Fig. 14.1
Port configuration. Hand port: right hand, C: 5 or 12 mm camera port, L1: 5 mm working port left hand, 12 mm if endoscopic stapler is used, L2: optional 5 mm port for superior splenic flexure mobilization, L3: optional 5 mm port for lateral splenic flexure mobilization
If the HALS device is placed in the periumbilical location, the camera port is moved to a 5 mm trocar in the suprapubic location (see port configuration in Fig. 14.2). The other working trocars are placed similarly as above.
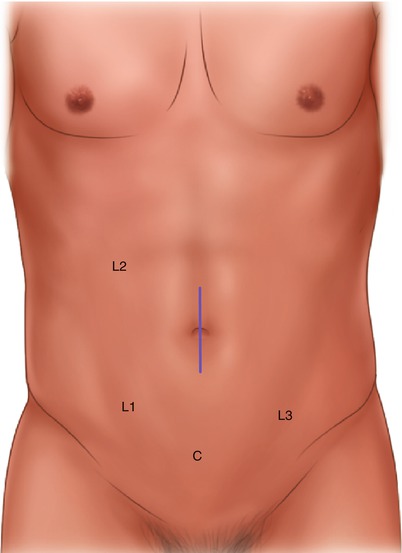
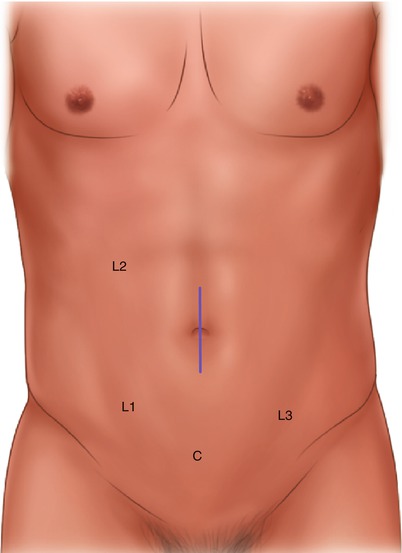
Fig. 14.2
Port configuration. Hand port: left hand, C: 5 mm camera port, L1: 12 mm working port right hand, L2: optional 5 mm port for superior splenic flexure mobilization, L3: optional 5 mm port for lateral splenic flexure mobilization
Box 14.3. Tip
For a virgin abdomen, a hand port can be placed directly through an open incision, thus avoiding potential complications of initial trocar placement.
Operative Steps (Table 14.1)
Table 14.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Exploratory laparoscopy and insertion of the hand port | 1 |
2. Identification of the ureter and ligation of the inferior mesenteric artery | 3 |
3. Mobilization of the sigmoid colon | 2 |
4. Mobilization of the descending colon and splenic flexure with identification and ligation of the inferior mesenteric vein | 4 |
5. Transection of the sigmoid colon | 3 (intracorporeally) |
2 (extracorporeally) | |
6. Anastomosis with leak test, closure, and reinspection | 2 |
Exploratory Laparoscopy and Insertion of the Hand Port
With the operating surgeon on the patient’s right side, a laparoscope is inserted through the supraumbilical port (“peak port”) to inspect the abdomen and pelvis. In cancer cases, the peritoneum and omentum should be checked for peritoneal implants or tumor seeding. The liver should also be closely inspected for metastases. Reverse Trendelenburg positioning can be used to facilitate this if necessary. In female patients, the pelvis should be closely inspected to look for ovarian implants or metastasis. Using the left hand through the HALS port, the sigmoid colon can be palpated either to identify the tumor or the extent of muscular hypertrophy in diverticular disease. Once inspection is complete, the patient should be placed in Trendelenburg position and rotated to the right. The omentum is lifted up over the transverse colon and pushed toward the upper abdomen, and the small bowel is packed to the right side of the abdomen using either a moist lap or blue surgical towel inserted through the hand port.
Identification and Division of Inferior Mesenteric Artery
The patient is still in Trendelenburg position and rotated to the right. The small bowel is packed to the right side of the abdomen, and the base of the mesentery of the left colon is exposed. If necessary, pelvic adhesions are lysed laterally to allow traction of the sigmoid colon to expose the mesocolon medially (see Video 14.1) (Box 14.5). The surgeon’s left hand is placed in the periumbilical HALS port, and the sigmoid colon is grasped and elevated anteriorly. This allows the surgeon to visualize the inferior mesenteric artery (IMA). The mesentery distal to the IMA now under tension is scored with either scissors or the alternative energy device through the RLQ port L1 (Box 14.4). This allows air into the retroperitoneum to aid in the dissection. The left ureter is found just lateral and posterior to the IMA. The gonadal vessels are identified just lateral to the ureter. Alternatively, the surgeon’s right hand is placed in the lower midline or Pfannenstiel HALS port, the sigmoid colon elevated similarly, and the dissection continued using instruments with the left hand through the RLQ port L1 (see Video 14.2).
Box 14.4. Tip
Open the peritoneum overlying the mesorectum distal to the IMA widely, and identification and short dissection of the presacral avascular plane allows identification of the correct plane between mesocolon and retroperitoneum
Box 14.5. Tip
If the hand does not create enough tension on the colon mesentery by lifting the colon itself, it can be placed close to the dissection plane lifting the colon mesentery directly.
Occasionally, it will be difficult to identify the left ureter. In these cases, the dissection plane is often too deep and the ureter is displaced anteriorly (Box 14.6). Once the IMA and the ureter are identified, the IMA is mobilized circumferentially. Unless extremely calcific, the vessel is divided with the advanced energy device and divided close to its takeoff (see Video 14.3). Some surgeons divide the IMA with an endoscopic stapler with a white cartridge. It cannot be stressed enough that the left ureter must be identified and preserved prior to dividing the IMA (Box 14.7).
Box 14.6. Tip
If the sigmoid colon is densely adhered and pulled into the deep pelvis, these adhesions should be taken first if possible in a safe manner. Otherwise, the IMA might be pulled into the pelvis, too, and it might be difficult to find the right medial plane.
Box 14.7. Tip
If the left ureter is not identified, do not proceed with ligation of the IMA, identify the ureter from a lateral approach, or convert to an open procedure.
The IMA can also be isolated and ligated in a lateral to medial approach similar to open surgery. This approach tends to be more difficult secondary to a mobilized and redundant colon. Here, the sigmoid colon is grasped with the operating surgeon’s left hand and the colon is retracted medially. The lateral attachments are taken down as the colon continues to be mobilized medially until the left ureter comes into view. After identifying the left ureter, the colon is retracted superiorly allowing isolation and safe division of the IMA at its origin. Once the IMA is divided, the remaining mesentery of the sigmoid and descending colon can be dissected using the medial to lateral approach. Here, pneumoperitoneum aids significantly in the dissection. Again using the left hand through the periumbilical hand port, the colon is elevated creating tension in the mesentery.
Mobilization of the Sigmoid Colon
The sigmoid colon is typically mobilized just following the medial dissection plane after division of the IMA. A second option is to mobilize the sigmoid colon from a lateral approach. With the left hand in the periumbilical HALS port, the surgeon retracts the sigmoid and left colon medially. After division of the IMA, sharp dissection with either scissors or an advanced energy device is carried between the colon mesentery along the left sidewall just inside the white line of Toldt up to the level of the spleen. If the hand port is used in the Pfannenstiel location, the surgeon can stand between the legs of the patient and place the left hand through the HALS port for medial and anterior traction and use the LLQ port L3 as the working port. The surgeon can also dissect along the line of Toldt with his/her right hand through the Pfannenstiel location and use an energy device through the RLQ port L1 (see Video 14.4).
Mobilization of the Splenic Flexure
Mobilization of the splenic flexure can be performed from a lateral, medial/inferior, or superior approach (Box 14.8). These approaches do not always need to be followed strictly, and they can be combined (see Video 14.5).
Box 14.8. Tip
Avoid extensive caudad traction of the colon with the hand, and preemptively add additional trocars to avoid injury to the spleen.
Medial mobilization of the splenic flexure is naturally following the progression of the medial mobilization of the descending colon and mesentery (Box 14.9). This can easily be divided up to the splenic flexure by continuing the dissection between the colon mesentery and the retroperitoneum or Gerota’s fascia. If the right hand is used through the lower midline or Pfannenstiel incision, the dissection is often times limited through the RLQ port L1. After identification of the inferior border of the pancreas, the dissection stays anterior to the pancreas until the lesser sac is entered.
Box 14.9. Tip
The inferior border of the pancreas should be recognized during continuous medial dissection to avoid pancreatic injury.
Similarly, the lateral approach follows the lateral mobilization of the sigmoid colon. In this case, the surgeon can move in between the legs and use the left hand for retraction and an optional LLQ port L3 for dissection. Occasionally, the working port needs to be moved from a LLQ L3 to an optional LUQ port L4. As the lateral wall attachments are divided, the colon will rotate medially and the Gerota’s fascia, the tail of the pancreas, and the tip of the spleen will be exposed. It is important to stay just inside the line of Toldt during this lateral dissection. If the dissection is too lateral, the retroperitoneum is entered causing bleeding and potential injury to the retroperitoneal structures and the spleen. Coming around the splenic flexure, the omentum is released and the lesser sac entered.
The superior approach is often times used as a first step of the entire procedure. This is facilitated by the placement of a periumbilical HALS port. The transverse colon is retracted with the right hand inferiorly, and the lesser omental sac is entered using an instrument through a RLQ port L1 or optional RUQ port L2. Alternatively, the assistant’s left hand can be used for downward traction on the transverse colon using the right hand for the camera control through a LM port. The surgeon would then dissect with a right-handed instrument through the RLQ port L1 and create countertraction by lifting the omentum with a left-handed instrument through the RUQ port L2. If the HALS port is in the lower midline or Pfannenstiel location, the HALS port is not used for a superior mobilization of the splenic flexure. The assistant helps with retraction through the RUQ port L4, and the surgeon utilizes ports L1 and L2 again. The dissection is started to the left of the middle colic artery and carried around the splenocolic ligament. If the earlier portion of dissection is adequate, the surgeon should see a purple hue in the tissue on the descending colon side of the splenic flexure.
The high ligation of the inferior mesenteric vein (IMV) is optional. The initial step is to identify the ligament of Treitz. Once identified, the IMV is seen lateral to it. The vein is gently isolated, and dissection is carried out in the plane just anterior to Gerota’s fascia. Often times, this portion of the procedure is carried out laparoscopically without the use of the HALS port. However, the assistant, who is on the patient’s left side, can use their left hand through the HALS port to retract the sigmoid and left colon anterior and lateral. This allows for mobilization and division of the IMV. Once the IMV is divided, dissection is carried out laterally to the sidewall if this is not already mobilized after a superior, medial, or lateral mobilization of the splenic flexure. Care is taken to stay anterior to Gerota’s fascia. The dissection can then proceed cranially to the inferior border of the pancreas.
A high division of the inferior mesenteric vein frequently allows the descending colon to reach the pelvis further for a coloanal anastomosis, and this may again not be needed for a colorectal anastomosis.
Transection of the Sigmoid Colon
The colon can be divided endoscopically with an endoscopic stapler or opened through the HALS port if it is in the lower midline or Pfannenstiel location. If the distal transection is performed first laparoscopically, the pericolonic fat and mesentery are thinned out at the point of intended division, usually at the proximal rectum where the taeniae converge. The endoscopic stapler is inserted through the RLQ port L1. Here, the surgeon’s left hand through the periumbilical HALS port is key in positioning the rectosigmoid junction properly in the stapler. An articulating stapler is helpful but not required. The proximal division is performed through the HALS port. The sigmoid colon is brought out through the hand port, and the location of proximal transection is determined. The colon is divided, checked for back bleeding, and the anvil for a circular stapler is placed in the proximal colon and secured by tightening the purse string suture. If the distal transection is done through an open approach, the sigmoid colon loop is delivered first through the HALS port in the Pfannenstiel location and the proximal transection performed using a stapler. After open division of the remaining sigmoid colon mesentery, the descending colon is returned into the abdominal cavity. Retraction of the sigmoid colon stump through the HALS port now allows for open dissection around the distal resection margin and use of a curved GIA stapler through the HALS port.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








