Fig. 29.1
Three different options for direct cervical injection: four-quadrant options (b, c) and a two-sided option (a) (Courtesy Abu-Rustum NR, Rob L. Atlas of Procedures in Gynecologic Oncology, 2013)
29.2 Lymphoscintigraphy
A preoperative planar lymphoscintigram is obtained after the injection (Fig. 29.2). Two series of pictures are obtained: immediate “dynamic images” and subsequent “static images” to localize the nodes. Some departments prefer single-photon emission computed tomography (SPECT/CT), which allows for enhanced three-dimensional localization of “hot” nodes.
Fig. 29.2
Lymphoscintigraphy. A preoperative planar lymphoscintigram in a 70-year-old woman with endometrial serous cancer is obtained after the cervical injection
29.3 Colored Dye
Several commercially available colored dyes are available throughout the world (Fig. 29.3a–d). The technique of cervical application is the same as the application of radioactive tracer. A spinal needle or Potocky needle is used to inject a total of 2–4 ml of blue dye directly into the cervical submucosa and stroma. A tenaculum can be used to assist in the stromal injection (Fig. 29.4). The injections can be given at the 3 and 9 o’clock positions, which correspond more to the parametria and avoid blue dye staining of the bladder flap secondary to the 12 o’clock injection. It is paramount to apply the blue Dye very slowly, at a rate of 5–10 s for each quadrant. After the injection, the patient is prepped and draped in the usual sterile fashion.

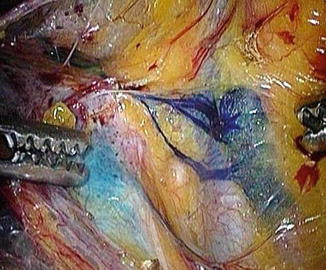

Fig. 29.3
(a –d) Isosulfan blue 1 %, methylene blue 1 %, patente blue 2.5 % sodium, and indocyanine green (ICG)
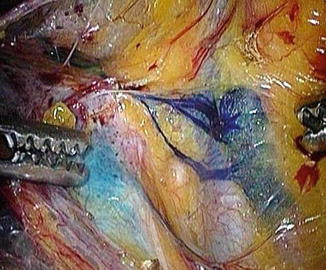
Fig. 29.4
Shows a blue right sentinel external iliac lymph node using methylene blue; blue channels can be seen leading to the lymph node
Some of the adverse effects of isosulfan blue or Patente blue include allergic reactions (<1 % of patients). Examples of such include localized swelling and pruritus of the hands, feet, abdomen, and neck. Severe reactions, including edema of the face and glottis, respiratory distress, and shock, have been occasionally reported with other similar compounds. In some instances, isosulfan blue can cause a transient drop in oxygen saturation as measured by the anesthesiologist’s pulse oximetry. Blue dyes will turn the urine blue-green for up to 24 h following injection. Contraindications include known hypersensitivity to these compounds.
The injection of isosulfan blue (Lymphazurin®) (Fig. 29.3a), Methylene Blue (Fig. 29.3b) or Patente–Blue (Blue Patente V sodique®) (Fig. 29.3c), or ICG (Fig. 29.3d) is given in the operating room at the time of the examination while the patient is under anesthesia. Isosulfan blue is a sterile aqueous solution packaged in 5 ml vials. No preparation is needed, and it can be stored at room temperature. Patente–Blue 2.5 % is a sterile solution that comes in 2 ml vials and is often diluted in 2 ml of Saline solution. Methylene blue is available in 10 ml vials at 10 mg/ml and can be injected without any preparation or dilution. ICG recently emerged as a very useful and safe dye for interstitial cervical injection and requires a near-infrared camera for visualization. ICG comes in a 25-mg dry powder vial and is mixed with 10–20 ml of sterile water in a 25-mg vial, and up to 5 mg is used directly into the cervix as well.
Figure 29.4 shows a blue right sentinel external iliac lymph node using Methylene Blue; blue channels can be seen leading to the lymph node. Figure 29.5 shows a blue right external lymph node using Isosulfan blue. Figure 29.6 shows blue lymphatic channels from the left parametria and broad ligament leading to a blue SLN in the left external iliac region. Following a cervical injection, most pelvic SLNs are located medial to the external iliac vessels, ventral to the internal iliac system, and in the superior part of the obturator space.
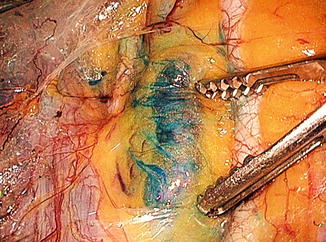

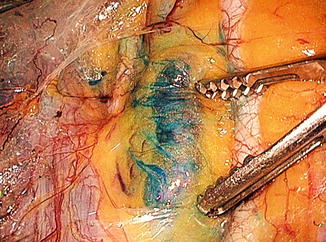
Fig. 29.5
Shows blue lymphatic channels leading into a right external iliac sentinel lymph node

Fig. 29.6
Shows afferent and efferent blue lymphatic channels with a blue left external iliac sentinel lymph node medial to the iliac artery
29.4 Discussion
The optimal technique of SLN mapping in uterine corpus cancer continues to be the subject of much debate. A cervical, hysteroscopic, and a fundal serosal injection can be utilized [2]. The cervical injection is described above, and although it may not appear rational to some surgeons to only inject the dye into the cervix when dealing with uterine cancer, it has been repeatedly demonstrated that a superficial and deep injection into the uterine cervix provides excellent dye penetration to the region of the uterine vessels and main lymphatic trunks that condenses in the parametria in the majority of cases (Fig. 29.7). The cervical injection technique is easy to utilize and has gained more acceptance in recent years. The combination of a superficial (1–3 mm) and deep (1–2 cm) cervical injection can lead to dye delivery to the main three layers of lymphatic channel origins in the cervix and corpus, namely the superficial subserosal, intermediate stromal, and deep submucosal lymphatic sites of origin [3, 4]. The dye commonly condenses around the parametria and appears in the main lymph trunks in the broad ligament and parametria and leads to pelvic and occasionally paraaortic nodes. Figure 29.8 demonstrates the most common location of SLNs after a cervical injection. Figure 29.9 demonstrates a less common location, usually seen when the lymph trunks do not cross over the obliterated umbilical and move cephalad following the mesoureter. Figure 29.10 demonstrates an example of an SLN identified by ICG during endometrial cancer surgery.

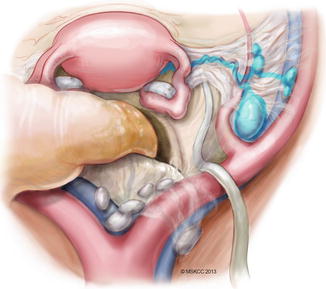
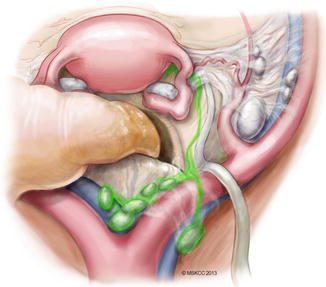

Fig. 29.7
Sentinel lymph node mapping for uterine cancer. A superficial and deep injection into the uterine cervix provides excellent dye penetration to the region of the uterine vessels and main lymphatic trunks that condenses in the parametria in the majority of cases
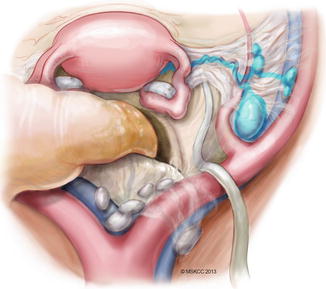
Fig. 29.8
Most common mapping topography following cervical injection of dye (©2013, Memorial Sloan Kettering Cancer Center)
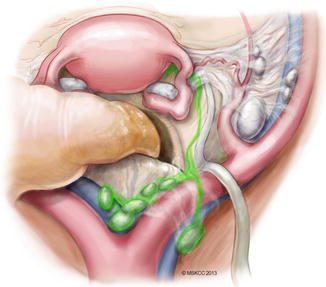
Fig. 29.9




Less common mapping topography. If the lymphatic trunks do not cross laterally over the umbilical ligament, as seen in the previous diagram, but instead drain cephalad and located in the mesoureter, this usually indicates that the sentinel lymph node will be located in the common iliac and presacral regions (©2013, Memorial Sloan Kettering Cancer Center)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








