Fig. 15.1
External instrument conflict and clashing resulting in awkward surgeon/assistant positioning during single-incision laparoscopic colectomy
Room Setup and Positioning
The operating room equipment requirements are identical to those for any other laparoscopic procedure. The surgeon/patient configuration is a “surgeon-disease-screen” setup, which refers to surgeon location contralateral to the diseased segment of the colon, the patient, and the laparoscopic monitor in the ipsilateral side of the diseased colon. For sigmoid/left colectomy, the surgeon and assistant are located on the right side of the patient, while the monitor is on the left.
The patient is secured to the operating room table with both arms tucked in modified lithotomy position and in moderate Trendelenburg with the left side elevated. Anti-slip rubber pads can be used to avoid the patient from sliding off – for adequate patient securing. A “wrapped” technique securing the patient with a three-inch adhesive tape placed at the level of the chest provides tight securing yet allows appropriate chest wall expansion and air flow.
Port Placement and Extraction Sites
There are several single-port devices commercially available, including the SILS® Port (Covidien, Mansfield, MA, USA), GelPOINT® Advanced Access Platform (Applied Medical, Rancho Santa Margarita, CA, USA), and TriPort Access System (Olympus Corporation, Tokyo, Japan), among others (see Fig. 15.2). In addition, sealed hand-assist devices, such as the GelPort® (Applied Medical), may also be utilized for single-incision laparoscopic colectomy. In our institution, the majority of our experience is with the SILS® and GelPOINT® devices.


Fig. 15.2
Three of the many single-port devices available in the market. (a) SILS® Port (Covidien, Mansfield, MA, USA); (b) the GelPOINT® Advanced Access Platform (Applied Medical, Rancho Santa Margarita, CA, USA); and (c) TriPort Access System (Olympus Corporation, Tokyo, Japan)
The SILS® port is a low-profile, one-piece device that allows easy insertion and removal. However, this device has several shortcomings including poor malleability, it is fixed with closely spaced port sites, and it has to be removed upon specimen extraction. The use of a fourth port, although is feasible, demands sacrificing the smoke evacuator. Furthermore, the incision cannot be extended, which restricts its use – especially in those with bulky specimen or thick subcutaneous fat. Another disadvantage is that the SILS® port tends to displace in patients with thick abdominal wall or during instrument torquing, thus releasing the pneumoperitoneum.
The GelPOINT® on the other hand, although more costly, is a more versatile device that allows multiple port placement, sacrificing neither CO2 insufflation nor smoke evacuator. Moreover, the wound protector is included in the device and affords adjustment based on incision length and abdominal wall thickness.
In comparison with multiport laparoscopy, single-incision laparoscopic port placement is substantially simplified. The single-incision approach affords a straightforward abdominal entry under direct visualization, eliminating the risk for port site bleeding and/or internal organ damage.
For sigmoid and left colectomy, the single-incision device is typically placed through a midline umbilical incision or via a Pfannenstiel incision. Each of these location sites has benefits and shortcomings as compared with one another. An alternative access is through a Pfannenstiel incision with an additional 5 mm umbilical port for the camera (Single + 1 technique) (see port configuration).
The transumbilical access is performed through a 2.5–3.0 cm skin incision. After division of the subcutaneous fat, the umbilical stump is identified and divided (see Fig. 15.3). Since the umbilical stump is a natural fascial defect, its division allows an extension of the fascial incision to approximately 5 cm, without requiring extension of the skin incision. This maneuver expands the port site, thus reducing instrument clashing and facilitating removal of bulky disease. The umbilical port location enhances versatility and maneuverability, as the instruments are located in the middle of the target operative fields (see Fig. 15.4a) – resulting in optimal reach to the distal transverse colon and splenic flexure and to the sigmoid and upper rectum. As such, this access location is considered more suitable for those surgeons early in their experience with the single-incision approach. However, as compared to Pfannenstiel incision, the umbilical access is associated with significantly higher hernia rates [9, 10].
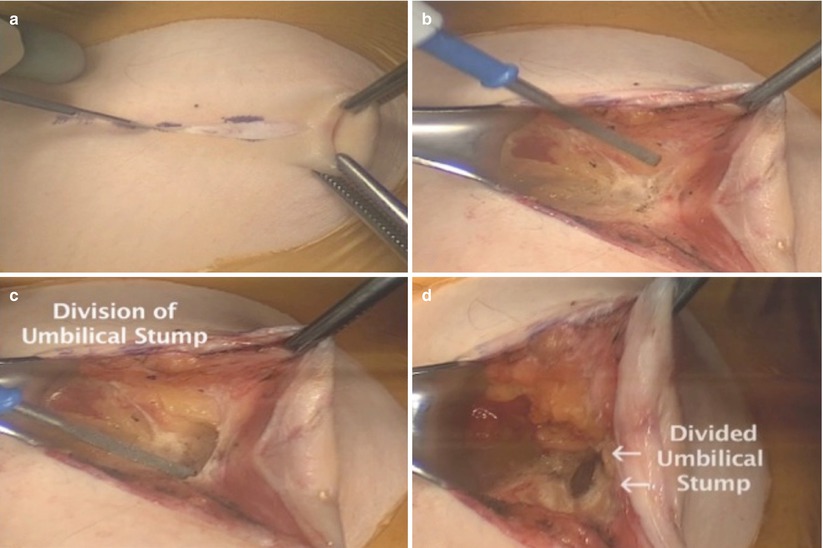
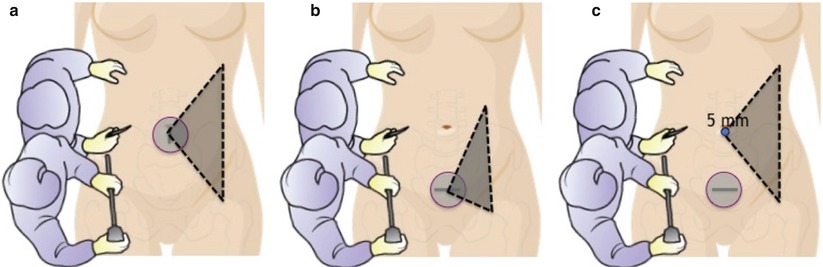
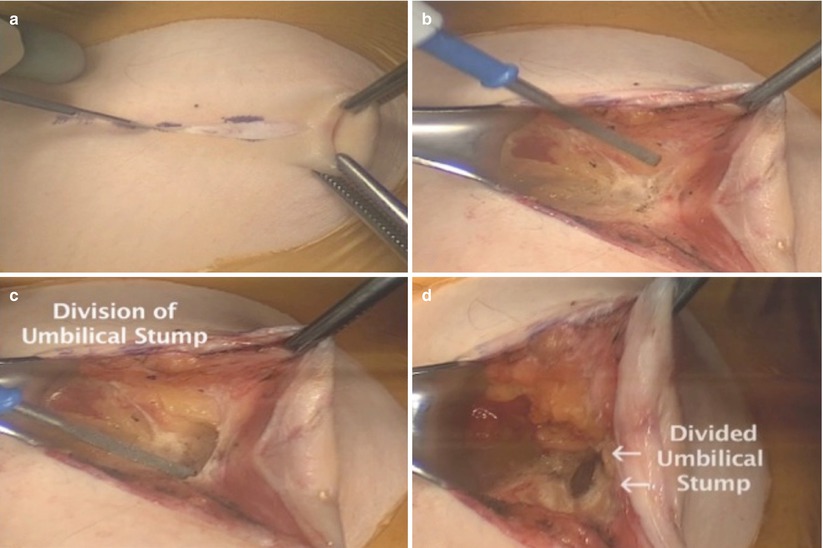
Fig. 15.3
Umbilical access through a 2.5–3.0 cm skin incision. After division of the skin and subcutaneous fat (a, b), the umbilical stump is identified and divided (c, d)
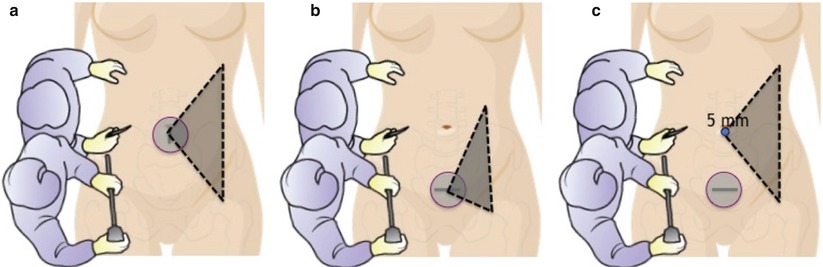
Fig. 15.4
Operative view perspective. The umbilical access (a) allows optimal view and reach to the distal transverse colon and splenic flexure and to the sigmoid and upper rectum. The Pfannenstiel access (b) has limited reach for splenic flexure takedown and restricts maneuverability due to the instrument close proximity to the target operative field. The “single + 1” technique (c) results in enhanced and expanded view, reduces instrument conflict, and facilitates access to the splenic flexure with the use of bariatric length instruments
For the Pfannenstiel incision access, a 3.5–4.0 cm skin incision is performed, and the peritoneal access is accomplished in a conventional fashion with a muscle splitting technique. This access affords enhanced cosmetic outcomes and lower hernia rates in comparison with the umbilical access. However, the Pfannenstiel incision access demands high laparoscopic technical skills and expertise. When introducing the laparoscopic instruments into the single-port device, they are located in extreme close proximity to the sigmoid and rectosigmoid. Therefore, this access restricts visualization, maneuverability, and range of motion. Additionally, reach to the splenic flexure is also limited due to the distance between the access site and the left upper quadrant (see Fig. 15.4b). Despite these challenges, there are technical modifications that allow the successful completion of the procedure using the Pfannenstiel access. In order to improve the visualization and view perspective of the operative field, an additional umbilical 5 mm port for the laparoscope may be utilized, resulting in the “Single + 1” technique (see Fig. 15.4c). This technique results in enhanced and expanded view, facilitated access to the splenic flexure, and reduction of instrument conflict. During the splenic flexure takedown, however, extra-long instrumentation is often required for retraction and reach.
The port placement itself depends on the specific device. The SILS® port placement is typically facilitated with the use of a curved clamp. The GelPOINT® insertion is achieved by introducing the Alexis® (Applied Medical) wound retractor, followed by the placement of the GelSeal® (Applied Medical) cap. In order to avoid injury, three trocars are inserted in a triangular fashion to the GelSeal® before its attachment to the wound protector component. Regardless of the type of device, once the single-port platform is placed, the instruments are inserted and the pneumoperitoneum is created.
Operative Steps (Table 15.1)
Table 15.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Insertion of the single port and exploratory laparoscopy | 1 |
2. Mobilization of the sigmoid colon, identification of the left ureter, and ligation of the inferior mesenteric artery | 6 |
3. Mobilization of the descending colon and splenic flexure with identification and ligation of the inferior mesenteric vein | 6 |
4. Transection of the sigmoid colon | 5 |
5. Anastomosis with leak test | 2 |
Insertion of the Single Port and Exploratory Laparoscopy
The procedure is initiated with exploration to assess the abdominal cavity and in cases involving malignant pathology, to evaluate the presence of distant metastases. When required, lysis of adhesions may also be performed promptly. In some occasions, adhesions are encountered upon entry to the peritoneal cavity. In such cases, it is often useful to perform adhesiolysis with the aid of laparoscopic visualization even before the placement of the single-port device and creation of pneumoperitoneum (see Fig. 15.5). This affords the release of bowel loops adhered to the abdominal wall and clears the fascial incision in order to safely place the device.
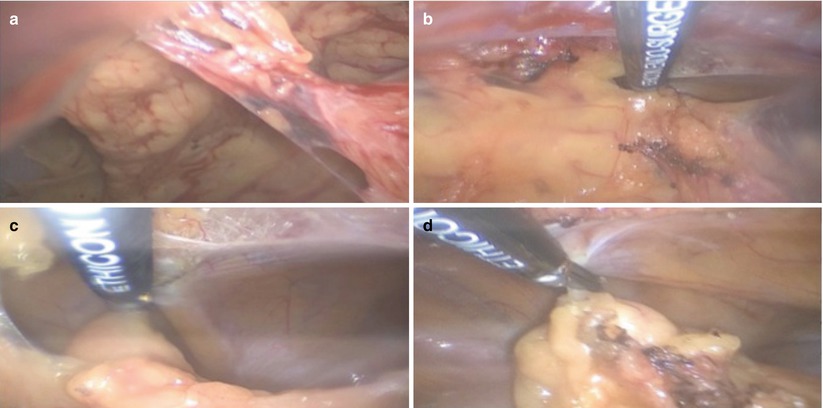
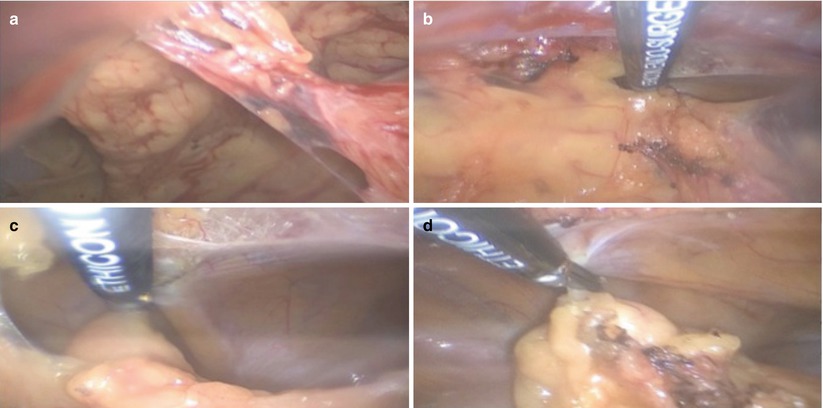
Fig. 15.5
“Pneumoless” lysis of adhesions may be accomplished prior the port placement to ensure safe abdominal cavity entry (a–d)
Mobilization of the Sigmoid Colon, Identification of the Left Ureter, and Ligation of the Inferior Mesenteric Artery
Following the laparoscopic exploration and taking advantage of the gravity with proper patient positioning – Trendelenburg and left-side elevation – the small bowel is retracted out of the operative field superiorly and to the right (Box 15.1). The rectosigmoid is identified and retracted laterally by countertraction, and a peritoneal incision is made medially at the level of the sacral promontory – with sharp incision or with monopolar energy such as the hook monopolar energy device (see Fig. 15.6a). Precise incision into the correct plane can be confirmed by the appearance of pneumo-dissection, which is characterized by bubble-like configuration expanding into the avascular areolar tissue (see Fig. 15.6b). Such pneumo-dissection in the avascular plane facilitates a clean precise dissection in a bloodless field. The presacral avascular plane is further developed with a tissue-sealing bipolar or other energy device, utilizing blunt and sharp dissection while maintaining hemostasis. A triangulation technique is utilized to further deepen the plane (see Fig. 15.7b). This technique facilitates exposure and dissection of the retroperitoneal plane with minimal clashing. In this technique, one instrument serves to elevate the tissue, while the other instrument carries out the dissection. It should be noted that triangulation technique is one of the cornerstones for successful completion of a single-incision laparoscopic approach and requires a medial-to-lateral dissection (see Video 15.1).
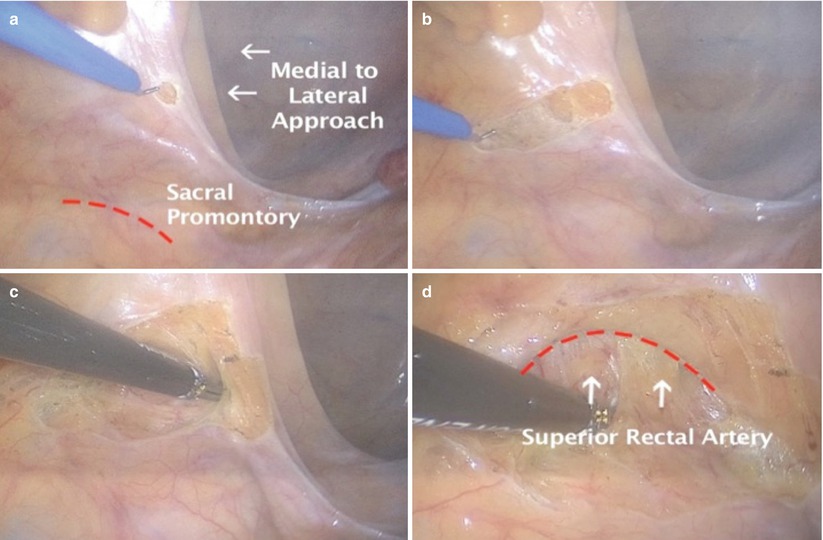
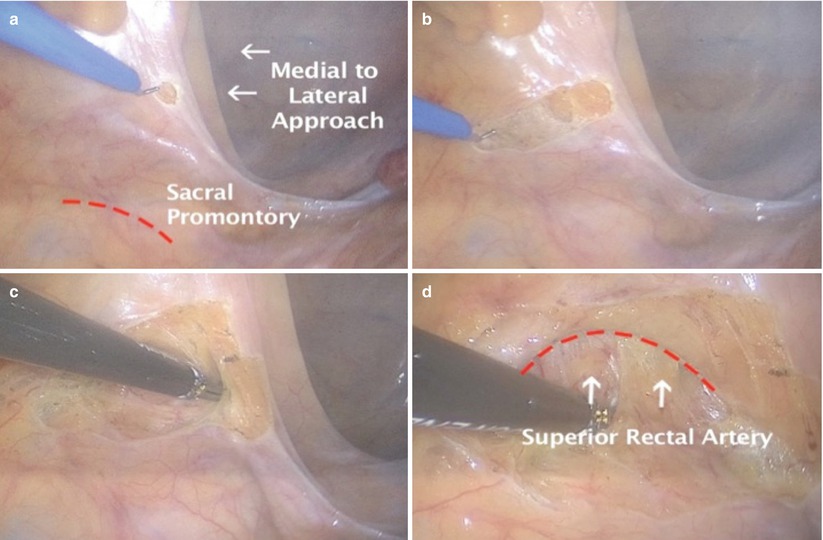
Fig. 15.6




Peritoneal incision to enter the presacral plane. The sacral promontory serves as anatomic landmark for the incision (a). The correct plane can be confirmed by the appearance of pneumo-dissection, characterized by bubble-like configuration expanding into the avascular alveolar tissue (b, c). As the plane is further developed the superior rectal artery is identified (d)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








