Indication
LESS procedure
Prostate adenocarcinoma
Radical prostatectomy
TCC bladder
Radical cystoprostatectomy
BPH
Simple prostatectomy (STEP)
Reconstruction
Bladder diverticulectomy
Ureteral reimplantation
Vesico-vaginal fistula repair
Sacrocolpopexy
19.3 LESS Prostate Surgery
Simple Prostatectomy
The open simple prostatectomy remains the gold standard in surgical therapy for prostates larger than 80 g [21]. However, there is still the potential for significant morbidity associated with this procedure, including significant hemorrhage. A number of centers have recently reported their experience with single-port transvesical enucleation of the prostate (STEP) as a minimally invasive alternative. For this procedure ports are placed through the bladder, and the prostate adenoma is enucleated. Desai et al. [22] described their experience with 34 cases in 2010. The mean prostate volume estimated by transrectal ultrasonography was 102.5 mL and the mean baseline prostate-specific antigen level was 6.7 ng/mL. A TriPort (Advanced Surgical Concepts, Wicklow, Ireland) multichannel port was placed into the bladder under direct cystoscopic vision, and pneumovesium of 15 mmHg was achieved. The adenoma was then enucleated with electrocautery or ultrasonic shears, by creating a circumferential mucosal incision at the bladder neck. A stay suture (2-0 polyglactin on CT-X needle) was placed through the intravesical adenoma and brought out percutaneously using a Carter-Thomason device, to facilitate retraction. In patients with a small intravesical component (19/34 of patients), enucleation of the distal apical adenoma was done with finger dissection by disconnecting the valve of the TriPort. Mean OR time was 116 min and EBL was 360 mL. There were two conversions to the open procedure. Major complications included one death, which was due to hemorrhage/coagulopathy in a Jehovah’s Witness who refused transfusion. One patient experienced a rectal injury. At 8 months follow-up mean American Urologic Association symptom score was 3, maximum urinary flow rate was 44 ml/s, and post-void residual was 30 mL. No patients developed incontinence. Wang et al. [23] performed the STEP procedure in nine patients with a mean prostate size of 83.8 ± 19.9 mL. Using a similar technique, a TriPort was placed in a preperitoneal fashion into the bladder. Mean OR time was 160.9 ± 30.4 min, and EBL was 418.8 ± 282.76 mL. One case was converted to open prostatectomy because of difficulties with TriPort insertion. At 12 months post procedure, the mean Qmax was 22.7 ± 4.62 mL/s, PVR was 36.1 ± 40.02 mL, and IPSS was 4.1 ± 1.36. Fareed et al. [24] reported their experience with STEP, using the DaVinci surgical robot. Nine patients underwent R-STEP with a GelPort (Applied Medical, Santa Margarita, CA) as the access platform (Fig. 19.1). Robotic instruments consisted of a 5-mm Schertel grasper and harmonic scalpel. Mean gland size was 146.4 mL (83–304 mL) based on trans-rectal ultrasound. Mean OR time was 3.8 h (2.75–4.75), and EBL was 584.4 mL (150–1,200). One patient required conversion to an open prostatectomy, and was excluded from the analysis. Two patients required cystoscopy, fulguration, and clot evacuation post-operatively for clot retention. Additionally one patient developed a DVT which required anti-coagulation, and one patient suffered a peri-operative myocardial infarction, requiring admission to the ICU. At 1 month follow up mean IPSS was 4.83 (2–15), Qmax was 20.1 mL/s (6–36), and PVR was 75.75 m; (0–360). The authors concluded that while R-LESS is technically feasible and effective in treating bladder outlet obstruction, they found a high rate of complications in their study (Table 19.2).
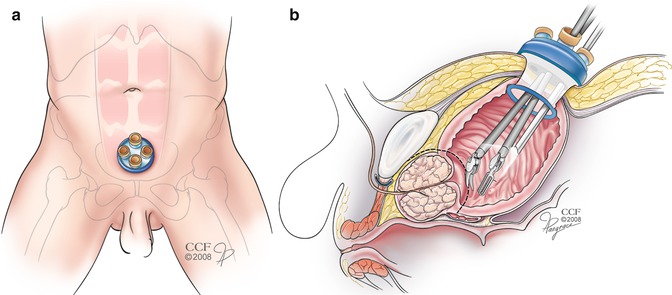
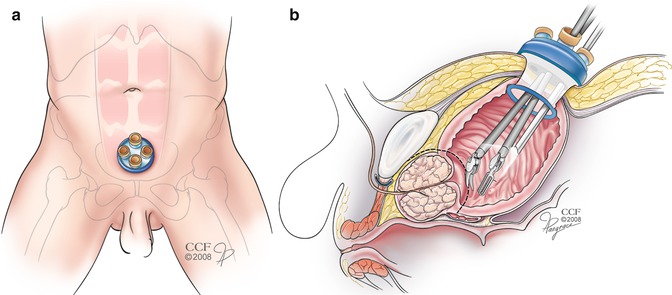
Fig. 19.1
Illustration of R-STEP. (a) Gel-port located in the suprapubic area; (b) 12mm robotic scopeand two 5mm robotic instruments introduced thorugh the Gel-port inserted in tranvesically through the bladder dome. The 30° lens are angled upwords in order to minimize instrument clashing
Table 19.2
LESS transvesical prostate enucleation series
Ref. | # of pts. | Procedure | Prostate volume (mL) | Port | OR time (min) | EBL (mL) | Conversions/extra ports | Complications | IPSS/Qmax (mL/s) |
|---|---|---|---|---|---|---|---|---|---|
Desai et al. [22] | 34 | STEP | 102.5 | TriPort | 116 | 360 | 2 (to open surgery) | 1 death (perioperative hemorrhage) | 3/44 of (8 months) |
1 rectal injury | |||||||||
5 perioperative hemorrhage | |||||||||
1 UTI | |||||||||
Wang et al. [23] | 9 | STEP | 83.8 | TriPort | 160.9 | 418.8 | 1 (to open surgery) | 1 UTI | 4.1/22.7 of (12 months) |
1 urethral stricture | |||||||||
Fareed et al. [24] | 9 | R-STEP | 146.4 | GelPort | 228 | 584.4 | 1 (to open surgery) | 1 MI | 4.83/20.1 of (1 month) |
1 DVT | |||||||||
2 perioperative hemorrhage | |||||||||
Lee et al. [25] | 7 | STEP | 100.8 | Home made | 191.86 | 600 | None | 1 transfusion | 11.43/17.14 of (3 months) |
Radical Prostatectomy
Kaouk et al. first reported a series of conventional LESS radical prostatectomy [3]. Four patients (mean age 63 years, mean BMI 29 kg/m2; mean PSA 5.50 ng/dl; no prior history of pelvic surgery) were selected to have the procedure. All were clinical stage T1c, with a Gleason score 3 + 3 in two, and 3 + 4 in two patients. An open Hassan technique was used to insert a Uni-X™ single access (Pnavel Systems) multichannel port through a 1.8 cm umbilical incision into the peritoneal cavity. Then, a 5 mm Endoeye scope (Olympus) with a flexible tip and articulating graspers (Novare Surgical Systems, Cupertino, CA, USA) were used (Fig. 19.2a). The surgeons reported that these instruments were helpful in providing effective retraction during dissection, but difficulty was noted with applying adequate anterior traction on the seminal vesicles and vas deferens while at the same time retracting the bladder cephalad to gain exposure to the rectum. For this reason apical dissection of the prostate was done first, prior to releasing the vas deferens and seminal vesicles completely. A lymph node dissection was performed in one patient only. Although the 5 mm LigaSure (Valley Lab) was used to take the pedicles, the neurovascular bundles were released with cold scissors. The urethro-vesical anastomosis was completed with interrupted 2-0 Vicryl sutures on SH needles (Fig. 19.2b). The knots were tied externally and advanced into the pelvis with a knot pusher. At the end of the procedure the prostate was delivered by extending the umbilical incision up to 2–3 cm. There were no urine leaks when the anastomosis was tested intraoperatively by filling the bladder with saline. Additionally there were no conversions to either standard laparoscopy, or open prostatectomy. Mean OR time was 4.75 h, and EBL was 287 mL. On follow-up, three patients were continent (using 0 or 1 pad for security). Follow up was too short to determine potency outcomes. One patient developed a recto-urethral fistula, which was treated with a mucosal advancement flap. Two patients had a positive margin but their PSA remained undetectable on short-term follow up. The authors concluded that while LESS radical prostatectomy was technically feasible, there was considerable difficulty with intracorporeal suturing and knot tying. They postulated that application of the robotic platform might overcome the challenges with conventional LESS.
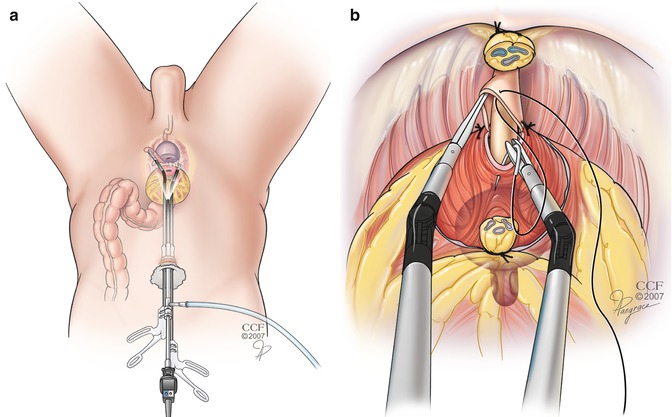
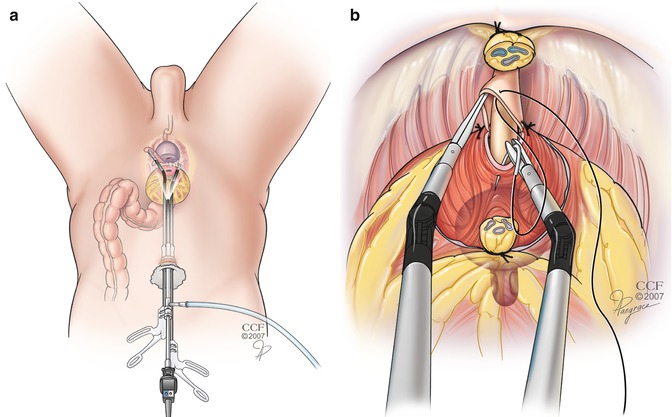
Fig. 19.2
Illustration of LESS radical prostatectomy. (a) Set-up with multichannel port and in-line instruments and scope (b) detail of urethro-vesical anastomosis using articulating instruments
Caceres et al. reported the largest LESS prostatectomy series of 31 patients using the KeyPort multi-channel single site umbilical system (Richard Wolf GmbH, Knittlingen, Germany), in conjunction with a new DuoRotate system (Richard Wolf) [26]. The system incorporates bent instruments with double rotation, and allows for precise movement at the tips of the instruments after alignment of the arms. The majority of patients had intermediate risk disease (45.8 %) according to D’Amico stratification [27]. An additional 3.5 mm port placed in the right iliac fossa was used by the assistant for suction/retraction, and was also used by the primary surgeon during the urethrovesical anastomosis to facilitate suturing. They also used “marionette” sutures to retract the bladder cephalad during dissection of the prostate. The anastomosis was completed with a running barbed polyglyconate suture V-LOC 90 2–0 (Covidien). There were no conversions to standard laparoscopy, or intraoperative complications. Mean OR time was 207 min (120–390) and EBL was 258 mL (200–500). Nerve sparing was performed in ten patients (32.3 %) and a lymph node dissection was done in eight (25.8 %). At 20 weeks post procedure, 33 % were fully continent. With regards to potency, 3/10 of patients who had an athermal nerve sparing procedure had a SHIM score of >21 at 20 weeks. Five patients had a focal positive margin. Two patients experience major complications. One patient had a rectal injury and presented 2 days post-op with peritonitis. He underwent a diverting colostomy. Another patient developed respiratory acidosis due to a prolonged OR time (390 min) and required admission to the intensive care unit post-operatively.
Zhu et al. [28] performed a LESS RP using an extraperitoneal approach in six patients. Mean age was 74.7 years (74–76) and BMI was 23.8 kg/m2 (19.5–32.2). Mean PSA was 8.49 ng/mL (1.53–19.4) and prostate volume was 45.5 ml (27.2–63.3). Three patients were cT2a and the remaining three were cT3a. On TRUS biopsy, two patients had Gleason 6 disease, and four patients had Gleason 7 (3 + 4 = 1 patient, 4 + 3 = 3 patients) Standard laparoscopic instruments were used in conjunction with a QuadPort (Olympus, Tokyo, Japan) and a 0° Olympus EndoEYE 5 mm flexible tip video-laparoscope. The extra-peritoneal space was developed using a balloon device. Nerve-sparing was not performed in this series of patients, and the harmonic scalpel was used to control the prostate pedicles. Mean OR time was 252.5 min (190–305) and EBL was 300 mL (100–500). There were no intraoperative complications or conversions to standard laparoscopy/open surgery. Long-term oncologic outcomes were not presented, but there were no positive margins, and all patients had an undetectable PSA at 1 month. Additionally all six patients were completely continent (0 pads/day) at 12 months post-operatively. Again, like previous studies, the authors reported that LESS RP is feasible, but found intracorporeal suturing during the urethrovesical anastomosis challenging.
A number of groups have reported their experience with R-LESS radical prostatectomy [29, 30], the largest including 20 patients by White et al. [14]. They used a single-site approach, with a SILS port and two 8 mm standard robotic trocars (or one 8 mm and one 5 mm trocar) placed through separate fascial incisions (Fig. 19.3). Standard 8 mm EndoWrist (Intuitive Surgical) monopolar shears and a 5 mm EndoWrist Schertel grasper were used during dissection. The majority of patients were D’Amico low risk (45 %). Mean age was 60.4 years, and mean BMI was 25.4 kg/m2. Because the fourth arm was not used, retraction was accomplished by assistant suction or marionette sutures. Mean OR time was 187.6 min, and EBL was 128.8 mL. There was one conversion to standard robotic prostatectomy because of a large median lobe and need for more effective retraction. Also, two cases required an additional 8 mm port placed outside of the umbilical incision due to issues with triangulation and leakage of gas from the SILS port. There were four positive margins, but no patients experienced biochemical recurrence at 1 year follow up. The authors also reported a trend towards improved urinary continence, with five patients completely pad free over the follow up period. Three patients underwent an interfascial nerve sparing technique, and one had SHIM score of >21 at 3 months post-operatively. Five patients had a leak at the urethrovesical anastomosis on cystogram done 1 week post surgery, and required an additional week of catheterization. One patient experienced urosepsis and was admitted to the ICU 45 days postoperatively, but recovered with intravenous antibiotics. The authors concluded that R-LESS is feasible, and less challenging than conventional LESS. Instrument clashing was virtually eliminated by staggering the robotic trocars, and marionette sutures allowed for effective retraction despite inability to use the fourth arm. Assistant-driven retraction with the suction was also important, and facilitated by placing a 15–30° downward bend, in the distal one third of the instrument (Table 19.3).
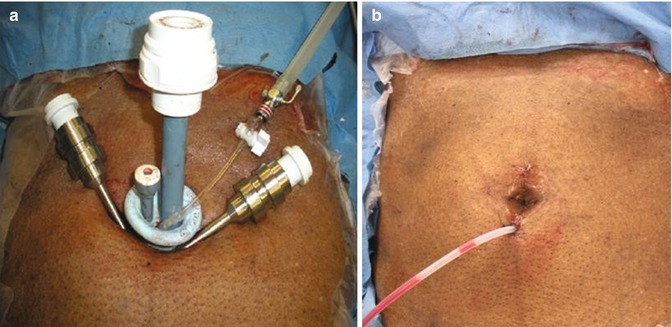
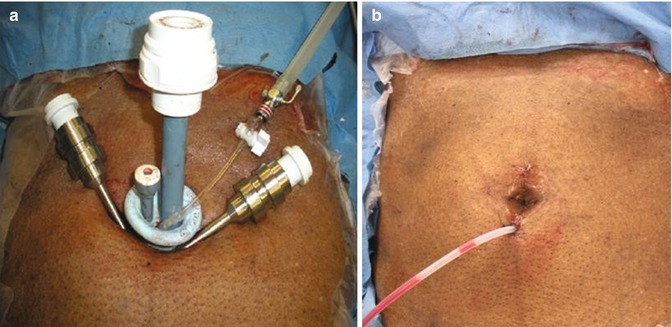
Fig. 19.3
Port configuration for R-LESS radical prostatectomy: (a) SILS port (Covidien) and two 8 mm standard robotic trocars (or one 8 m and one 5 mm trocar) placed through separate fascial incisions; (b) final aspect of umbilical incision (Photos courtesy of Dr. Jihad Kaouk, Cleveland Clinic)
Table 19.3
LESS radical prostatectomy series
Ref. | # of pts. | Procedure | Port | OR time (min) | EBL (mL) | Conversions/extra ports | Complications | Margins | Potency | Continence | PSA (ng/dL) |
|---|---|---|---|---|---|---|---|---|---|---|---|
Kaouk et al. [3] | 4 | LESS RRP | Uni-X | 285 | 287 | None | 1 rectourethral fistula | 2 positive | F/U not sufficient | 3 patients dry (0–1 pads/day) | <0.03 |
Caceres et al. [26] | 31 | LESS RRP | KeyPort | 207 | 258 | None (all cases had 2.5 mm port in RIF) | 1 rectal injury | 5 positive | 3/10 of patients had SHIM>21 (20 weeks) | 33 % continent at 12 weeks | F/U not sufficient |
1 resp. acidosis | |||||||||||
1 transfusion | |||||||||||
1 UTI | |||||||||||
Zhu et al. [28] | 6 | LESS RRP (extraperitoneal) | QuadPort | 252.5 | 300 | None | None reported | All negative | Non-NS procedure | All continent at 12 months (0 pads) | <0.03 (1 month) |
Wen et al. [31] | 6 | LESS RRP | QuadPort/ Home Made | 265 | 230 | None | None reported | All negative | 3/6 of patients had erections (3 months)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





