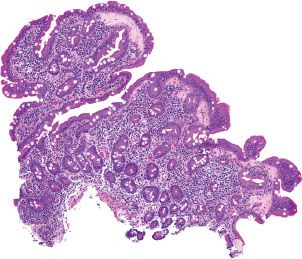
This biopsy was labeled as “pouch” from a patient with an ileal anal-pouch for ulcerative colitis. Which statement best characterizes the findings?
A. This biopsy was taken from the rectal cuff due to the presence of anal squamous mucosa.
B. This biopsy was taken from the rectal cuff due to the presence of squamous metaplasia.
C. This biopsy shows chronic pouchitis due to the presence of squamous metaplasia.
D. This biopsy shows Crohn disease due to the presence acute inflammation adjacent to anal squamous mucosa.
E. This biopsy shows Crohn disease due to the presence of squamous metaplasia.
Answer: This biopsy was taken from the rectal cuff due to the presence of anal squamous mucosa (A).
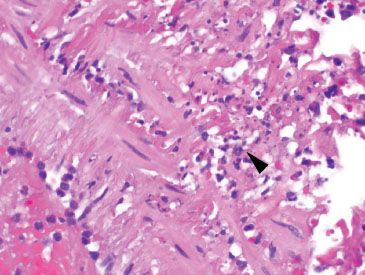
The presence of squamous mucosa (arrowhead) identifies this tissue fragment as adjacent to the anal canal and originating from the rectal cuff. Squamous metaplasia has not been described as a feature of rectal cuffs (B), chronic pouchitis (C), or Crohn disease (E). Although perianal Crohn disease may involve the anal canal and cause acute inflammation in the distal rectum, this diagnosis cannot be established based on the figure presented (D).
E-QUIZ QUESTION 5 (e-FIGS. 3.4 and 3.5)
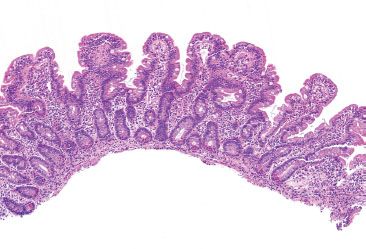
e-Figure 3.4
e-Figure 3.5
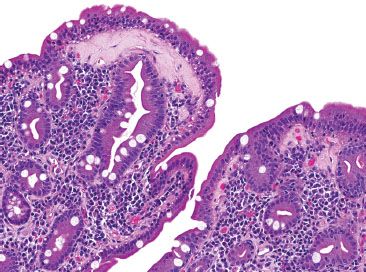
Which of the following entities have been associated with the above finding?
A. Celiac disease
B. Collagenous colitis
C. Lymphocytic gastritis
D. Medication injury
E. All of the above
Answer: All of the above (E).
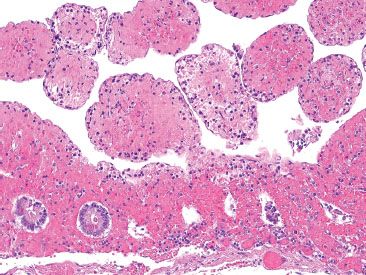
The histologic features shown here include a stripped or detached surface epithelium without crypt architectural changes. The second figure shows a markedly abnormal subepithelial collagen layer. Collagenous enteritis (pictured) has been associated with collagenous gastritis, collagenous colitis, lymphocytic colitis, lymphocytic gastritis, ulcerative jejunitis, and medication injury due to olmesartan.
E-QUIZ QUESTION 6 (e-FIG. 3.6)
e-Figure 3.6
Select the best answer for the above small bowel biopsy:
A. Unremarkable small bowel mucosa
B. Celiac disease
C. Giardiasis
D. Amyloidosis
Answer: Giardiasis (C).
While the low power view of the duodenal mucosa is fairly unremarkable (A), numerous Giardia organisms are seen swirling in the luminal spaces between the villi (C). Giardiasis is one of a host of diagnoses that are difficult to make unless searched for in every case; the background mucosa is essentially unremarkable and offers no clues to the diagnosis. Although this patient was asymptomatic, treatment was required to eradicate the infection and prevent onward transmission. The intact villous architecture and lack of intraepithelial lymphocytosis argue against celiac disease (C). Amyloid deposition is not identified (see the lamina propria vessels on the far left, which have crisp and delicate borders, making a Congo red special stain for amyloid unnecessary).
E-QUIZ QUESTION 7 (e-FIGS. 3.7 and 3.8)
e-Figure 3.7
e-Figure 3.8
The first figure shows a small arterial wall directly subjacent to the area shown in the second figure. Which of the following is a true statement?
A. The first figure shows leukocytoclastic vasculitis and is likely the cause of the ischemia seen in the second figure.
B. The first figure shows angioinvasive fungal organisms and is likely the cause of the ischemia seen in the second figure.
C. The first figure shows karyorrhectic debris, but it is not clear whether this represents vasculitis, since it was found directly adjacent to ischemic enteritis.
D. The first figure shows a fibrin thrombus that caused the ischemia shown in the second figure.
E. The first figure shows E. coli 0157:H7 that caused the hemorrhagic colitis seen in the second figure.
Answer: The first figure shows karyorrhectic debris, but it is not clear whether this represents vasculitis, since it was found directly adjacent to ischemic enteritis (C).
Although inspection for vasculitis in cases of ischemia may yield a diagnostic focus, one must be wary not to overinterpret vascular changes that are directly adjacent to areas of ischemia or ulceration. Given the proximity of the vessel to the ischemic area, it is not possible to confidently diagnose this as leukocytoclastic vasculitis (A). Invasive fungal organisms should appear filamentous and their presence can be confirmed with a GMS stain (B). Fibrin thrombi should be within the lumen of the vessel and not in the wall (D). Enterotoxic microorganisms are not typically visible on biopsy and require microbiologic confirmation (E).
E-QUIZ QUESTION 8 (e-FIG. 3.9)
e-Figure 3.9
This duodenal biopsy was taken from a 54-year-old female with abdominal pain, bloating, and diarrhea. Prior to endoscopy, she demonstrated a negative antitissue transglutaminase antibody (TTG). In addition, she was negative for HLA-DQ2 and DQ8. At the time of biopsy, a duodenal aspirate was obtained for cultures, which subsequently grew >100,000 CFU/mL. After reviewing her biopsy, which of the following statements is most accurate?
A. This woman has celiac disease.
B. This woman has SIBO, and she does not have celiac disease.
C. This woman has SIBO and celiac disease cannot be excluded.
D. This woman has both SIBO and celiac disease.
E. This woman does not have small intestinal bacterial over growth or celiac disease.
Answer: This woman has SIBO, and she does not have celiac disease (B).
The finding of negative HLA-DQ2 or DQ8 haplotypes in this patient essentially excludes celiac disease in this patient (A, C and D). The negative TTG also supports this interpretation. The finding of >100,000 CFU/mL growing from her duodenal aspirate is diagnostic of SIBO SIBO (E). The histologic findings of SIBO include a malabsorption pattern of injury that can mimic celiac disease. The presence of crypt hyperplasia, villous blunting, and intraepithelial lymphocytosis should always be correlated with clinical information.
E-QUIZ QUESTION 9
Titanium pigment is unique to the terminal ileum and is thought to derive from which of the following:
A. Ingested whitening agents in toothpaste
B. Topical titanium–containing sunblock solutions
C. Swallowed gum
D. Chewing pencils
Answer: Ingested whitening agents in toothpaste (A).
Titanium is a finely granular dark-brown to black pigment confined within the cytoplasm of macrophages. It is historically thought to represent a combination of titanium, aluminum, and silicon from ingested whitening agents in toothpaste (A). The other answer choices are distractors (B–D).
E-QUIZ QUESTION 10 (e-FIGS. 3.10 and 3.11)
e-Figure 3.10
e-Figure 3.11
This biopsy was taken from the terminal ileum. Higher magnification of a metaplastic condition is featured in the second figure. What is the significance of the pictured finding in figure 2?
A. This finding is pyloric metaplasia and is diagnostic for Crohn disease when found in the terminal ileum.
B. This finding is pyloric metaplasia and is diagnostic for backwash ileitis from ulcerative colitis when found in the terminal ileum.
C. This finding is pyloric metaplasia and is diagnostic for NSAID-related injury when found in the terminal ileum.
D. This finding is pyloric metaplasia and indicates chronic injury, but is nonspecific for an etiology.
E. This finding is Paneth cell metaplasia and indicates chronic injury, but is nonspecific for an etiology.
Answer: This finding is pyloric metaplasia and indicates chronic injury, but is nonspecific for an etiology (D).
Pyloric metaplasia is a nonspecific finding that indicates chronicity when found in the terminal ileum. The finding may be seen in association with Crohn disease, NSAID-related diaphragm disease, or other chronic inflammatory processes, but is not specific (A, C). Backwash ileitis is frequently a mild acute pattern of injury, and typically lacks features of chronic injury (B). Paneth cells are a normal epithelial constituent of the small bowel, and contain abundant eosinophilic granules (E). Paneth cells are a feature of chronic injury when present in the descending and sigmoid colon and rectum.
E-QUIZ QUESTION 11 (e-FIGS. 3.12 and 3.13)
e-Figure 3.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








