Fig. 9.1
Surgical team position
Long and straight atraumatic bowel graspers
Scissors
Bipolar diathermy forceps
Monopolar diathermy hook
Articulated linear stapler
Circular stapler
Suction irrigator
Titanium clip applier, small and medium
9.2.2 Patient Position
The patient is placed in supine position with legs apart. The right arm is adducted, while the left one is opened. The surgeon is sitting at the right side of the patient, and the camera assistant is located to the right side of the first operator during the splenic flexure mobilization while to the left side during the other steps. The nurse stays between the legs of the patient.
It is mandatory to place nasogastric tube and bladder catheter.
The monitor is placed in front of the surgeon, at the level of the left thigh, so that the surgeon, working field and monitor represent almost subsequent points of the same axle.
We suggest to use the energy device having commands with pedals to obtain more hand freedom.
9.2.3 Step-by-Step Technique
All patients underwent single-access laparoscopic left hemicolectomy using the device “QuadPort Plus access system” (Advanced Surgical Concept, Tokyo, Japan). A 3–4-cm vertical incision was made in the umbilical fold. The umbilicus was suspended for the “QuadPort Plus access system” insertion, and the pneumoperitoneum was obtained with CO2 gas (Fig. 9.2).


Fig. 9.2
QuadPort Plus access system device
In high reverse Trendelenburg position, the mobilization of the splenic flexure and descending and sigmoid colon was performed, and the Gerota fascia (Fig. 9.3) was detached from the Toldt fascia. The gonadal vessels and the left ureter were identified under the Gerota fascia. During this step, it is very important to find the best position between the straight graspers and the 5-mm camera. With some flexible optic, it is possible to avoid the internal instrument clashing as well as the operator hands fight (Fig. 9.4).
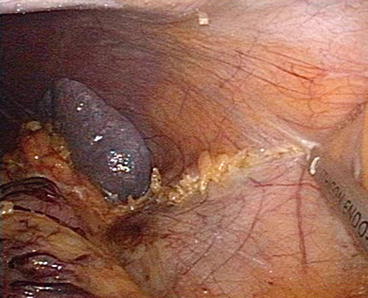
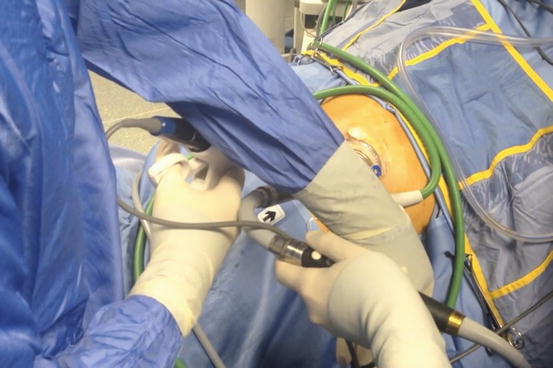
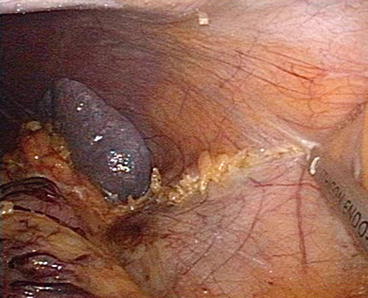
Fig. 9.3
Splenic flexure mobilization
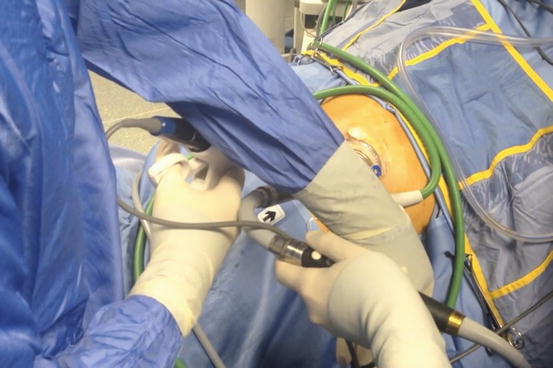
Fig. 9.4
Operator hands fight
During a conventional laparoscopic colectomy, we used to dissect the plane between the Gerota and Toldt fascia pulling down the splenic flexure. During a single-access procedure, instead, this movement is not very easy and effective. So we add to this an opposite movement of the right hand pushing down the Gerota fascia.
We suggest extending the dissection as much as possible down to the left parieto-colic ligament in such a way to make the next step easier.
In slight Trendelenburg position, the inferior mesenteric vein was isolated and transacted at the inferior margin of the pancreas after the incision of the Treitz muscle. The artery was isolated and transected about 2 cm over the aorta, after a complete mobilization of the sigmoid colon (Fig. 9.5).
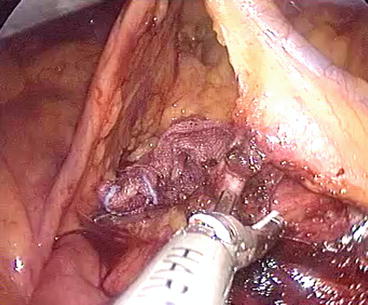
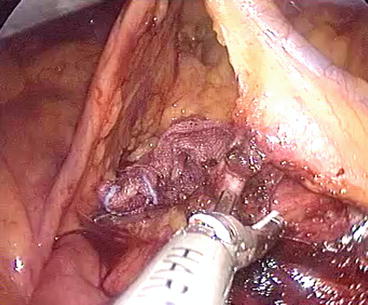
Fig. 9.5
Inferior mesenteric artery isolation
In some cases of benign disease, we applied a standardized technique for the preservation of the inferior mesenteric artery (IMA) as reported by Valdoni et al. [3, 4].
The transection of the sigmoid-rectal junction was done in the same way as the conventional laparoscopic procedure. We suggest to use an articulated linear stapler with the handle rotated at the top.
The left colon resection was completed extracorporeally after the umbilical extraction (Fig. 9.6), and the head of the 33-mm circular stapler was inserted to the proximal colonic segment using a purse string of polypropylene. The T-T-stapled colorectal anastomosis was performed intracorporeally according to the Knight-Griffen technique and checked by hydro-pneumatic test.
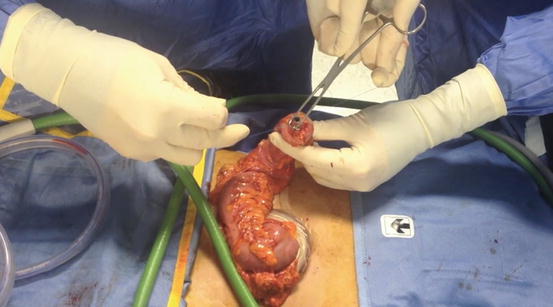
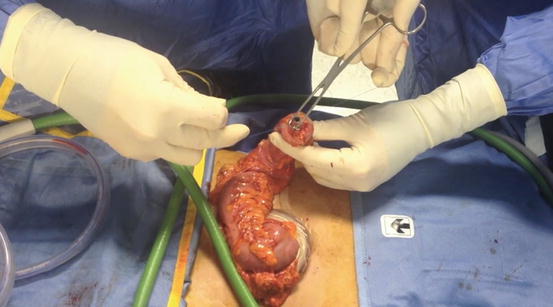
Fig. 9.6
Extracorporeal preparation of left colon
The umbilical fascia was closed with continuous suture, and the skin was closed with Dermabond glue (Ethicon Inc, Cincinnati, OH, USA) (Fig. 9.7).


Fig. 9.7
Final result of skin incision
9.3 Our Experience
Our experience included 45 single-access left hemicolectomies with or without preservation of the IMA. All procedures were performed from October 2009 to August 2013.
The mean age was 63 years (range 37–84 years old); the mean BMI was 27.34 kg/m2 (range 19.82–30.1 kg/m2). Demographic and pathological features are summarized in Table 9.1.
Table 9.1
Demographic features
Demographic and pathological features | |
|---|---|
Patient number | 45 |
Male | 18 |
Female | 27 |
Age (mean/range) years | 63/37–84 |
BMI (mean/range) kg/m2 | 27.34/19.82–30
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





