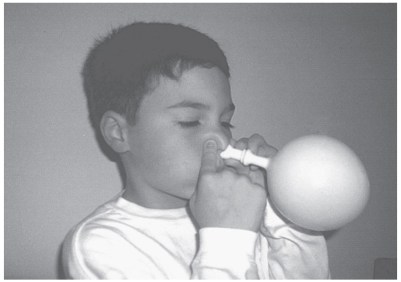
CHAPTER 9 ROLE IN MANAGEMENT OF MIDDLE-EAR DISEASE Knowledge of the role that the dysfunctional ET system plays in the pathogenesis of middle-ear disease and disorders is essential for effective management. The chapter includes • The role of the ET in the prevention and management of diseases and disorders, both nonsurgical and surgical treatment options for acute otitis media, otitis media with effusion, and tubal dysfunction and obstruction, including barotrauma or the patulous tube. • The possible contribution of ET dysfunction in the persistence of middle-ear effusion following an episode of acute otitis media, despite apparent sterilization of the bacterial infection by appropriate and adequate antimicrobial therapy. • The rationale for placement of tympanostomy tubes and explanation of why post-tube otorrhea occurs and its management. • The value of understanding ET function and tests of function in the decision-making process to remove the tubes. • Detailed description of a surgical procedure to close the middle-ear end of the patulous ET. • See Chapter 10 for other disorders related to tubal dysfunction, such as atelectasis of the middle ear, retraction pocket, and some aspects of acquired cholesteatoma, perforation of the tympanic membrane, and chronic suppurative otitis media. Some specific management options to treat and prevent otitis media and certain related conditions are related to ET dysfunction, whereas others are not. An understanding of the role that tubal dysfunction plays in the currently available nonsurgical and surgical options can be helpful not only in the decision-making process to treat or not to treat but also the reasons for complications of treatment, such as post–tympanostomy tube otorrhea. From evidence-based clinical trials, some options have been shown to be effective, whereas others have yet to be scientifically proven. Thus, an understanding of the role of the tube in the pathogenesis of the disease can provide a rationale for specific treatment options, even if proof of efficacy is lacking (see Chapter 6, “Pathogenesis”). Role of the ET System in Nonsurgical Management Of the nonsurgical methods to treat and prevent otitis media, only some are related directly to the tube, such as inflation of the tube and middle ear. Others are probably not, such as antimicrobial therapy, because the goal of antibiotics is to sterilize the bacterial infection of the middle ear and resolve the middle-ear effusion.1 On the other hand, related to prevention of otitis media, antibiotic prophylaxis may prevent bacterial infection of the nasopharynx, but there is no proof that prophylaxis targets the ET; however, there are risk factors for otitis media that can be related to ET dysfunction that can possibly be eliminated or reduced. Management of Risk Factors for Otitis Media Related to the ET System As described in Chapter 2, “Epidemiology,” there are certain risk factors for otitis media that are evidence based that are related to the tubal system. Others may be related to the system but currently lack convincing proof. Still others are unrelated, such as impaired immunity and a lack of breast-feeding. As listed in Table 2–3, risk factors that are related to otitis media may or may not be altered. For example, it is well documented that the infant tube has an immature structure and function, compared with the adult tube, but only growth and development will improve this risk factor in babies and young children (see Chapter 3, “Anatomy,” and Chapter 4, “Physiology”). Likewise, certain racial groups, such as the Aborigines of Australia and the certain Native and Inuit populations of North America, are known to be at high risk of otitis media. They are also at risk of developing perforation of the tympanic membrane and chronic suppurative otitis media, which may be related to several risk factors, one of which has been shown in the Apache to be a patulous or semi-patulous ET.2 It is not possible today to change the status of the structure of the tube in these high-risk special populations. Even though future research may uncover the underlying cause of the genetic predisposition for otitis media to be related, to some degree, to dysfunction of the ET, currently, there is no remedy. FIGURE 9–1. Proposed pathophysiology of an infant sucking on a pacifier when there is nasal obstruction, such as owing to an upper respiratory tract infection (the Toynbee phenomenon). On the other hand, there are potential inflammatory and abnormal pressure-related factors that can influence the ET system and be eliminated or reduced. The presence of an upper respiratory tract allergy, smoking in the household, and attendance in child day care are all known risk factors that can potentially cause inflammation of the ET system that can be eliminated (smoke exposure), treated and controlled (allergy), or modified (attending a day-care center with as few children as possible or no day care). But nothing can be done about the number of children in the family (and, as in day care, as the number of children increases, the rate of otitis media rises) or sibling order (the youngest are most affected). However, the use of a pacifier, thumb sucking with the nose closed, and sucking on an unventilated baby bottle are related to middle-ear disease in the infant, which is probably due to the development of abnormally high nasopharyngeal pressures adversely affecting the tube. Figure 9–1 shows my explanation of the effect of sucking on a pacifier when there is nasal obstruction (upper respiratory tract infection), which I have termed the Toynbee phenomenon (see Chapter 5, “Pathophysiology”). These activities can be eliminated. Even though a cause-and-effect relationship is lacking, gastroesophageal reflux has been associated with otitis media in children, and this is another potential cause of inflammation of the nasopharyngeal end of the ET system that can possibly be controlled by positioning of the child during and immediately after feeding, diet, and medical treatment (see Management of Gastroesophageal Reflux Related to the ET System). Medical Management of Otitis Media Related to the ET System Unfortunately, no medical treatments have been proven to be effective in improving the function of the ET in the human or animal when acute otitis media or otitis media with effusion is present. Likewise, none have proven to be effective in improving obstruction of the tube to prevent these diseases. Theoretically, because in individuals with preexisting tubal dysfunction, an upper respiratory tract infection can progress to tubal obstruction (partial), followed by middle-ear underpressures and otitis media with effusion3 or acute otitis media,4 medical treatment of the ET at the initial stage of infection could prevent this cascade of events. There is evidence that a viral upper respiratory tract infection can cause pathologic changes in the tube. In the chinchilla animal model, an experimental influenza A virus infection of the nasopharynx revealed histopathologic changes in the ET lumen (see Chapter 6).5 The following are some of the studies in animals and humans that have addressed potential medical treatments directed at the tube for treatment and prevention of otitis media. Table 9–1 summarizes studies that have evaluated the effect of medical treatments on tubal function in various animals.6–16 Table 9–2 summarizes studies that have assessed the effect of medical treatments in humans.6, 17–30 Systemic Decongestant and/or Antihistamine Treatment? In an early limited (small sample size) study by Miller, 13 children who had had tympanostomy tubes in place had a small Foley catheter inserted into the external auditory canal.17 The ability to equilibrate applied negative middle-ear pressure during swallowing was assessed following oral administration of a decongestant (carbinoxamine maleate and pseudoephedrine hydrochloride) in a double-blind, placebo-controlled clinical trial. Of the 13 subjects, 5 responded to the drug, but none of the subjects responded to the placebo. In a later randomized, double-blind, placebo-controlled clinical trial, systemic pseudoephedrine hydrochloride was not effective in the prevention of otitis media with effusion following antibiotic treatment of acute otitis media or in the treatment of the middle-ear effusion that occurred; subjects who had an allergic history did significantly worse on the decongestant.18 At our center, we assessed the effect of an oral decongestant with or without an antihistamine on the ventilatory function of the tube. Two separate studies were conducted in 50 children who had chronic or recurrent otitis media with effusion and in whom tympanostomy tubes had been inserted previously. The first was a double-blind study that compared the effect of an oral decongestant, pseudoephedrine hydrochloride, with that of a placebo in 22 children who had an upper respiratory tract infection during an observation period.21 Certain measures of ET function were significantly elevated above baseline values during the upper respiratory tract infection, which was attributed to intrinsic mechanical obstruction of the tube. It was found that oral decongestants tended to alter these measures of tubal function in the direction of the baseline (before upper respiratory tract infection) values. Even though the effect was statistically significant, the favorable changes in measurements of tubal function were only partial and were more prominent on the second day of the trial, after the subjects had received four doses of the decongestant. However, the administration of a nasal spray of 1% ephedrine had no effect on ET function in these children. TABLE 9–1. Effect of Medical Treatments on the Function of the ET in Animals In a second part of the clinical trial described earlier, a double-blind crossover design was employed. In this study of 28 children who did not have an upper respiratory tract infection, the effect of a decongestant–antihistamine combination (pseudoephedrine hydrochloride and chlorpheniramine maleate) was compared with that of a placebo. When the subjects were given the decongestant–antihistamine medication, there were favorable changes in certain ET function measures that were not observed when the children received the placebo. Again, the response differences between the two groups were statistically significant. These two studies indicated that an oral decongestant appeared to favorably affect the ET function of children who had an upper respiratory tract infection and that the combination of an oral decongestant and antihistamine had a similar effect on tubal function in children without an upper respiratory tract infection. However, an evaluation of the efficacy of these commonly employed medications had to await the results of randomized clinical trials in children with otitis media with effusion. At our center, we conducted two large randomized clinical trials that evaluated the efficacy of a then-popular combination of decongestant-antihistamine for treatment of otitis media with effusion in over 1000 children. A double-blind, placebo-controlled, randomized clinical trial of an oral suspension of pseudoephedrine hydrochloride and chlorpheniramine maleate combination in 553 infants and children with otitis media with effusion showed no efficacy of these drugs.31 In addition, side effects such as irritability and sleepiness were more common in children in the drug group than in subjects who received the placebo. In a follow-up to this trial, we wanted to determine if this combination of decongestant-antihistamine would be effective if we added an antibiotic. Mandel and colleagues reported that amoxicillin was effective, compared with placebo, in the treatment of otitis media with effusion, but the addition of the combination of the oral decongestant and antihistamine to amoxicillin provided no additional benefit over amoxicillin alone; more side effects were noted in children who received the decongestant and antihistamine combination.32 After these reports were published in the 1980s, the use of systemic decongestant-antihistamine combinations for otitis media fell sharply. We did not specifically recruit children who had allergic rhinitis in these two trials. Stillwagon and colleagues recruited 10 adult volunteers who had ragweed allergic rhinitis and underwent progressive intranasal challenge with ragweed pollen out of the ragweed season.33 Before the challenge, the subjects received chlorpheniramine maleate and phenylpropanolamine or placebo in a double-blind, randomized, crossover design. All of the subjects had objective measurements of nasal and ET function before and after the challenge. The investigators found a beneficial effect of the drug therapy on nasal and tubal function compared with placebo. They concluded that there is a role for antihistamine-decongestant treatment of allergic rhinitis, as well as of potential allergen-induced ET dysfunction. Thus, there may be a beneficial effect on the ET system in patients who have allergic rhinitis and tubal obstruction or even otitis media. In a recent placebo-controlled trial at our Center, Teixeira and co-workers found a statistically significant decrease in the rate of transmucosal nitrous oxide exchange for the middle ear with oral pseudoephedrine.19 Topical Decongestant Therapy? At our hospital, we evaluated the effect of a topical nasal decongestant spray on ET function in 40 children with tympanostomy tubes. Five tubal function variables were assessed by a modified-inflation test and forced-response test before and after the nose was sprayed with either oxymetazoline hydrochloride or placebo, according to a double-blind study design. The results showed no significant differences between the two treatment groups of the study children who had severe functional tubal dysfunction, as documented by constriction of the ET lumen during swallowing (see Chapter 5).34 In another clinical trial, Jensen and colleagues applied topical xylometazoline chloride to the middle ear end of the tube through a perforation in older children and adults and found an effect only at unphysiologic high pressures.24 Turner and Darden conducted a randomized, double-blind, placebo-controlled clinical trial that evaluated the effect of phenylephrine hydrochloride nose drops versus normal saline (control) on middle-ear pressure in infants who had an upper respiratory tract infection.23 They reported that there was no effect from the decongestant on the abnormal middle-ear pressures. In a 2015 clinical trial using a pressure chamber, Meyer et al. concluded that xylometazoline nasal spray might have a minor effect during active and passive pressure equalization.27 TABLE 9–2. Effect of Medical Treatments on the Function of the ET in Humans AOM = acute otitis media; ETF = Eustachian tube function; OME = otitis media with effusion; TM = tympanic membrane; TT = tympanostomy tubes; URI = upper respiratory tract infection. Interferon-β Serine? The effects of recombinant interferon- serine were evaluated in 38 healthy adult volunteers who had experimental rhinovirus colds.28 Tympanometry revealed abnormal middle-ear pressures in at least one ear during 18% of observations in recipients who received interferon compared with 38% of observations in those who were in the placebo group. The findings suggested a possible role for antiviral therapy in altering the ET–middle-ear dysfunction during the course of a viral upper respiratory tract infection. Rimantadine Treatment for Viral Upper Respiratory Tract Infection? In a randomized, double-blind, placebo-controlled study at our center, 105 susceptible adult volunteers had a nasal challenge with a rimantadine-sensitive strain of influenza A (H1N1) virus, followed in 2 days by 8 days of oral rimantadine treatment. Even though the rimantadine-treated group had less virus shedding, symptom load, and sinus pain compared with the placebo group, there were no differences between the two groups in nasal patency, mucociliary clearance, nasal signs, or symptoms and signs of otologic disease.35 The investigators concluded that the outcome of this study does not support treatment with rimantadine to prevent the otologic manifestations of an upper respiratory tract infection caused by influenza A. Surfactant? As described in Chapter 4, surface tension–lowering substance has been identified in animal models.6,36,37 In experiments in the guinea pig38 and the gerbil,8 surfactant reduced the ET opening pressure. In an experiment in the monkey, new assessments (compliance, hysteresis) of tubal function were used to evaluate the effect of surfactant on tubal function, which suggested that surfactant therapy may be successful only in stiff, inelastic tubes.39 In an even more recent series of experiments, Chandrasekhar and Mautone assessed the effect of intranasal aerosolized surfactant versus propellant (control) on the function of the ET in gerbils and mice.10 They reported that surfactant significantly reduced the passive opening pressure, whereas the control substance did not. Intranasal Topical Decongestant and Cortisone? Recently, Gluth and colleagues (2011)30 failed to find an effect with triamcinolone nasal spray on 91 patients with ET dysfunction. Despite the disappointing outcomes in most of the studies cited earlier, there may be an advantage to aggressively trying to prevent the tubal inflammatory stage at the onset of a viral upper respiratory tract infection, similar to preventing ET obstruction and barotrauma during air flight (see Otitic Barotrauma [Barotitis]). Even though oxymetazoline hydrochloride could not be shown to be effective by Lildholdt and colleagues,34 presumably owing to the preexisting severity of the subject’s ET dysfunction, I recommend spraying the drug into each nasal cavity (two sprays), waiting 5 minutes, spraying again (two sprays), waiting another 5 minutes, and then spraying with an intranasal topical aqueous hydrocortisone (two sprays). My rationale for this method of treatment is to first decongest the intranasal cavities; the second spraying 5 minutes later is an attempt to decongest the nasopharyngeal end of the tube. The topical hydrocortisone has two potential effects: as an anti-inflammatory agent and to prevent the rebound phenomenon associated with prolonged use of an intranasal topical decongestant. I recommend this treatment regimen until the signs and symptoms of the intranasal viral infection are absent. It is important to start this treatment when the signs and symptoms are initially present because the study by Moody and colleagues showed (by tympanometry) that middle-ear underpressures were present prior to the onset of the signs and symptoms of a viral upper respiratory tract infection.40 My recommendation is based on anecdotal experience and not from proof of efficacy from a clinical trial. I am convinced from personal experience that the signs and symptoms of paranasal sinusitis can be prevented at the onset of a viral upper respiratory tract infection in some patients (including me) by using this regimen. Summary of Medical Treatments As described earlier, there have been many medical treatments reported that attempted to improve ET function. But none have been proven to be safe and effective in randomized clinical trials with an adequate sample size that meets current scientific standards.41 Chapter 11, “Future Directions,” provides some research goals related to possible medical treatments that have potential merit. Inflation of the Middle Ear Several methods have been recommended in the past in which air is forced into the ET and middle ear–mastoid in an effort to equalize intratympanic underpressures and eliminate middle-ear effusion. The first methods advocated were those of Valsalva and Politzer.42,43 Also, catheterization of the ET through the nasal cavity has been used for over a century. Most recently, a balloon attached to a nasal tube has been invented. All of these methods are discussed in detail later. Rationale for Inflation There is theoretical merit for inflation of the ET–middle-ear system. Figure 9–2 shows the flask model of the nasopharynx–ET–middle-ear system (see Chapter 4). Liquid is shown in the body and narrow neck of an inverted flask. Relative negative pressure inside the body of the flask prevents the flow of the liquid out of the flask. This is analogous to an effusion in a middle ear that has abnormally high negative pressure. If air is insufflated up into the liquid, through the neck and into the body of the flask, the negative pressure is converted to ambient or positive pressure and the liquid will flow out of the flask. If the liquid is of high viscosity, however, the likelihood of air being forced through the liquid into the body of the flask is remote, especially if the thick liquid completely fills the chamber. Also, a thick, viscid liquid will not flow as readily as a fluid that is thin and less viscous. Therefore, in the human system, a thin, serous effusion would be more likely to flow out of the middle ear and out of the tube than would a thick, mucoid effusion that fills the middle ear and mastoid cavities. The method is probably not effective in maintaining normal middle-ear pressure in children who have atelectasis caused by tubal obstruction (i.e., high negative pressure) because experiments in animals have shown inflation of the middle ear not to be effective.44,45 FIGURE 9–2. Flask model of theoretical rationale for inflation of air into the middle ear–mastoid through the ET. The flask can be likened to the tubal system: the bulbous portion of the flask is the middle ear and mastoid and the narrow neck of the flask is the ET. When a liquid is in the bulbous portion (middle ear–mastoid), a relative negative pressure develops as the liquid flows into the narrow neck (ET). When air is forced into the bulbous portion, the negative pressure is equalized, or positive pressure is in the body of the flask, which facilitates liquid flow out of the flask through the narrow neck. Methods of Inflation In theory, inflation of the tube and middle ear should be an effective treatment option for patients with otitis media, ET obstruction (abnormal middle-ear pressures), or both. In reality, there are several problems with this method of management. VALSALVA’S MANEUVER The method of Valsalva is well known to pilots and scuba divers, who frequently use it to inflate the middle ear during descent. Valsalva’s maneuver is highly successful in most instances, but it is somewhat difficult for children to learn because it is a self-inflation technique that involves forced nasal expiration with the nose and lips closed (Figure 9–3).42 Valsalva’s method may be enhanced by first spraying the nasal cavities with topical oxymetazoline, waiting 5 minutes, spraying a second time, waiting another 5 minutes, and then performing Valsalva’s maneuver. This method is not very feasible or successful in children. Cantekin and colleagues tested 66 children between the ages of 2 and 6 years who had had chronic or recurrent otitis media with effusion and who had functioning tympanostomy tubes in place.46 They asked each subject to try to blow his or her nose with the glottis closed. None of these children could passively open their tubes and force air into the middle ear by Valsalva’s method, even though they developed a maximum nasopharyngeal pressure of 538.8 + 237.0 mm H2O. It was concluded that Valsalva’s method of opening the ET in this age group was not successful owing to possible tubal compliance problems. Unfortunately, children in this age group have a high incidence of otitis media; for infants, who have the highest incidence of otitis media, the procedure cannot be used at all. POLITZERIZATION Adam Politzer described a method of opening the ET that involves inserting the tip of a rubber bulb into one nostril while the other nostril is compressed by finger pressure and then asking the patient to swallow while the rubber bulb is compressed (Figure 9–4).43 Some individuals, especially children, complain of a sudden “pop” in the ear as the positive pressure is forced through the ET and have discomfort with the procedure. This method is also extremely difficult to perform in infants. FIGURE 9–3. Valsalva’s maneuver for inflation of the ET–middle ear. FIGURE 9–4. Politzerization method of inflation of the ET–middle ear. Politzerization was popular in the early part of the twentieth century among otolaryngologists as an office procedure. They used compressed air attached to a nasal olive tip to force air into a nebulizer, in an effort to inflate the middle ear and to insufflate medicines into the middle ear. One fairly popular agent in the past was chlorobutanol, but neither this rather obscure drug nor any other has ever been proven to be safe and effective in treating middle-ear effusions and is not recommended for clinical use at this time. Nevertheless, insufflating drugs into the middle ear may have merit in the future if they can be proven to be safe and effective (see the following section). CATHETERIZATION OF THE ET Transnasal catheterization of the ET with the classic metal cannula has been used to inflate the middle ear for more than a century (Figure 9–5). Catheterization of the tube was first described by a Parisian, Deleau, in the early part of the nineteenth century for diagnostic purposes and in an effort to improve hearing.43 The first method of introducing the cannula involves applying a topical, local anesthetic into the nasal cavity. The cannula is introduced along the floor of the nasal cavity until the instrument touches the posterior nasopharyngeal wall, and then it is turned toward the midline and brought forward until it stops at the posterior edge of the nasal septum. The cannula is then rotated laterally (about 180 degrees) until it enters the nasopharyngeal end of the ET. More current methods use a rigid rod-lens telescope or a flexible fiberoptic laryngoscope inserted through the opposite nasal cavity to directly visualize the introduction of the cannula. This method is more feasible in older children and adults than in young children, and especially infants. One advantage of introducing the cannula into the ET orifice is that a medication can be insufflated or instilled into the tube and middle ear. Similar to Politzerization, medicines were introduced in an effort to cure middle-ear effusions in the early part of the twentieth century. However, no drug has been proven to be safe and effective in clearing a middle-ear effusion using this method, and it is not indicated until a drug and this method meet the current standards of safety and efficacy. On a limited experimental basis, I have used an ET cannula to instill an aqueous corticosteroid from an intranasal steroid nasal spray bottle into the middle ear of adults and have had success in clearing a middle-ear effusion. But this was only in a few “adult volunteers” who had barotitis media and who otherwise had no previous history of middle-ear disease. Thus, I do not currently recommend this treatment since it remains experimental. FIGURE 9–5. Catheterization of the ET for inflation of the middle ear. NASAL BALLOON Stangerup and colleagues described a method of autoinflation that consists of a balloon attached to a nasal tube, the Otovent nasal balloon (Abigo Medical AB, Askim, Sweden).48 The patient inserts it into one nostril and blows up the balloon through one side of the nose while the other side is closed with finger pressure (Figure 9–6). The technique can be used in adults but can be taught only to those who are 3 years of age and older (see later). In a 2013, Cochrane review of autoinflation for otitis media with effusion it was concluded that all the studies were small, of limited treatment duration and short follow-up, the low cost and absence of adverse effects it could be used while awaiting natural resolution of the effusion.49 They also recommended a possible role in primary care, and indeed Williamson and co-workers (2015) tested the effect of nasal balloon autoinflation in children in primary care who had middle-ear effusions, and found it feasible and “improved symptoms and quality of life.”50 FIGURE 9–6. Inflation of the ET–middle ear using the Otovent nasal balloon (Abigo Medical AB, Askim, Sweden). The nosepiece is tightly held into one nostril, and while the opposite nostril is compressed with finger pressure and the mouth closed, the balloon is inflated through the nose. Problems with Inflation The major difficulty with both methods is determining whether the middle ear is actually inflated by the procedure. If a patient hears a “pop” or has a pressure sensation in the ear, there is only presumptive evidence of passage of air into the middle ear. Auscultation of the ear (listening for the sound of air entering the middle ear during the procedure) is helpful in determining whether the procedure is successful, but a sound may be heard even when air does not enter the middle ear. (A Toynbee tube has been used in the past to determine if an inflation method worked; the device is a length of rubber tubing with an olive tip at either end, one for the patient’s test ear and one for the ear of the examiner.) Objective otoscopic evidence that the middle ear is actually inflated would be constituted by the presence of bubbles or a fluid level behind the tympanic membrane when these findings were not present prior to inflation. Another excellent method for determining objectively if the inflation is successful is to obtain a tympanogram before and after the procedure: the compliance peak should shift toward or be in the positive pressure zone after inflation (Figure 9–7). If none of the results of these presumptive or objective methods of determining the success of inflation are definitive, then the clinician cannot be certain that the procedure has been therapeutic. Failure to achieve a successful result may be related to • the inability of the patient to learn the method, • insufficient nasopharyngeal overpressure to open the ET passively, • ET abnormality, or • a middle ear filled with a very thick, mucoid effusion. FIGURE 9–7. Tympanometric method of documenting successful inflation of the middle ear after politzerization with air. First, the compliance peak is determined, followed by a second tympanogram after attempting inflation. If successful, the peak should be shifted toward the positive pressure zone. CLINICAL TRIALS Unfortunately, the beneficial effect of the Valsalva and Politzer methods of inflation for treatment of otitis media with effusion or atelectasis has been subjected to only a limited number of randomized controlled trials. Most of the evidence has been anecdotal until recently. Gottschalk claimed to have had remarkable success with a modification of the Politzer method in over 12,000 patients; the average course of treatment was a minimum of 12 inflations in the office on 3 separate days.51,52 Schwartz and colleagues showed that it is possible to inflate the middle ears of children at home by Politzer’s method; they documented the results of the method by tympanometry but did not test its efficacy.53 Kaneko and colleagues inflated the ears of 149 children who were 3 to 9 years of age and reported success related to the season, but this trial did not include a control group.54 Fraser and colleagues reported one of the first controlled trials of this method, but they were not able to demonstrate that it was efficacious.55 Chan and Bluestone also conducted a randomized clinical trial in 40 Pittsburgh children, most of whom had chronic otitis media with effusion that was unresponsive to antimicrobial treatment.56 All of the children were taught how to use the specially developed system, which consisted of a flowmeter attached to a disposable anesthesia mask, based on a modified Valsalva’s technique.57 The children were stratified according to their ability to achieve ET opening as determined by tympanometry. Subjects were randomly assigned to either autoinflation three times each day for 2 weeks or to no inflation (control). Of the 19 children who autoinflated their ears, only 1 patient (5%) was effusion free at the end of the trial, which was comparable to the control group; only 2 (10%) of 21 subjects were without middle-ear effusion (Table 9–3). We concluded that autoinflation, as conducted in the trial, was ineffective for treatment of otitis media with effusion. In a later clinical trial from Denmark by Stangerup and colleagues, however, autoinflation was considered to be effective using the Otovent nasal balloon, which the child inserts into one nostril and blows up the balloon through one side of the nose while the other side is closed with finger pressure.58 The technique could be taught only to children who were 3 years of age and older, and during the trial, many of the children failed to use the instrument the prescribed three times daily during the 2-week regimen. In those children who had type B tympanograms on entry, the investigators concluded that the tympanometric conditions were “better” in the treated group than in the untreated children at the end of the 2 weeks, but there were no statistically significant differences after 2 or 3 months between the two groups. Because the effect was “short-lasting,” they advocated repeated use. Because this study had several shortcomings—for example, tympanometry only to identify middle-ear effusion, analysis by ear and not by subject—the safety and efficacy of this device await further study, especially when used repeatedly by children who have chronic and recurrent disease. A clinical trial by Stangerup and colleagues reported success in using the Otovent in children who suffered from barotitis following air flight: 21% were relieved by Valsalva’s maneuver, but 82% could increase middle-ear pressure using the nasal balloon method.58 In a later study, Stangerup and colleagues again reported success in airplane passengers who developed barotitis during descent (see later).59 TABLE 9–3. Percentage of 40 Children with Middle-Ear Effusion Who Had Persistent Effusion 2 Weeks after Autoinflation or No Inflation (Controls) Adapted from Chan KH and Bluestone CD. Fisher’s exact test (two-tailed = 1,000) In a systematic review of 35 potential articles that addressed autoinflation for treatment of “glue ear” in children, Reidpath and colleagues concluded that the evidence for efficacy is conflicting but that future clinical trials are warranted.60 ANIMAL STUDIES In a series of studies in monkeys, inflation of the middle ears was not effective in preventing the occurrence of middle-ear effusion even when repeated over days using the inert gas argon61 and may be related to timing of the inflations to be potentially successful.62,63 A more recent study in the monkey model by Alper and colleagues revealed that inflation merely displaces the middle-ear effusion to other portions of the middle-ear cleft, which appears to be clear in the middle ear.45 Even though inflation failed in a monkey model to prevent or treat middle-ear effusion, as described earlier,45,61,64 a new clinical trial, funded by the National Institutes of Health, addressing the efficacy of this method, in addition to systemic hydrocortisone therapy, is currently being conducted at our center under the leadership of Cuneyt M. Alper, MD. Inflation for Barotitis At present, it would appear reasonable to recommend autoinflation of middle ears for prevention and treatment of barotrauma (following flying or swimming) if high negative middle-ear pressure, otitis media with effusion, or both are present. Inflation of the middle ear should be helpful under these circumstances because this condition is usually not due to chronic ET dysfunction and inflation may resolve the acute, subacute, or chronic disorder rapidly. In a clinical study by Stangerup and colleagues, the prevalence of barotitis after an airplane flight was reported to be 25% in children compared with only 5% in adults.58 They also reported that only 21% of the youngest children with middle-ear negative pressure could perform a successful Valsalva’s maneuver, whereas 82% could increase the middle-ear pressure with the Otovent. More recently, Stangerup and colleagues conducted a controlled trial of the Otovent in preventing barotitis in adults, which revealed that this method was successful in preventing middle-ear negative pressure on descent during air flight—6% in the treatment group versus 15% in the control group—and when persistent negative middle-ear pressure developed following the flight, inflation equilibrated the negative pressure in 69% of individuals who were not successful in using Valsalva’s maneuver to relieve the abnormal pressure.59 This study has merit and deserves to be tested by other investigators; future trials should also include children. Conclusions Regarding Inflation In conclusion, these procedures may be worthwhile for patients with barotitis and for those who have an occasional episode of otitis media with effusion or ET dysfunction, but they are probably not helpful in children who have chronic or frequently recurrent middle-ear effusion, atelectasis, or both (see the section on atelectasis and retraction pocket in Chapter 10). When a middle-ear effusion not due to barotrauma is found in a patient, who only occasionally has a problem and in whom frequently recurrent or chronic disease is not suspected, then the procedure may also be successful, especially if a small amount of serous effusion is visible behind a translucent tympanic membrane. It is unlikely, however, that a mucoid or purulent effusion could be evacuated by this technique, and if it could be, it would probably recur immediately after the procedure. Atelectasis of the tympanic membrane and middle ear, with or without high negative pressure, can also be treated by repeated autoinflation (Valsalva) or Politzer’s method, but even if the middle ear is successfully inflated, the benefit is usually only of short duration and the procedure must be repeated frequently. Therefore, it is unlikely that inflation will be successful in alleviating frequently recurrent or chronic tubal dysfunction for any length of time. There is also a remote possibility that bacteria can be forced into the middle ear from the nasopharynx during this procedure and the possibility that repeated autoinflation could cause the tympanic membrane to lose its stiffness (become hypercompliant). Laboratory and clinical studies are continuing in more than one center in an effort to resolve the ongoing controversy regarding the efficacy of inflation of the tube and middle ears of patients in preventing ET dysfunction or otitis media, especially when a common cold is present, and treating these conditions when they are present. Management of ET Dysfunction Even when an effusion is not present in the middle ear, signs and symptoms of tubal dysfunction can occur. Abnormal function of the ET can cause otologic symptoms despite the lack of otitis media. The symptoms can be intermittent or persistent, and the severity of the complaints can be mild, moderate, or severe. At the time of the examination, the tympanic membrane may have a normal appearance, and its mobility may or may not be impaired when tested with a pneumatic otoscope or by tympanometry; the tympanic membrane may or may not be retracted. The condition can be either of short duration (acute) or long-standing (chronic). The patient commonly will have a past history of ET dysfunction or episodes of acute otitis media, otitis media with effusion, or both. Two types of ET dysfunction can be present: obstruction or abnormal patency (see Chapters 5 and 6). Also, rapid alterations in barometric pressure, such as when flying in an airplane or scuba diving, can cause obstruction of the tube that can result in otologic symptoms (otitic barotrauma or barotitis), especially in children who have an underlying tubal dysfunction.63 ET Obstruction When obstruction of the ET is present, the tube periodically opens to regulate gas pressure within the middle-ear cavity but at less frequent intervals than normal; in this case, high negative intratympanic pressure may be present for transient or prolonged periods (acute or chronic). The obstruction of the tube can be anatomic (mechanical), functional (failure of the opening of the tube), or both. Anatomic obstruction may be due to infection or allergy or possibly adenoids. Functional obstruction is idiopathic but is due to failure of the opening mechanism, which, in turn, may be caused by floppy tubal cartilage or abnormalities of the tensor veli palatini muscle or be secondary to the yet to be determined etiology of constriction of the tube during swallowing. This type of intermittent middle-ear regulation of middle-ear pressure can cause periods of otalgia, a feeling of fullness or pressure, hearing loss, popping and snapping noises, tinnitus, disequilibrium, or even vertigo. These symptoms are more commonly encountered in older children and teenagers than in young children. Most likely, infants and young children have these symptoms but rarely complain. Frequently, patients will have otologic symptoms on awakening and then periodically during the rest of the day. When symptomatic, the patient will commonly have a retracted tympanic membrane, which will have limited or no mobility to applied negative pressure and no mobility when positive pressure is applied during pneumatic otoscopy. This indicates the presence of negative pressure in the middle-ear cavity. Tympanometry can be helpful in confirming and documenting the high middle-ear negative pressure (see Chapter 8, “Diagnosis and Tests of Function”). But a patient may have no evidence of middle-ear negative pressure at the time of the examination because the pressure can fluctuate during the course of the day. Audiometric testing will frequently reveal normal hearing, but if high negative middle-ear pressure is present, there may be a mild conductive hearing loss owing to the impaired compliance of the middle ear. This disorder is relatively common in the third trimester of pregnancy and in children during puberty, especially girls, and can be present even when a past history of middle-ear infection is absent. Management of the patient who has tubal obstruction is related to the frequency, severity, and duration of the symptoms and the underlying cause. If the condition is present only during episodes of an acute upper respiratory tract infection, medical treatment should be directed toward relief of the nasal congestion and counseling the patient and parent that the disorder will resolve spontaneously. A systemic or intranasal topical decongestant may be helpful for the nasal congestion. Inflation of the middle ear can be tried (see Inflation of the Middle Ear). I have recommended the method of sequentially spraying oxymetazoline and hydrocortisone in the nasal cavities, as described earlier for prevention, but with limited success. In my opinion, intranasal oxymetazoline is effective in preventing symptomatic barotrauma during descent in an airplane or during scuba diving (see later). When the symptoms are extremely troublesome and interfere with concentration, a myringotomy and tympanostomy tube may be required. When symptoms are of a chronic nature, a search for an underlying cause (e.g., paranasal sinusitis, nasal allergy, or hypertrophy of the adenoids) should be attempted and, if found, appropriate management should be instituted. Frequently, there is a strong family history of middle-ear disease, which implies a hereditary factor in children who have not only otitis media but also ET obstruction (see Chapter 2). If no underlying cause is uncovered, then a trial with a topical intranasal decongestant might be helpful or inflation of the ET–middle ear may be tried, but there is no evidence that these treatment options are effective for the short or long term. Unlike the clinical trials that were cited earlier when a chronic middle-ear effusion is present, there have been essentially no trials of medical treatments for the obstructive type of tubal dysfunction. Even the trials of medical treatments in humans and experiments in animals summarized in Tables 9–1 and 9–2 are disappointing. Again, I still recommend a trial of an intranasal decongestant and hydrocortisone, as described earlier, for chronic symptomatic ET obstruction that is troublesome to the patient. Recently balloon dilation of the ET has been reported to be promising,65,66,67 but as of this date there is no proof of efficacy in randomized, controlled trials using ET function as an outcome measure with long-term follow-up. When nonsurgical methods are unsuccessful and the symptoms are troublesome to the patient, then myringotomy and insertion of a tympanostomy tube may be necessary to alleviate the symptoms when the tubes are patent and functioning. This treatment is successful but is only a “bypass” for the dysfunctional tubal system. The condition, even though chronic, will usually resolve with advancing age in children, but some pediatric patients, especially adolescents, may need to have the tympanostomy tubes replaced several times, and some may even need a “permanent” tympanostomy tube. This chronic disorder can persist throughout adult life, for which long-lasting tubes are essential. Recently (2010), placing the tube under the annulus has been recommended in an attempt for long term treatment,68 but I have seen cholesteatoma at the site of insertion and thus do not advocate it. (see Myringotomy and Tympanostomy Tube Related to the ET System). When ET obstruction is chronic, sequelae such as atelectasis of the middle ear (and tympanic membrane) are possible and can progress into a retraction pocket, which, in turn, can lead to a cholesteatoma. Abnormally Patent (Patulous) ET The other end of the spectrum of ET dysfunction is abnormal patency. In its extreme form, the hyperpatent tube is open even at rest (patulous) (see Chapter 5). Lesser degrees of abnormal patency result in a semi-patulous ET that is closed at rest but has low tubal resistance to gas flow in comparison with the normal tube. A patulous ET may be caused by abnormal tubal geometry or a decrease in extramural pressure, such as occurs as a result of weight loss or, possibly, mural or intraluminal changes. These last conditions may be seen when the extracellular fluid is altered by medical treatment of another unrelated condition. Interruption of the innervation of the tensor veli palatini muscle has also been shown to be a cause of a hyperpatent tube.69 Clinically, the presence of a patulous ET is a relatively uncommon finding in adolescents and adults but is even less commonly encountered in young children. But, when present, this disorder can be misdiagnosed as tubal obstruction and inappropriately treated. The patient frequently complains of hearing his or her own breathing, voice (autophony), or both in the ear. Some patients become habitual “sniffers” because they can close the ET lumen with the self-induced nasopharyngeal negative pressure. Patients with chronic tubal obstruction can be “puffers” or use the self-Valsalva maneuver, both of which produce positive pressure in the nasopharynx in an attempt to equilibrate the negative middle-ear pressure. Otoscopic examination reveals a tympanic membrane that moves medially on inspiration and laterally on expiration; the movement can be exaggerated with forced respiration, especially with one nostril pinched closed. The condition is relieved when the patient is recumbent because mural and intramural pressure in the ET is increased by venous engorgement in this position. The patient should therefore be examined in the sitting position. The diagnosis can also be made by measuring the immittance of the middle ear.70 A tympanogram is obtained while the patient is breathing normally, and a second one is obtained while the patient holds his or her breath. Fluctuation in the tympanometric line should coincide with breathing. The fluctuation can be exaggerated by asking the patient to occlude one nostril and close the mouth during forced inspiration and expiration or by performing the Toynbee or Valsalva maneuver (see Chapter 5 and Chapter 8). Management of a patulous ET depends on first determining the cause of the problem. If the symptoms are of relatively short duration, the condition may subside without any active treatment. In children and teenagers, this condition is usually self-limited and probably due to age-related changes in the structure and function of the tube and adjacent areas secondary to rapid growth and development. Interruption of the neuromuscular component of the tube, such as from trauma or surgery, may be the cause, but more commonly rapid loss of weight is the underlying pathogenesis. In adults, a neurologic disorder may be present, but in children, the condition is most commonly idiopathic. When the symptoms are disturbing and the condition is chronic, active treatment is indicated. Myringotomy with insertion of a tympanostomy tube may be helpful in some patients, probably owing to the coexistence of obstruction and abnormal patency. But tympanostomy tube placement may exaggerate the symptoms if the tube is consistently hyperpatent. I prefer to place a tympanostomy tube prior to a more aggressive surgical procedure (described later) because the symptoms may improve, and a direct measurement of tubal function can be performed to confirm the diagnosis (see Chapter 8). Medical management of this type of tubal dysfunction has been disappointing. Insufflation of powders into the tube and instillation of 2% iodine or 5% trichloroacetic acid solution have also been advocated.71 Infusion of an absorbable gelatin sponge solution has also been suggested,72 as has injection of polytetrafluoroethylene (Teflon) into the paratubal area.73 All of these methods have major disadvantages. They are, for the most part, irreversible and may not improve the condition or may provide only temporary relief. Total obstruction of the ET can also be a complication. Stroud and colleagues suggested the transposition of the tensor veli palatini through a palatal incision, but the procedure has not been shown to be safe and effective in a large number of patients by other investigators.74 DiBartolomeo and Henry reported initial success in treating 8 of 10 patients who had patulous tubes with a new intranasal medication composed of diluted hydrochloric acid, chlorobutanol, and benzyl alcohol.75 The safety and long-term efficacy of this experimental treatment have not been confirmed.76 At present, the most logical choice for relief when the discomfort becomes severe is a procedure that would alleviate the symptoms simply, reversibly, and without untoward reactions. A technique described by Bluestone was used successfully in adults but is rarely indicated or necessary in children because the patulous tube condition is usually self-limited in this age group.77 The procedure involves placement of a plastic catheter into the middle ear end of the ET and is described in detail later.78 More recently, Oh and co-workers (2015) using a similar trans-tympanic approach but through a myringotomy incision and placing a catheter filled with bone wax in 35 ears of 29 patients and reported relief of autophony.79 The surgeons did credit my procedure as the first to introduce it. Another procedure reported 2011 placed a curvature inversion plastic tube in 11 patients.80 Otitic Barotrauma (Barotitis) Barotitis usually occurs in individuals who have ET obstruction, either functional, mechanical, or both, most frequently during periods of upper respiratory tract inflammation. AIR FLIGHT On ascent in an airplane, the normal ET opens spontaneously; there is forced opening, and the relative positive middle-ear gas pressure is equilibrated with the cabin pressure. Most commercial aircraft are pressurized to an equivalent altitude of 7000 feet. On descent, however, the ET does not open spontaneously but opens by actively swallowing owing to contraction of the tensor veli palatini muscle, which equilibrates the relative negative middle-ear pressure. Jaw movements and Valsalva’s maneuver may successfully open the ET when tubal dilation fails to occur during swallowing. If the ET is totally mechanically obstructed, which is extremely rare in children and adults, then the patient will have otalgia and barotitis on both ascent and descent. Since functional ET obstruction is the most common type of dysfunction of the tube, most individuals will have difficulty only on descent because the tube can easily open spontaneously during ascent; even infants and children without a history of middle-ear disease frequently have trouble on descent because their ability to actively open the tube by swallowing is inefficient compared with that of most adults (see Chapter 4).58 Children or adults may have little or no symptoms during flying in an airplane until they develop an upper respiratory tract infection or during a period in which their allergic rhinitis is present (inflammation of the tube is superimposed on a preexisting functional obstruction). Evidence that infants have relatively inefficient active tubal opening is noted by their crying during descent, which probably inflates their middle ears—a physiologic compensatory mechanism. Barotitis that is symptomatic and persistent is the result of the ET being persistently closed, or even “locked,” during descent (see Chapter 5).81 The tympanic membrane is severely retracted with limited or no mobility when examined with a pneumatic otoscope because high middle-ear pressure is present. The middle-ear mucous membrane can actually tear, which can result in bleeding into the middle ear (hemotympanum) secondary to the alterations in middle-ear gas pressure and the pressure in the cabin of the airplane. A middle-ear effusion can be present and is secondary to the negative middle-ear pressure. (This sequence of events is fairly good evidence of the validity of the hydrops ex vacuo theory of Politzer, but in an unphysiologic manner Professor Politzer never dreamed of in his day.) If the patient, especially a child, has a preexisting middle-ear effusion, then there is little or no movement of the tympanic membrane, and thus no otalgia on descent. If the child has had recurrent otitis media and has ET dysfunction but has no effusion, then otalgia and barotitis are possible; the symptoms are similar to those described earlier when ET obstruction is present. Indeed, Weiss and Frost evaluated 14 children, whose ages ranged from 3 to 11 years and who had middle-ear effusion in one or both ears before an air flight.82 None of the children experienced difficulty in the ears with effusion, but two of the children had symptoms attributable to barotitis in a contralateral effusion-free ear. We recommend that children who have middle-ear effusion present in both ears may fly in commercial aircraft without any preventive medication. If the child has had recurrent otitis media, however, or signs and symptoms of ET dysfunction and has no middle-ear effusion in either ear, then prevention is advisable. We recommend an oral decongestant, such as pseudoephedrine hydrochloride, prior to the flight, and a topical nasal decongestant, such as oxymetazoline, immediately before descent; administer two sprays in each nostril and then repeat with two more sprays in about 5 minutes. Most patients have little or no difficulty during descent with this method of prevention. Flying in airplanes is part of our current culture and, therefore, should not be withheld from children or adults who have middle-ear problems. Fortunately, patients who have functioning tympanostomy tubes in place have no difficulty during flying because their middle-ear pressure is always equilibrated with ambient pressure. SWIMMING AND DIVING It is uncommon for barotitis to occur during normal swimming activity in healthy individuals, but in those who have active upper respiratory tract inflammation (e.g., viral, bacterial, allergic), especially when there is a preexisting dysfunction of the ET, diving deeply into water can result in an acute barotitis media; sudden positive pressure under the water and relative negative pressure in the middle ear can result in insufflation of nasopharyngeal secretions into the middle ear (put another way, the middle ear relative underpressure aspirates the nasopharyngeal secretions) (Figure 9–8). Also, such a person may not develop an acute middle-ear effusion but may have tubal “locking” with high middle-ear pressure that can also be associated with acute otologic signs and symptoms. Even though not as rare as a complication of diving, in underwater swimming, an individual with preexisting tubal dysfunction can also develop middle-ear barotrauma during periods of inflammation of the nose and nasopharynx. Management is fairly straightforward. Keeping potential swimmers, especially children, out of the water during periods of colds or allergy is the best advice. The use of an intranasal decongestant spray prior to swimming and diving is an alternative for competitive swimmers, but for the casual swimmer, refraining from this activity is recommended. SCUBA DIVING Use of a self-contained underwater breathing apparatus (scuba) is not a common recreational activity in young children, but it is not uncommon in older children and adults. The pathophysiology during descent and ascent is similar to that described earlier during flying in an airplane, and the methods of prevention and treatment are also similar. But there are pathophysiologic differences between flying in an airplane and scuba diving, such as the adverse effect of the prone and head-down body position during immersion when scuba diving, secondary to venous engorgement of the ET and middle-ear mucosa (see Chapter 5).83 Also, Shupak and colleagues tested 42 Israeli scuba diving candidates in a pressure chamber using tympanometry to assess middle-ear pressures before and during a simulated dive.84 They concluded that the ability to autoinflate the middle ear at sea level was not a good criterion for whether the candidate could or could not equalize middle-ear pressures during the dive. Thus, it would be unwise for a recreational scuba diver who has difficulty equalizing middle-ear pressures during scuba training to continue to pursue this sport. Also, I do not recommend scuba diving for any individual who has had recurrent or chronic otitis media or ET obstruction because an adverse outcome may occur (e.g., traumatic rupture of the tympanic membrane) and may even be life-threatening if severe vertigo develops owing to inner ear barotrauma. Scuba diving is not a physiologic activity that evolved in humans, and when this activity is associated with possible severe middle and inner ear complications, it should be avoided. The enthusiast should try swimming with a snorkel because there are not the same strains on the ET system, even with “free dives” at reasonable depths. FIGURE 9–8. Diving deeply into water can result in acute barotitis media when the swimmer has an upper respiratory tract infection, especially in individuals who have a preexisting dysfunction of the ET.










Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








