Single-Incision Laparoscopic Bariatric Surgery
Sunil Sharma
Alan A. Saber
There is a growing trend toward surgical techniques that facilitate less abdominal trauma. This has the potential to complement and expand the benefits of traditional laparoscopic surgery that stems from less abdominal trauma, less postoperative pain, analgesia requirement, hospital stay, less scarring, and better cosmetic outcome.
With the emergence of natural orifice translumenal endoscopic surgery, more attention has been directed toward the single-incision transumbilical laparoscopic approach for minimally invasive surgery. Single-incision surgery brings together the cosmetic advantages of natural orifice translumenal endoscopic surgery and the familiarity of conventional laparoscopic surgery. As instruments become more flexible, along with availability of multichannel ports, the single-incision approach could represent the future direction of minimally invasive surgery.
The predetermined exclusion criteria for the single-incision bariatric approach includes patients who have undergone previous bariatric surgery, upper abdominal open surgery, or upper abdominal ventral hernia mesh repair and super-morbid obesity.
As with any form of bariatric surgery the essential prerequisites before surgery are to attend a weight loss surgery information seminar, psychological evaluation and clearance, nutrition evaluation, medical evaluation, workup and clearance. We have found that by instructing all of our bariatric patients to consume a high-protein low-calorie liquid diet for 2 to 4 weeks before their scheduled surgery enables the liver to shrink, making its retraction more feasible. All patients should be involved in the decision-making process. They should receive a detailed description of the risks and benefits of all bariatric procedures.
Deep vein thrombosis prophylaxis is achieved using anticoagulation, compression stockings, and lower extremity sequential compression devices. Preoperative intravenous antibiotic prophylaxis is administrated before making the skin incision.
Operative Strategy and Technical Considerations
The feasibility of the single-incision approach is enhanced when tailored according to each patient’s body habitus. In patients with a relatively low BMI, peripheral obesity, a small liver, and a short umbilicus–xiphoid distance, we proceed with transumbilical single incision. In addition to the cosmetic advantages of a hidden intraumbilical single incision, the umbilicus provides a safe zone for abdominal access while minimizing the torque effect of an obese patient’s thick abdominal wall. In contrast, for patients with a much greater BMI, central obesity, a large liver, and a long umbilicus–subxiphoid distance, we advance the single incision toward the epigastric area.
TAP Block
The single-incision approach involves a single incision as opposed to multiple tiny incisions, scattered all over the abdomen in a standard laparoscopic operation. We take advantage of this situation by selectively blocking the nerves supplying the periumbilical area. This is achieved by ultrasound-guided transversus abdominis plane (TAP) block. When the block is performed correctly, the single incision stays relatively pain-free, thereby reducing the requirement for narcotic analgesics and enabling for a faster recovery and earlier discharge from the hospital.
Anatomy
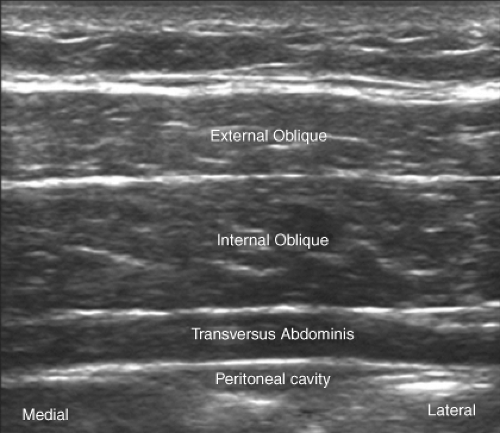
The anterior abdominal wall (skin, muscles, parietal peritoneum) is innervated by the anterior rami of the lower six thoracic nerves (T7 to T12) and the first lumbar nerve (L1). Terminal branches of these somatic nerves course through the lateral abdominal wall within a plane between the internal oblique and transversus abdominis muscles. This intermuscular plane is called the TAP. Injection of local anesthetic within the TAP can therefore potentially provide unilateral analgesia to the skin, muscles, and parietal peritoneum of the anterior abdominal wall (Fig. 33.1).
Block Technique
Scanning Technique
Ultrasound-guided TAP block:
Using ultrasound guidance, it is easy to identify the fascial plane between the internal oblique and the transversus abdominis muscles.
The patient is placed in a supine position exposing the costal margin and the iliac crest.
A linear, high-frequency transducer is recommended for this block.
After preparing the skin and transducer in sterile fashion, the transducer is placed in an axial (transverse) plane, above the iliac crest, and at the anterior axillary line.
The three muscular layers of the abdominal wall are identified as follows: the external oblique (most superficial), the internal oblique (most prominent), and the transversus abdominis muscles below it (Fig. 33.2). The terminal branches of the anterior rami are expected to lie within the TAP between internal oblique and the transverse abdominis muscles above the iliac crest. The peritoneal cavity lies deep to the transversus abdominis muscle layer and may be identified by the peristaltic movements of bowel loops.
Needle Insertion
A 120- to 150-mm 22G short beveled block needle is inserted in-plane with the transducer, in an anterior-posterior direction Alternatively, a spinal needle may be used and connected to the syringe via short extension tubing.
The needle is inserted some distance away from the transducer. This permits a shallower needle trajectory and improves needle shaft and tip visualization.
In obese patients with protuberant abdomen, manual retraction of the abdominal wall by an assistant is a useful maneuver to facilitate needle insertion.
Accurate placement of the needle tip may be facilitated by “hydrodissection” of the appropriate plane. This is achieved by injection of a small amount of fluid (1 to 2 mL of saline or local anesthetic).
It is important to deposit local anesthetic deep to the fascial layer that separates the internal oblique and the transversus abdominis muscles.
Local Anesthetic Injection
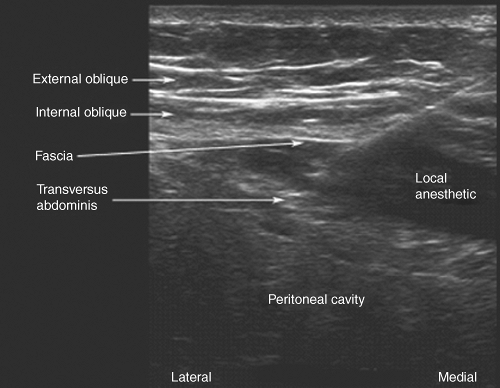
A total of 20 to 30 mL of local anesthetic (e.g., ropivacaine 0.5% to 0.75%) is injected into this plane on each side (Fig. 33.3).
Correct needle tip position and deposition of local anesthetic is indicated by the appearance of a hypoechoic fluid pocket immediately deep to the hyperechoic fascial plane below the internal oblique and above the transversus abdominis. If the needle tip is intramuscular, a pattern of fluid spread consistent with intramuscular fluid injection will be seen.
During local anesthetic injection, it is advisable to scan the abdomen cephalad and caudad to determine the extent of longitudinal spread. Medial and lateral scanning will determine the extent of horizontal spread.
Technical and Physical Challenges in Single-Incision Approach
Lost Triangulation and Trocar Placement Strategy
Achieving adequate triangulation is a basic principle of traditional laparoscopic surgery.
Trocars could be directed from multiple points of entry, guiding instruments toward the target organ, where adequate manipulation could be achieved. (Fig. 33.4A)
Operating through a single incision with only rigid instruments would be challenging, because the surgeon would either implement a coaxial positioning of instruments (Fig. 33.4B) or a “crossing” arrangement (Fig. 33.4C). In the coaxial technique, both instruments emerge through the umbilicus and are parallel to one another; thus, controlling both instruments outside the abdomen would pose a challenge, because the surgeon’s hands would be at such close proximity. On the other hand, when rigid instruments are crossing, there would be a considerably more comfortable range of movement on the outside; however, on the inside, the left hand controls the right instrument, and vice versa, posing a challenge for first-time single-incision adopters. As the overall flexibility of the instruments increases, triangulation issues can be overcome without sacrificing external maneuverability.
Flexible instruments have articulating shafts, steering the tip of the instrument toward the target organ and restoring lost triangulation. Thus, combining flexible and rigid instruments has resulted in a more comfortable configuration (Fig. 33.4D, E), increasing maneuverability and the feasibility of advanced surgical procedures using a single incision.
Conflict of Instruments
Multiple instruments inserted at close proximity through a common port of entry produce an undesirable limitation of movement both inside and outside. Many advanced
procedures involve switching instruments and trocars more often, which could compromise the pneumoperitoneum. These challenges have led to the development of multichannel ports to avoid the clinching of laparoscopic instruments diverting from a common point.
procedures involve switching instruments and trocars more often, which could compromise the pneumoperitoneum. These challenges have led to the development of multichannel ports to avoid the clinching of laparoscopic instruments diverting from a common point.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree