, Said Abdallah Al-Mamari1 and Salim Said Al-Busaidy1
(1)
Urology Department, The Royal Hospital, Muscat, Oman
29.1 Prostate Cancer
1.
An 88-year-old man develops castration-resistant prostate cancer (CRPC) after bilateral orchidectomy and flutamide (Casodex®). Androgen withdrawal was attempted with no symptomatic or biochemical improvement. Magnetic resonance imaging (MRI) was performed for persistent back pain which revealed collapsed T8 and T9 vertebrae without neurological compression or evidence of bony or other metastases.
What will be your oncological management?
Does the skeletal status influence your management?
2.
A 56-year-old man with a PSA of 1.22 ng/ml has a routine digital rectal examination (DRE) revealing a nodule in the apex of the left prostatic lobe. What is your management?
3.
A 73-year-old man with a clinical prostate cancer T1b has a progressive rise of the PSA reaching 9 ng/ml. A robotic-assisted laparoscopic prostatectomy was performed and the histopathology was reported: pT3b (involving the right seminal vesicle). Surgical margins were negative (R0). The patient was warned about the risk of disease recurrence and advised immediate adjuvant radiotherapy but refuses. PSA 6 months post-operative was undetectable. What is your management?
4.
A 68-year-old patient has a rapid increase of the PSA, rising to 8.7 ng/ml. He has no LUTS. The prostatic biopsy shows a core positive at the apex on the left lobe, GS: 6 (3 + 3).
He is known to have a severe cardiomyopathy with echocardiography showing 20 % left ventricular ejection fraction. What is your management?
5.
A 74-year-old man was treated with EBRT for PC confined to the prostate as defined by pelvic MRI (initial PSA 25 ng/ml). On follow-up his PSADT was 5 months and a salvage cryotherapy was performed after negative bone scan and F-choline-PET scans suggesting confined disease. What is your management?
6.
A 67-year-old man had radical prostatectomy performed and this histopathological report (HPR): prostate adenocarcinoma pT3bN0, Gleason 3 + 4. His chest, abdomen and pelvis MRI was normal. Bone scan is also normal. What is your further management?
7.
A 68-year-old patient is on active surveillance with a cT2a PC, Gleason 6 (3 + 3), and PSA 6. The PSA rises to 15 on follow-up. MRI: One LN metastasis. What is your management?
8.
A 56-year-old man had RP with PLND. HPR: pT3bN0, negative surgical margins. His PSA was undetectable in the follow-up, but rose to 0.13 ng/ml 3 years post-surgery.
What is your plan?
9.
A 48-year-old man has PSA 10 ng/ml, GS 9 (4 + 5) and a cT3N1. MRI shows involvement of the right seminal vesicle (VS) and a pelvic CT-scan reveals enlargement of a pelvic LN. Isotope bone scan is normal. What is your management?
10.
A 66-year-old man with PC GS 7 (3 + 4), PSA 15. MRI: T3b left seminal vesicle. Biopsy: All 12 biopsies are positive. What is your management?
11.
A 60-year-old man with family history of PC comes for a screening which reveals a PSA of 4.5 ng/ml with F/T ratio of 25 %. He has a normal MRI. Does he require a prostatic biopsy?
12.
A 65-year-old man has a PC with GS 7 (3 + 4), 2+/12 (2 biopsies positive out of 12), both at the right base, PSA 6.66 ng/ml. MRI: T3b (both VS are involved). Your management?
13.
A 56-year-old man with a PSA of 1.22 ng/ml and a nodule felt in the apex on the left side has a TRUS-guided prostatic biopsy revealing a 6-mm tumour, Gleason’s score 6 (3 + 3), 1+/12.
The MRI shows a peripheral lesion on the left lobe. No regional extension.
What are the possible treatment options?
14.
A 70-year-old sexually active man has a PSA of 3. DRE: suspected nodule on the right lobe. Biopsy: 3+/12 right apex and left mid-pole, GS 7 (3 + 4). MRI: Lesion limited to the apex, no capsular infiltration.
What is the clinical stage of this tumour and the d’Amico risk group?
What is your management?
Does the patient need a PLND?
15.
An 81-year-old man had radical prostatectomy in 2003 and the HPR was: pT2b, GS 6 (3 + 3), R0. Then he had biochemical and local failure in 2006 for which an RT was done. Again he developed a local failure and biochemical recurrence in 2009. He was started on HT with Casodex®. Again Casodex® was given in 2013 because of elevated PSA. Despite Casodex® the PSA continued to rise again to 2.4 ng/ml. The testosterone level was 15 ng/dL. The patient had no pain. CT-scan: Iliac LN enlargement was seen. Bone scan: There is one lesion at the left sacro-iliac joint. What is your subsequent management?
16.
A 65-year-old man is known to have a PC since 2007: 2 mm tumour of GS 5 (3 + 2). He was kept under AS since then and his PSA started to rise progressively from 3.96 → 12 → 18 → 19. He had a repeat biopsy in 2013 which showed no tumour! He has voiding difficulty due to a prostatic adenoma. A comparison of an MRI performed in 2007 and repeated in 2014 showed a similar sized (5 mm) tumour at the left base.
What is your conclusion?
What is your further management?
17.
A 58-year-old man has a PSA 9 and prostatomegaly of 120 cc. Biopsy shows 2 microfoci of less than 2 mm each in the mid prostate and the apex and GS 6 (3 + 3). MRI shows a lesion in the left posterior aspect of the prostate. What is your management?
18.
A 70-year-old man has a clinical T3b PC with PSA 16 and GS 9 (4 + 5). He has radio-hormonotherapy. A follow-up choline-PET showed a local recurrence 6 months later for which he had a salvage prostatectomy + PLND. The HPR is pT3b Nx, GS 9 (but now 5 + 4). The PSA 3 months after surgery was 3 (same level as pre-operatively).
Why does the report state Nx despite performing PLND?
What is the further management?
19.
A 66-year-old patient is known with prostatic enlargement and a PSA of 3 which has risen to 6.89 on follow-up. The prostate volume is 60 ml. DRE is normal. He has a TRUS-guided biopsy of the prostate with the HPR: Gleason 6 (3 + 3) in 2 cores: 6 mm at the apex and 2 mm at the base. What is your management?
20.
73-year-old man with a rising PSA from 3 to 8.63 ng/ml over a 3-year period. No urinary symptoms. Past history: L3-L4 surgery for disc prolapse. Biopsy: GS 8 (4 + 4) with 9 mm total tumour length in all biopsies, perineural infiltration by the tumour, prostatic capsule involved. MRI: cT3a. Bone scan: L3 isotope hyperfixation. What is your management?
21.
A 66-year-old man is a known case of PC: T3b, GS 7 (3 + 4), PSA 10; had combined RT + HT in 2005. The PSA fell. Then in 2007: the patient had urinary infection and the PSA rose to 8. The patient was treated with antibiotics and again the PSA fell to 4. He had TURP performed in 2007 for prostatomegaly and voiding difficulty. Now again PSA has reached 8. The patient develops recurrent retention of urine. What is your management?
22.
A 73-year-old man is known to have a prostate cancer. GS 7 and PSA 11. Biopsy: 7+/12. He had RP done in 2005. On follow-up he had a rising PSA and a CT-scan showed a single costal metastasis as well as a 33-mm supra-pubic pre-vesical soft tissue mass at the midline, infiltrating the recti abdominis muscles (Fig. 29.1). Both lesions and the PSA progress on follow-up despite Casodex® + Decapeptyl. The patient is asymptomatic. What is your management?
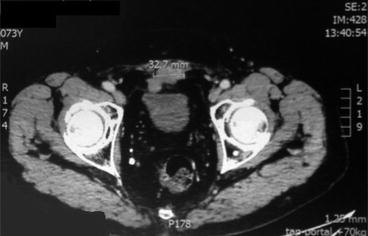
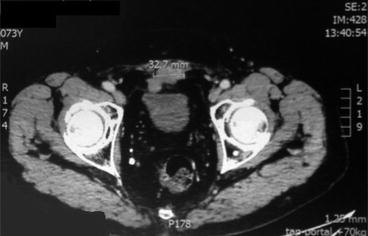
Fig. 29.1
23.
A 63-year-old man has a PC with PSA 9, GS 6 (3 + 3) and T2b right side. The capsule is invaded but no tumour beyond. What is the d’Amico risk group and what is your management?
24.
A 68-year-old man had RP done in 2011. HPR: GS 7, pT3aR1NX (positive margin at the apex right side). No PLND done. Undetectable PSA following surgery. Then rose to 0.21 in August 2014 (confirmed on repeat test). A bone scan is negative. MRI is also negative. The patient is asymptomatic. What is your impression and management?
25.
A 59-year-old man had RP with GS 7. He had a local failure after 1 year for which a salvage RT was performed. He is now developing bony and nodal metastases but he is still in good general condition. DRE was negative. He has already received five lines therapy: Abiraterone (Zytiga)® → docetaxel → estradiol (Estrana)® → estramustine (Estracyst)® → enzalutamide (Xtandi)®.
The PSA is rising despite Xtandi and the patient remains asymptomatic. Now PSA is 355.
Your management?
26.
A 59-year-old man with PSA 6.7 has two biopsies +/12 in the apex on the right side with GS 6. IRM: 2 mm long tumour. What are the possible managements here?
27.
A 75-year-old patient had RP 12 years ago. On follow-up he developed a biochemical failure after RP. MRI shows an isolated single 8-mm lesion in the prostatic bed near the urethral sphincter with no other metastases. What is your management?
28.
A 64-year-old man is a regular long distance bicycle rider. He is found to have a PSA 7. He is asymptomatic. DRE: 50 g prostate, no nodule felt. He had a repeat PSA: 1.87. A third PSA was performed due to increased anxiety and was again high 6.5. He had an MRI which showed a 4-mm lesion in the left lobe. On biopsy there is a HGPIN in 2/12 at the base and apex. What is your management?
29.
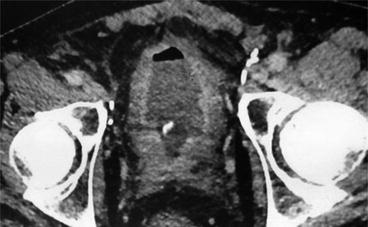
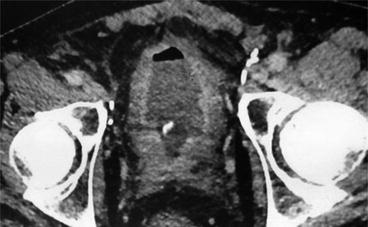
A 65-year-old man is a k/c/o PC with RT performed 1 year ago. Now complaining of dysuria for several months and found to have recurrent UTIs. Had pelvic CT shown in Fig. 29.2. What is your differential diagnosis? Discuss the further management.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







