Fig. 3.1
Sigmoid mesentery being separated from underlying retroperitoneal structures with the left ureter and gonadal vessels in view
Tips for Retraction in SILS
In SILS colectomy, one would need to accustom to the lack of retraction from an assistant. It is often useful to use a laparoscopic Debakey forceps with opened jaws to tent up the sigmoid mesentery. The alternative is to use a laparoscopic fan retractor.
In order to avoid the “chopstick effect,” some of the dissection needs to be performed by the “cross out” (Fig. 3.2).
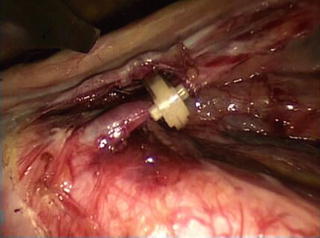
Fig. 3.2
Clipping of the inferior mesenteric artery before dividing
Brunner described the technique of transabdominal sutures, using a straight needle, to retract the sigmoid colon in SILS colectomy [33] (Fig. 3.3).
Leroy utilizes the flexible sigmoidoscopy to aid in the retraction of sigmoid colon, using its tip angulation and endoscope torque. An anvil is also passed transanally into the colon by a flexible introducer, and with the use of an extracorporeal magnet, the sigmoid colon could be lifted up for medial dissection [41].
Ligation of IMA and IMV
After dissecting the sigmoid mesentery from the retroperitoneal structures, the inferior mesenteric artery (IMA) is identified as the tubular structure that tense up the mesentery. It is skeletonized, clipped with either 5 mm Hem-o-lok (Teleflex Medical, USA) or 10 mm Lapro-clip (Covidien, USA) and divided close to its origin (Fig. 3.2). One must distinguish it from the left ureter before dividing it. The mesentery is divided towards further lateral until the inferior mesenteric vein (IMV) is identified. The vein is traced proximally towards the lower border of the pancreas, and clipped and divided. Currently available bipolar devices with the ability to divide vessels up to 7 mm can also be used to control the major vessels. After dividing the inferior mesenteric vessels, the dissection continued further upwards towards the splenic flexure of the colon, separating the mesentery from the pancreas.


Fig. 3.3
Use of transabdominal suture for retraction
Taking Down Splenic Flexure
The lateral peritoneal attachment of the sigmoid colon is incised along the line of Toldt. With the medial to lateral approach, the sigmoid mesentery has already been separated from the underlying retroperitoneal structures, thereby leaving only a thin layer of peritoneum to be incised. Sharp dissection of the peritoneum is continued in the cephalic direction. With the descending colon retracted towards the medial side, its mesentery is separated from the retroperitoneum and the pancreas by blunt dissection. Care should be taken not to exert excessive traction, which may result in splenic laceration. To take down the splenic flexure of colon, one would need to grasp the greater omentum towards the cephalic direction and tension will be created to the colo-omental adhesions by gravity. These adhesions together with the gastrocolic ligament are incised until the lesser sac is entered. The dissection is continued laterally until the line of dissection rendezvous with the one created from lateral dissection. One should remember the dissection is not made between the greater omentum and the spleen. In this way, the chance of splenic laceration is minimized.
Transection of Colon and Performing Colorectal Anastomoses
Once the splenic flexure of the colon is taken down, the lateral peritoneal attachment of sigmoid colon to the pelvis is also divided and the mobilization of the left colon is complete. The double stapling method is used for performing colorectal anastomoses. At the level of distal transection, the mesorectum is divided at the level of transection with cautery or energy devices. The rectum is transected with a laparoscopic linear stapler with an articulating mechanism, e.g., EchelonFlex™ Endopath® 60 mm stapler (Ethicon, USA) and EndoGIA™ with Tri-Staple™ 60 mm stapler (Covidien, USA) (Fig. 3.4). In female patients, the uterus could be slung by transabdominal sutures to facilitate this step (Fig. 3.5).
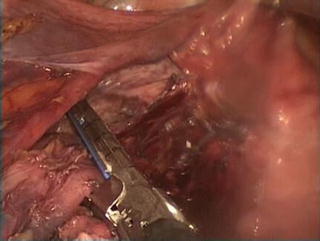

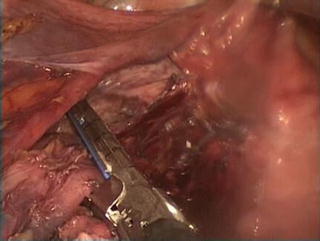
Fig. 3.4
Applying the laparoscopic linear stapler for distal transection

Fig. 3.6
Retrieval of the specimen through the umbilical incision
The application of the transverse stapler across the rectum for transection may be difficult through the umbilical single incision. The authors usually mobilize the rectum adequately so that it can be retract anteriorly towards the abdominal wall. The stapler is placed posterior to the rectum and angulated anteriorly at its tip so that a staple line at right angle to the bowel can be achieved.
The midline wound is used to retrieve the specimen. Many a time, the single port access device is removed and a double-ring wound protector, e.g., Alexiś® wound retraction system (Applied Medical, USA), is inserted to facilitate the retrieval of the specimen (Fig. 3.6). The stump of IMA and IMV together with the left colon is delivered through the wound. The level of proximal transection is chosen. The line of dissection of the mesentery starts from the stump of the pedicle towards the intended level of proximal transection. The mesentery is then divided between ligatures. Care must be taken to preserve the marginal artery of Drummond supplying the part of colon later used to anastomose with the rectum. The proximal transection is then performed with diathermy and the specimen is delivered. Adequate blood supply could be confirmed by bleeding from the transection edge. A purse-string suture is applied, either by hand-sewn or a purse-string instrument, and tied after inserting the anvil of a circular stapler. After hemostasis is ensured, the colon with the anvil secured in it is brought back to the peritoneal cavity. After reinserting the single port access device, pneumoperitoneum is reestablished. The assistant would introduce the circular stapler, e.g., DST Series™ EEA™ 28 mm (Autosuture, Covidien, USA) or CDH29A (Ethicon, USA) transanally towards the rectal stump. Intracorporeal colorectal anastomosis is performed (Fig. 3.7). Before closing and firing of the circular stapler, one would need to ascertain no twisting of the colon. The mesentery of the left colon should be at the posterior position, aligning with the mesorectum. There should be adequate length of the colon without tension on the anastomoses. The final part of the operation includes performing colonoscopy to check for any bleeding from the anastomosis, the color and thus the viability of colon and lastly, to perform an air leak test. The anastomosis is submerged in the pelvis filled with saline and the bowel is occluded proximally. The rectum is inflated with air endoscopically. Air bubbles persistently emerging from the pelvis would indicate a leak. Both proximal and distal doughnut from the circular stapler should be complete ring. The distal doughnut should be sent for section as the distal resection margin. A final check on the hemostasis is performed, any residual fluid is aspirated and any remaining laparoscopic gauze is removed. Unless otherwise indicated, it is not a routine to place a drain. The wound is closed by opposing the fascia with interrupted sutures. 0.5 % Chirocaine® is used to infiltrate the wound for postoperative pain control. The skin is closed with subcuticular absorbable sutures (Fig. 3.8).

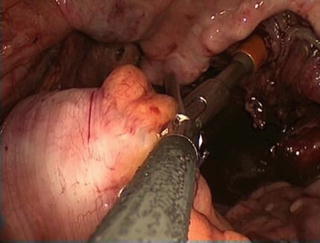


Fig. 3.5
Using transabdominal sutures to sling the uterus
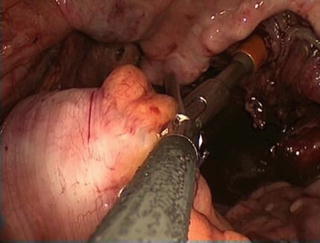
Fig. 3.7
Performing intracorporeal anastomosis with the circular stapler

Fig. 3.8
Final incision
Lateral to Medial Approach
The lateral to medial approach could be used as an alternative when there are difficulties or poor progress in establishing an avascular plane between the sigmoid mesocolon and the retroperitoneum by the medial to lateral approach. This is a laparoscopic version of the open approach used to mobilize the sigmoid colon. With gentle traction of the sigmoid colon towards medial direction, the lateral peritoneal attachment is incised alone the white line of Toldt. The avascular plane between mesocolic and retroperitoneal fat is followed and separated by both sharp and blunt dissection. The gonadal vessels and the left ureter, which is more medial, are seen. In thin patients, the left common iliac artery is seen as a pulsating tubular structure. All these structures are to be protected. The dissection is continued further upwards. Splenic flexure is taken down in a similar fashion as the medial to lateral approach. The lateral dissection is then extended down to the pelvis. With the sigmoid colon fully medialized and the important retroperitoneal structures protected, the colon is retracted towards the upward and lateral direction. The peritoneum lining the sigmoid mesocolon is then incised medial to the inferior mesenteric artery. The inferior mesenteric artery and vein are ligated and divided. The transection of colon and intracorporeal anastomosis could then be performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








