Fig. 6.1
Patient and team positioning
6.2.2 Hiatal Hernia Repair
6.2.2.1 Beginning of the Procedure
The umbilicus is incised, and the fascia is opened until the peritoneal sheet is reached, which is opened as well. A purse-string suture using PDS 1 is placed in full-thickness method in the umbilical fascia and peritoneum at 1-, 3-, 5-, 6-, 7-, 9-, 11-, and 12-o’clock positions (Fig. 6.2). An 11-mm reusable metallic trocar is introduced into the peritoneal cavity inside the purse-string suture, and the pneumoperitoneum is created. A 10-mm, 30° rigid and standard length scope (Karl Storz-Endoskope) is advanced through the 11-mm trocar, and the DAPRI curved reusable instruments (Karl Storz-Endoskope) are inserted into the abdomen through the umbilical scar without trocars (Fig. 6.3). The bicurved grasping forceps III (Fig. 6.4a) is inserted through a separate fascia window, created by a wire of 5-mm trocar, at some of 5 mm, outside the purse-string suture at 10-o’clock position in respect of the patient’s head. The other instruments like the monocurved coagulating hook (Fig. 6.4b), the monocurved scissors (Fig. 6.4c), the monocurved RoBi bipolar grasping forceps and scissors (Fig. 6.4d, e), the monocurved needle holder II (Fig. 6.4f), the monocurved suction and irrigation cannula, the straight 5-mm clip applier, and the straight 5-mm grasping forceps are introduced on the other side of the bicurved grasping forceps III at 3-o’clock position, parallel to the 11-mm trocar and inside the purse-string suture. The suture is adjusted to maintain a tight seal around the 5-mm tools and the 11-mm trocar and opened only for the change of the instruments and evacuation of the smoke created with the dissection. The operative table is positioned in a reversed Trendelenburg position.
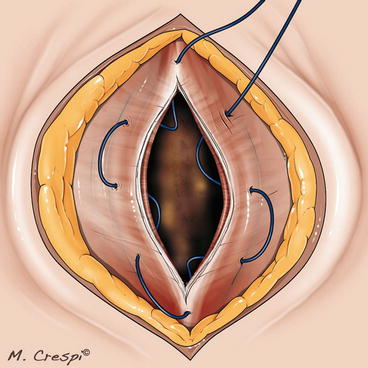
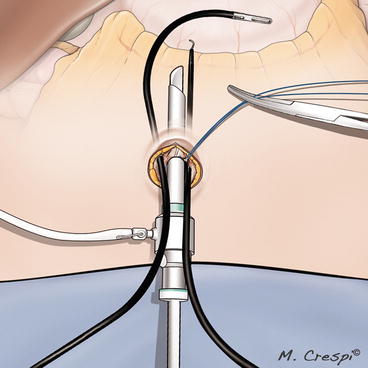
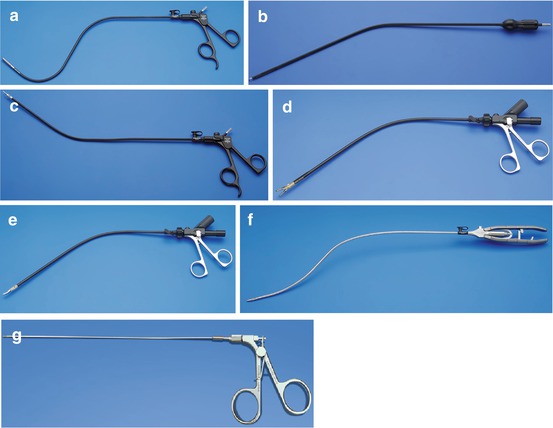
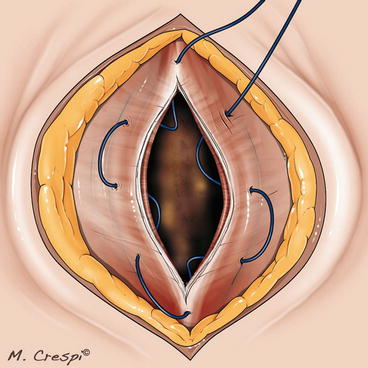
Fig. 6.2
Hiatal hernia repair: placement of the purse-string suture at the access-site (umbilicus)
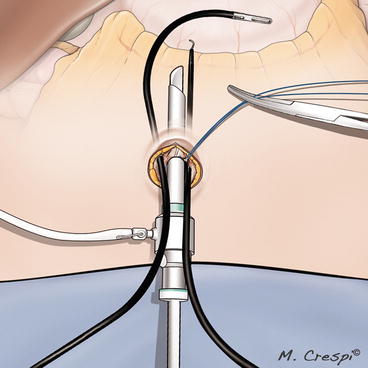
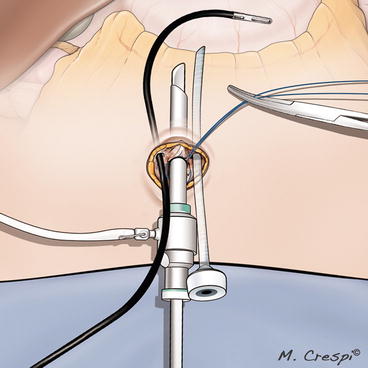
Fig. 6.3
Hiatal hernia repair: placement of the instruments through the access-site
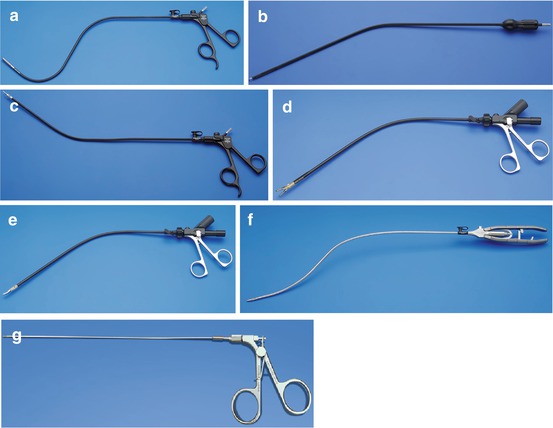
Fig. 6.4
DAPRI instruments: bicurved grasping forceps III (a), monocurved coagulating hook (b), monocurved sicssors (c), monocurved RoBi bipolar grasping forceps and scissors (d, e), bicurved needle holder II (f), straight 1.8-mm trocarless grasping forceps (g)
The distal curve of the bicurved grasping forceps III is used to retract the left liver lobe and to contemporary expose the opening of the hepatogastric ligament on the lesser curvature. If an insufficient exposure of the hiatal region is shown, the DAPRI 1.8-mm trocarless grasping forceps (Karl Storz-Endoskope) (Fig. 6.4g) is inserted percutaneously through a skin puncture under the xyphoid access, created by a Veress needle.
The hepatogastric ligament is opened close to the liver segment 1, and the right phrenogastric ligament is incised as well, dividing its anterior and posterior sheets. The right crus is freed from the bottom to top (Fig. 6.5). Thanks to the peculiar shape of the instruments, the scope never appeared in conflict with the instruments’ tips, and the conflict between the surgeon’s hands and the scope is avoided (Fig. 6.6). The left phrenogastric ligament is incised, and the left crus is exposed. The lower esophagus is freed, encircled, and suspended by a piece of cotton tape using the bicurved grasping forceps III (Fig. 6.7a). Thanks to this maneuver, both crura under the esophagus are better exposed and more easily freed (Fig. 6.7b).
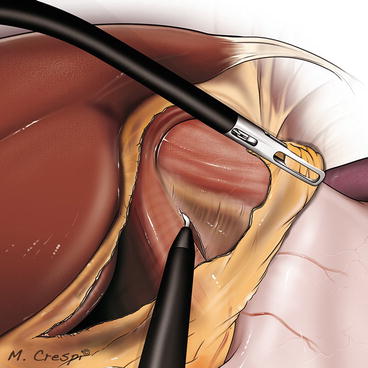
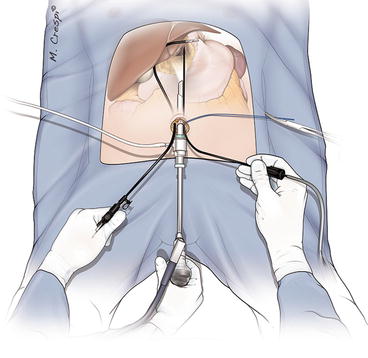
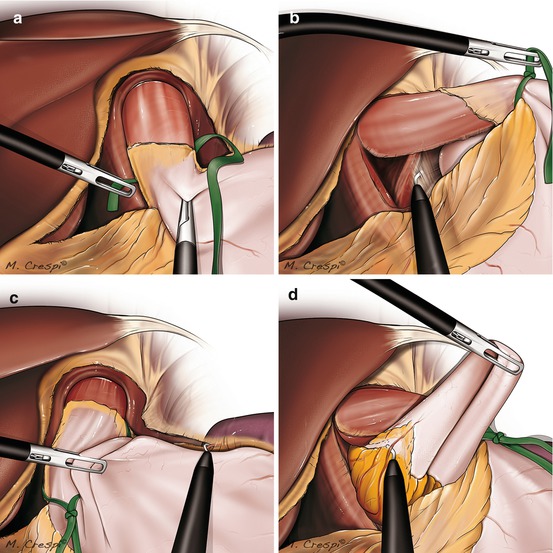
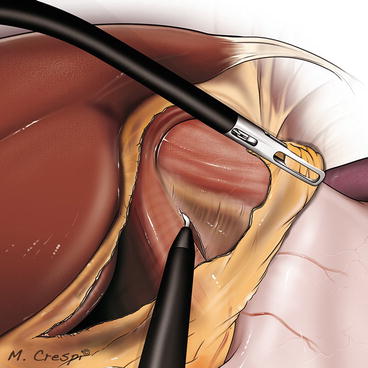
Fig. 6.5
Skeletonization of the right crus from bottom to top
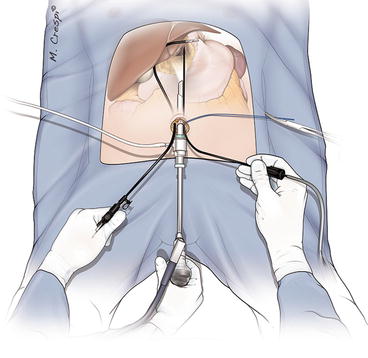
Fig. 6.6
The conflict between the surgeon’s hands, and between the instruments’ tips is avoided thanks to the peculiar curved shape of the instruments
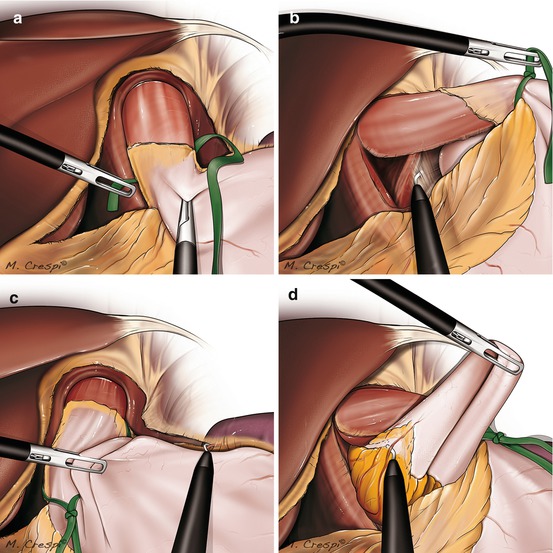
Fig. 6.7
The lower esophagus is encircled by a piece of cotton tape (a), permitting a better exposure of the both crura (b); control of the first short gastric vessel by a medial-to-lateral approach (c), and of the other short gastric vessels just “à la demand” by a medial-to-lateral approach (d)
The operative table is maintained in a reversed Trendelenburg position with right-sided tilt, permitting an increased exposure of the splenic region. The gastrosplenic ligament is incised starting from the previous dissection of the left phrenogastric ligament, to control the first short gastric vessel (Fig. 6.7c). Then, the operative table is replaced without any tilt maintaining the Trendelenburg position, in order to move the upper part of the gastric fundus behind the lower esophagus. The other short gastric vessels are just dissected “à la demand” giving a more slack to the wrap (Fig. 6.7d), using the monocurved coagulating hook or the monocurved bipolar grasping forceps and scissors.
Figure of 8 sutures using silk 2/0 are used to close the crura, using intracorporeal sutures and knotting technique (Fig. 6.8). This maneuver is realized without the orogastric bougie (34 French), which is pushed by the anesthesiologist only after the cruraplasty.
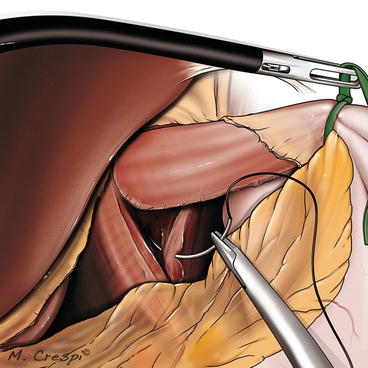
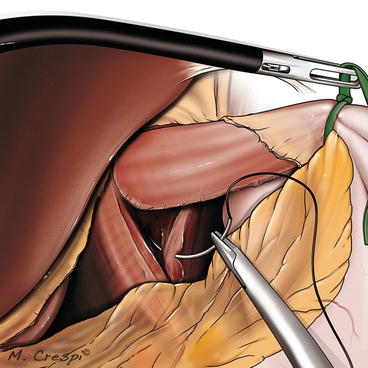
Fig. 6.8
Figure of 8 sutures are used to close the crura, using intracorporeal sutures and knotting technique
6.2.2.2 Nissen Fundoplication
The floppy 360° fundoplication is performed using intracorporeal sutures (silk 2/0) and knotting technique, under ergonomic position and without clashing of the instruments’ tips (Fig. 6.9a). A gastro-gastric suture, a gastro-eso-gastric suture (Fig. 6.9b), and two gastroesophageal sutures inferiorly to the first previous and on both sides of the lower esophagus are performed (Fig. 6.9c).
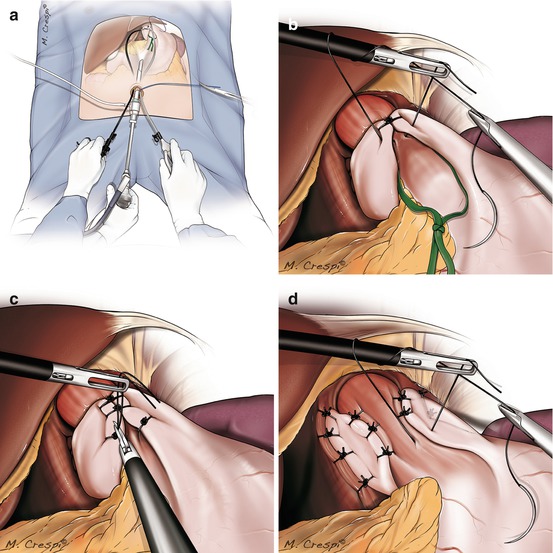
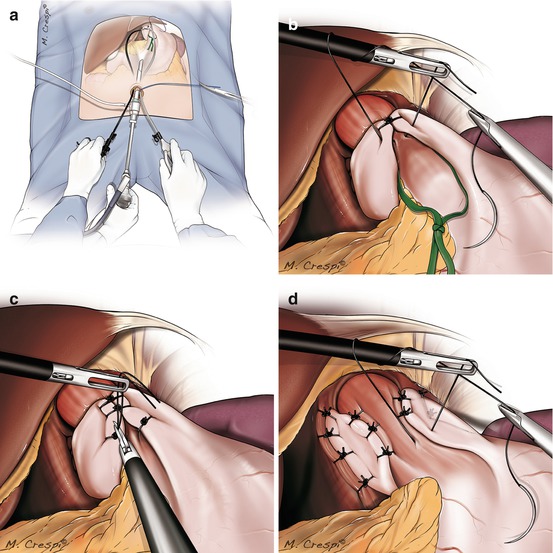
Fig. 6.9
The fundoplication is performed under ergonomic position and without clashing of the instruments’ tips (a); Nissen fundoplication (b, c); Toupet fundoplication (d)
6.2.2.3 Toupet Fundoplication
The 270° fundoplication is performed using silk 2/0 sutures. The right side of the wrap is fixed by four simple sutures to the right crura, starting with the first suture at the apex of the right crura. Then, the right side of the wrap is anchored to the lower esophagus by three other simple sutures. As well, the left side of the wrap is fixed to the left crura by two simple sutures, and then the left side of the wrap is anchored to the lower esophagus by three other simple sutures (Fig. 6.9d).
6.2.2.4 End of Both Fundoplications
At the end of the procedure, the operative table is replaced like in the beginning of the procedure, without any Trendelenburg position and tilt. The orogastric bougie, the piece of cotton tape, the needles, and all the instruments are removed under view. The curved instruments are retrieved following their curves at 45° in respect of the abdominal wall.
The 11-mm trocar for the scope is removed, Vicryl 1 sutures are placed as figure of 8 to close the umbilical fascia, including the separate fascia opening for the bicurved grasper (Fig. 6.10). Intradermal sutures close the cutaneous scar.
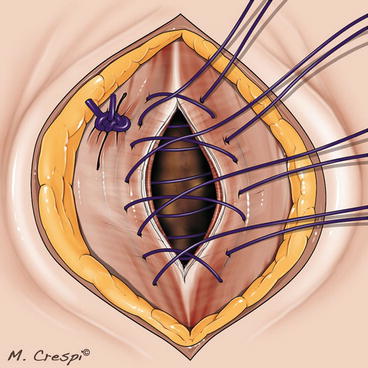
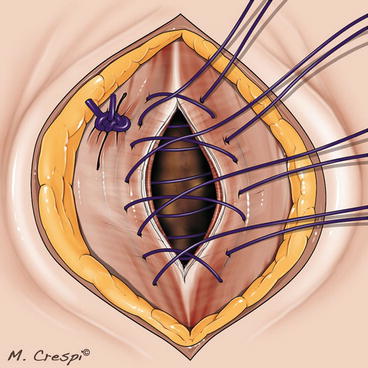
Fig. 6.10
Figure of 8 sutures are used to close the umbilical fascia, including the separate fascia opening for the bicurved grasper
6.2.2.5 Postoperative Care
One gram of paracetamol is given i.v. at the end of the surgical procedure. Postoperative analgesia is given following the WHO visual analog pain scale (VAS). In the recovery room, the following scheme is followed: for VAS between 1 and 3, 1-g paracetamol i.v. is pushed; for VAS between 4 and 8, 100-mg tramadol i.v. is used; and for VAS >8, 1-mg piritramide i.v. is incremented.
After the patient left the recovery room, pain is assessed every 6 h, with 1-g paracetamol administered i.v. if VAS is between 1 and 3, 100-mg tramadol administered i.v. if VAS is between 4 and 8, and 1-mg piritramide administered i.v. if VAS is >8.
A gastrograffin swallow check is scheduled on the first postoperative day, and if negative, the patient is allowed to drink water and, after 24 h, to tolerate a light diet. If there are no complications, the patient is discharged on the second postoperative day.
Upon discharge, 1-g paracetamol perorally or 50-mg tramadol perorally is prescribed only if needed.
Office visits are scheduled at 10 days, 1, 3, 6, and 12 months after the procedure. Barium swallow checks are performed at 6 and 12 months.
6.2.3 Gastric Resections
6.2.3.1 Beginning of the Procedure
The umbilicus is incised, and the fascia is opened until the peritoneal sheet is reached, which is opened as well. A purse-string suture using PDS 1 is placed in full-thickness method in the umbilical fascia and peritoneum at 1-, 3-, 5-, 6-, 7-, 9-, 11-, and 12-o’clock positions (Fig. 6.2). An 11-mm reusable metallic trocar is introduced into the peritoneal cavity inside the purse-string suture, and the pneumoperitoneum is created. A 10-mm, 30° rigid and standard length scope (Karl Storz-Endoskope) is advanced through the 11-mm trocar, and the DAPRI curved reusable instruments (Karl Storz-Endoskope) are inserted into the abdomen through the umbilical scar. The bicurved grasping forceps III (Fig. 6.4a) is inserted through a separate fascia window, created by a wire of 5-mm trocar, at some of 5 mm, outside the purse-string suture at 10-o’clock position with respect of the patient’s head. The other instruments like the monocurved coagulating hook (Fig. 6.4b), the monocurved scissors (Fig. 6.4c), the monocurved RoBi bipolar grasping forceps and scissors (Fig. 6.4d, e), the bicurved needle holder II (Fig. 6.4f), the monocurved suction and irrigation cannula, the straight 5-mm harmonic shears (Ethicon, Johnson & Johnson, Cincinnati, OH, USA), and the straight 5-mm grasping forceps are introduced through a 6-mm flexible trocar (Karl Storz-Endoskope) positioned at 5 mm outside the purse-string suture at 2-o’clock position with respect of the patient’s head (Fig. 6.11). The suture is adjusted to maintain a tight seal around the 11-mm trocar. The operative table is positioned in a reversed Trendelenburg position.