Fig. 2.1
Use of a flexible and roticulating tip forceps and an ultrasonic dissector during single-incision laparoscopic appendectomy
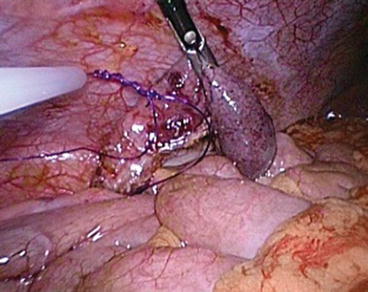
Fig. 2.2
Use of Endoloop (5 mm) for closure of the appendiceal stump before transection of the appendix
On the other hand, there are at least three different approaches to site and handle the wound, and there is yet any consensus as to which one is better.
1.
Single fascial incision
Commercially, there is a number of proprietary, multilumen, single-trocar systems specifically designed for single-incision surgery. The more commonly used ones include the TriPort (Olympus Medical), the SILS port (Covidien), the CX Cone (Karl Storz), and some gel port systems (Figs. 2.3 and 2.4). All these devices share the concept that only one single fascial incision (usually transumbilical) is required for passage of the composite port through which the laparoscope and instruments are inserted into the abdominal cavity. Theoretically, they minimize friction injury to the soft tissues at wound site and reduce inadvertent damage to the shaft of laparoscopic instrument during manipulation. Cost is one of the prohibitory factors why surgeons do not use them more often.



Fig. 2.3
The LESS port (Courtesy of Covidien, MA, USA) for SILA

Fig. 2.4
The TriPort (Courtesy of Olympus, Tokyo, Japan) being used for SILA
Alternatively, some surgeons adopt the so-called “glove-port” method when performing SILA [27]. In brief, a small fascial incision about 2–2.5 cm is made through the umbilicus. A small-sized wound retractor is inserted across this fascial wound using the Hasson technique. A sterile latex glove is mounted onto the external rubber ring of the wound retractor, and multiple plastic or metal trocars are then inserted through the glove into the peritoneal cavity for passage of video telescope and other laparoscopic instruments.
2.
Single skin wound with multiple fascial incisions
Instead of using the single fascial incision technique, which may entail the cost of expensive composite port systems, some surgeons opt for making a single skin incision either transumbilically or infraumbilically in a curvilinear manner. Subcutaneous dissection is performed under the skin incision to allow exposure of a small area of anterior rectus fascia. Trocars of 5 mm or 10 mm are then inserted through different fascial incisions made in this wound. To minimize collision of instruments at the entry point, low-profile trocars bearing smaller external components are preferred. This technique is less expensive than the single-port method, but it may also be the culprit of more postoperative wound pain and surgical site complications such as bruises, hematoma, and infection.
3.
Suprapublic single–incision approach
Some surgeons considered a transumbilical scar is cosmetically unsightly and a disadvantage of SILA. They proposed using the suprapubic approach for SILS so that the visible part of the abdomen could be left with no scars [28, 29]. One of the advantages of this approach includes a better view of the appendix and its base, thus avoids inadvertent injury to the cecum especially in retrocecal and gangrenous appendicitis. Another advantage is the close proximity of the suprapubic wound to the pelvis, which facilitates rinsing of the area safely in case of a ruptured appendicitis. While initial reports claimed better cosmetic outcomes with an acceptable operation time and relatively low wound pain score with this approach, clinical pictures of scars published in these articles were not quite appealing. Some of them appeared as if a conventional McBurney’s incision had been shifted to the hypogastrium.
2.5 Current Evidence
Many of the earlier series of SILA were single-arm studies. Most of them confirmed that SILA was a feasible and safe option in the management of uncomplicated acute appendicitis. Subsequently, some comparative studies had also been published but were based largely on retrospective data with small sample size [30, 31].
It was not until 5 years after Ates’s series that St. Peter et al. and Teoh et al. reported the first truly randomized trial comparing SILA versus conventional 3-port appendectomy in children and adults, respectively [32, 33]. Of the 200 patients recruited in Teoh’s study, 98 SILA and 97 3-port appendectomies had complete set of data for further analysis. While there were no difference between the two groups in the morbidity rates, operative time, conversion rates, overall pain score, and pain score at rest, those with SILA did have significant more pain upon coughing or standing and required more intravenous analgesics (p = 0.001, 0.038, and 0.035, respectively). On the other hand, cosmetic satisfaction was better in the SILA group when compared to the 3-port appendectomy group.
There were at least three more randomized trials published afterwards [34–36]. Many systematic reviews and meta-analyses have also been released recently. The latest meta-analysis includes 5 randomized trials covering a total of 746 patients [37]. Thirty-day morbidity and wound infection rates were similar between SILA and conventional laparoscopic appendectomy, but SILA required a significantly longer operating duration to accomplish. More importantly, despite pooling of information from over 700 patients, the authors commented that the available data were not robust enough to reach any conclusions regarding hospital stay, postoperative wound pain, and open conversion.
The lack of instrument triangulation in SILA often results in poor ergonomics, which may be reflected by the increased operating time seen for SILA. It is noteworthy that in another meta-analysis, it was revealed that about 7 % of patients needed the insertion of an additional port, even in the hands of experienced laparoscopic surgeons with a low open conversion rate [38].
If SILA is not inferior to conventional 3-port laparoscopic appendectomy in terms of safety, it seems that the price to pay for a cosmetic benefit is the longer operating time. However, St. Peter et al. reviewed the cost-effectiveness of the two procedures and demonstrated significantly higher hospital cost associated with SILA (US$17,600 ± 4,000) versus conventional laparoscopic appendectomy (US$16,600 ± 3,900; p = 0.005). It is probably due to the use of extra equipment in addition to the longer operating room usage.
2.6 Future Perspectives
There is currently little evidence available regarding the effectiveness of SILA in specific challenging patient cohorts, including obese and elderly patients and those with multiple medical comorbidities. As some surgeons use a multiport device through a single fascial incision for the insertion of laparoscopic instruments, whereas others use three separate trocars through multiple fascial incisions, it is not sure which technique may end up with more incisional herniation in the long term. All these could be interesting areas of future research.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








