Fig. 13.1
Port configuration. C, 5 or 12 mm camera port; L1, 5 mm or 12 mm (for stapler) working port right hand; L2, 5 mm working port left hand; L3, 5 mm assistant port; L4, optional 5 mm assistant port
The most common extraction sites utilized for a total laparoscopic sigmoid colectomy are either a limited Pfannenstiel incision or a muscle splitting incision enlarging the LLQ trocar site. These extraction sites have the benefit of decreased incisional hernia rates compared to midline incisions. Rarely, the extraction site needs to be moved to a periumbilical incision in very obese individuals in which the purse string and anvil cannot be placed extracorporeally due to limited reach through a very thick abdominal wall in the Pfannenstiel location. Alternatively, the anvil can be secured intracorporeally using various techniques such as an endoloop placement.
Operative Steps (Table 13.1)
Table 13.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Exploratory laparoscopy | 1 |
2. Identification of the ureter and ligation of the inferior mesenteric artery | 5 |
3. Mobilization of the sigmoid colon | 3 |
4. Mobilization of the descending colon and splenic flexure with identification and ligation of the inferior mesenteric vein | 5 |
5. Transection of the sigmoid colon | 4 |
6. Anastomosis with leak test | 2 |
Exploratory Laparoscopy
The abdomen and liver is explored for malignant cases to evaluate for metastases (see Figs. 13.2 and 13.3). For patients with severe diverticular disease, the extent of the inflammatory process, adhesions, and phlegmon formation is assessed to evaluate feasibility of a safe total laparoscopic approach (Box 13.1). Alternatives are early conversion to a hand-assisted approach or laparoscopic mobilization of the splenic flexure only limiting the incision size of an open approach.
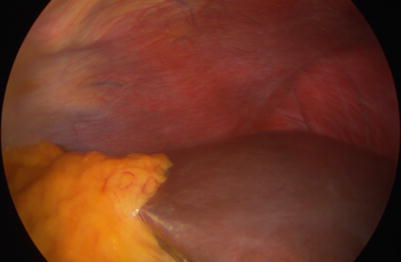

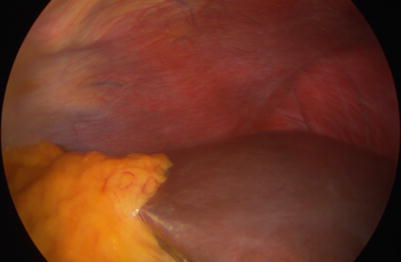
Fig. 13.2
Exploration of right liver lobe

Fig. 13.3
Exploration of left liver lobe
Box 13.1. Tip
Estimate the size of the final specimen, which might be enlarged due to various pathologic processes to see if a larger extraction site is needed and then convert to a hand-assisted technique rather than making the same incision at the end of a total laparoscopic approach.
Identification of the Ureter and Ligation of the Inferior Mesenteric Artery
One of the essential steps prior to vascular ligation is the identification of the left ureter (Box 13.2). The assistant through ports L3 and L4 typically tents the sigmoid colon or rectosigmoid colon up to achieve tension on the rectosigmoid mesentery (see Fig. 13.4). The surgeon uses a bowel grasper through L2 and a dissecting instrument in L1. The peritoneum is scored and blunt dissection identifies areolar tissue to enter the upper presacral space. Once this avascular plane is entered, it can be traced superiorly to separate the sigmoid colon mesentery from the retroperitoneum and the left ureter can be identified. The peritoneum proximal to the bulging inferior mesenteric artery (IMA) pedicle is scored and a window created. After identification of the IMA root and the bifurcation of the left colic artery, the IMA is ligated above or below the bifurcation depending on the patient’s individual anatomy and surgical indication for resection (see Fig. 13.5). Various bipolar vessel sealers, clips, or an endoscopic stapling device can be used (see Video 13.1).

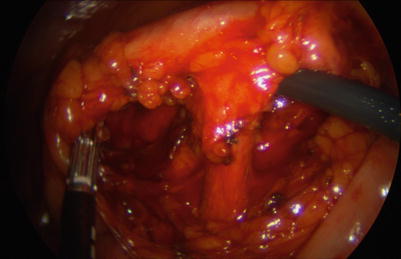

Fig. 13.4
Tension on the sigmoid colon mesentery
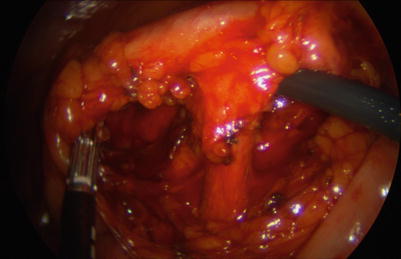
Fig. 13.5
Identification of the IMA (inferior mesenteric artery)
Box 13.2. Tip
If the sigmoid colon is densely adhesed towards the pelvis, it might be difficult to open the window between the superior rectal artery and presacral fascia. The adhesions might need to be divided first or the plane cephalad to the IMA entered first.
Mobilization of the Sigmoid Colon
If the mesocolon of the sigmoid colon was dissected off the retroperitoneum completely through the medial approach, only a thin layer of the peritoneum is left for easy division and this can be seen as a dark hue through the peritoneum (see Fig. 13.6) (Box 13.3). If the medial dissection is difficult and not progressing or the left ureter cannot be identified, the lateral mobilization can be used prior to a complete medial to lateral approach (see Video 13.2). The surgeon and the assistant retract the sigmoid colon medially and the mesocolon is separated off the retroperitoneal structures including the ureter similar to an open approach and the left ureter is seen.


Fig. 13.6
Lateral peritoneal layer after medial dissection
Box 13.3. Tip
Invariably, cases with more difficult anatomy will be encountered, and a switch back and forth between the medial and lateral dissection may be helpful.
Mobilization of the Descending Colon and Splenic Flexure with Identification and Ligation of the Inferior Mesenteric Vein
The inferior mesenteric vein can be ligated high next to the duodenum or more distally parallel to the inferior mesenteric artery. The decision is made based on the need to ligate high to ensure a tension-free anastomosis. The high ligation will be therefore described in the proctectomy chapters with coloanal anastomosis. Occasionally the patient’s anatomy may mandate high ligation of the IMV during a laparoscopic sigmoid colectomy.
The splenic flexure can be mobilized from a medial, lateral, or superior approach. The patient is placed in the reversed Trendelenburg position.
The medial approach is the continuation of the medal dissection of the descending colon mesentery off the retroperitoneum and Gerota’s fascia (see Fig. 13.7). This approach is suitable for isolation and high ligation of the IMV. Continuation of the dissection will identify the inferior border of the pancreas and dissection above the border will break through into the lesser sac. The assistant is again tenting up the descending colon through L3 and L4 and the surgeon is utilizing L1 and L2. The medial approach can be limited in obese patients with small bowel loops falling into the operative field.
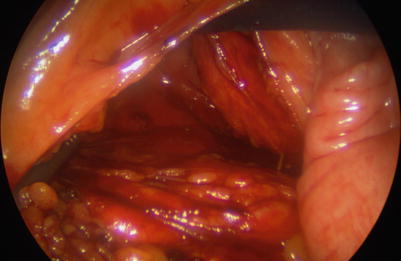
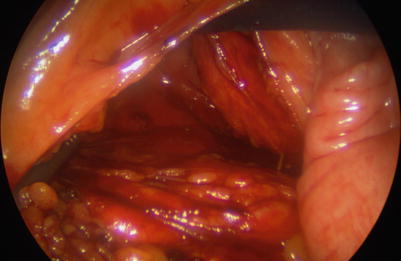
Fig. 13.7
Medial to lateral mobilization
The lateral approach is again similar to the open approach. The assistant is on the right side of the patient and retracts the descending colon medially through L2. The surgeon who is standing in between the legs uses L1 to retract the colon and L3 to dissect. The colon is progressively rolled over medially and separated from Gerota’s fascia. It is important to turn medially at the junction to the splenic flexure and not dissect along the line of Toldt lateral to the spleen.
The omentum is separated from the distal transverse colon and the lesser sac entered during the superior approach. The assistant is retracting the omentum or stomach superiorly through L4. The surgeon is retracting the colon inferiorly through L1 and using a dissecting instrument through L2. This allows visualization of the splenocolic attachments, which are divided gradually, and the colon is rolled over inferiorly meeting with the previous dissection planes.
Transection of the Sigmoid Colon
After identification of the distal resection margin, the peritoneum overlying the mesorectum is scored bilaterally towards the anterior rectal wall. Using gentle blunt dissection and partial division of the mesorectum, a window is created (see Fig. 13.8). An endoscopic stapler through the RLQ port L1 or the camera port is used for a perpendicular transection of the colon (see Video 13.3).
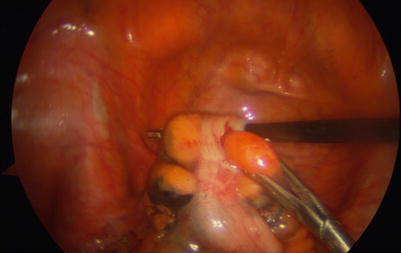
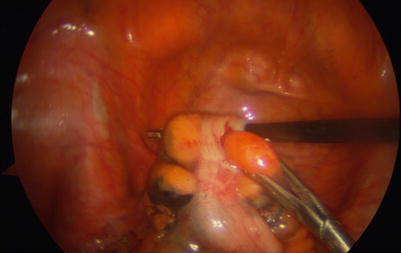
Fig. 13.8
Mesenteric window
Anastomosis with Leak Test
The proximal resection margin is identified, pulled towards the pelvis and the rectal stump to test tension-free reach, and marked using monopolar energy (Box 13.4). The colon is then exteriorized using a wound protector through a muscle splitting left lower quadrant or small Pfannenstiel incision, and the proximal colon is transected. After the anvil is secured using a purse string, the wound protector can be twisted 360° and then clamped with a ring clamp to allow re-insufflation. The circular stapler is placed through the rectum under laparoscopic guidance. The spike of the stapler is advanced through or right next to the center of the staple line (see Fig. 13.9), the anvil attached securely, and the anastomosis performed (see Fig. 13.10). If the stapler is not easily reaching the end of the rectal stump, a reversed Baker anastomosis can be performed traversing the spike of the stapler through the anterior rectal wall 5 cm distal to the end.
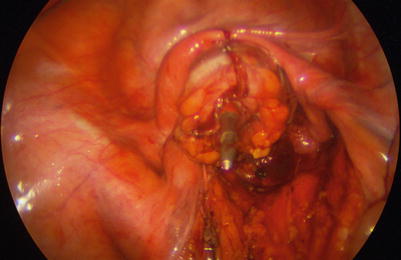
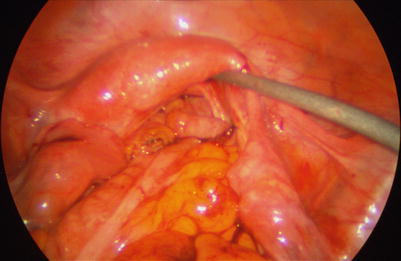
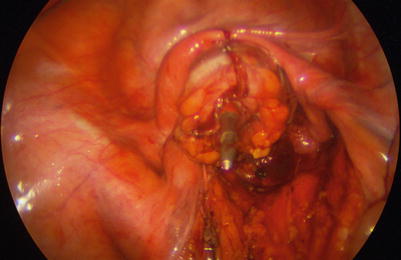
Fig. 13.9
Laparoscopic-guided stapler advancement
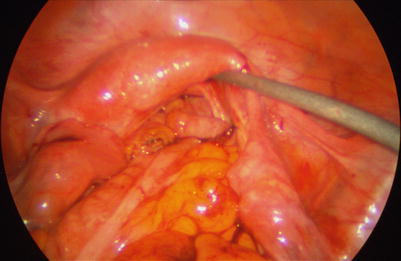
Fig. 13.10
Anastomosis
Box 13.4. Caveat
Do not force the stapler to the end of the rectal stump. Adequate prior partial mobilization of the rectal stump will certainly facilitate this, but a forceful attempt to reach the end can lead to premature separation of the staple line or an anterior rectal tear.
The doughnuts of the stapled anastomosis should be checked for completeness and sent to pathology for malignant disease. A colonoscope is inserted to observe the anastomosis for bleeding and completeness. The proximal colon is occluded and air insufflated through the colonoscope to identify an air leak of the anastomosis, which is merged in irrigation fluid. In case of an air leak, the anastomosis should be fashioned again given adequate distal length after a sigmoid colectomy. The rectum may have to be further mobilized as described in the proctectomy chapters.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








