Fig. 12.1
Single-dock port placement
Following placement of the robotic camera port, the remaining 8 mm port is placed in the right subcostal position, lateral to the mid-clavicular line, and will initially be used for the surgeon’s first robotic arm. Finally, the 12 mm assistant port is placed in the RLQ, as lateral as possible and just inferior to the anterior superior iliac spine. Typically, the assistant port is unable to be placed at the previously marked ileostomy site, which is usually more medial and superior to an optimally placed assistant port.
The da Vinci® robot is then docked from between the patient’s legs, in-line with the bed. The arm for the robotic camera is docked in the subxiphoid position; the first, second, and third robotic arms are docked in the right subcostal, left subcostal, and left lateral ports, respectively (Fig. 12.2).
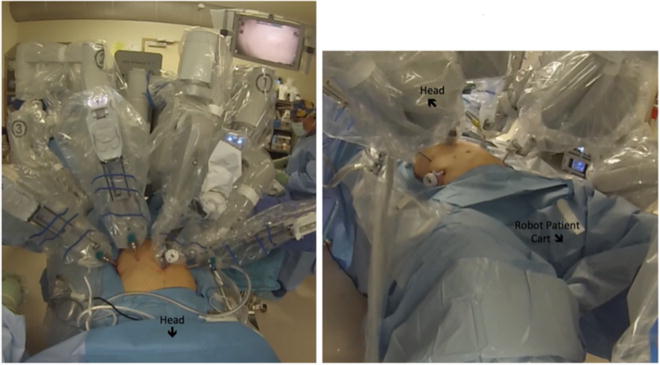
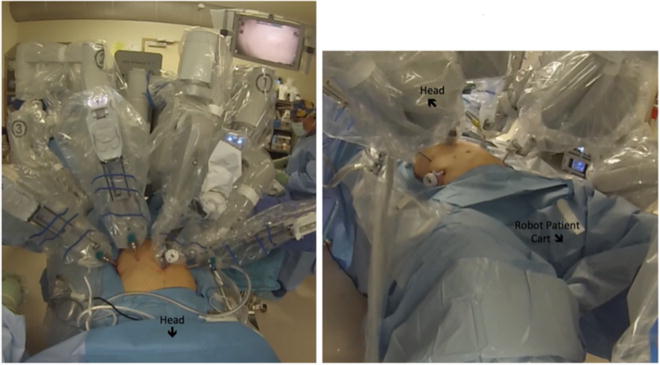
Fig. 12.2
Robotic docking in single-dock technique
12.4.4 Surgical Technique
The robotic vessel sealer and hook cautery are alternated in the surgeon’s first robotic arm, the Cadiere forceps in the second robotic arm, and a fenestrated grasper in the third robotic arm. In a female patient, the uterus can be retracted and fixed anteriorly using temporarily placed transabdominal sutures. The sigmoid colon is mobilized until the rectosigmoid junction is identified. At this point, the rectosigmoid junction is dissected and divided using a laparoscopic linear stapler via the assistant port.
The left colon is then mobilized, and left colic artery (or IMA) is divided with the robotic vessel sealer, or alternatively, by an energy device introduced through the assistant port. Dissection proceeds toward the splenic flexure, and the assistant retracts the left colon inferomedially. Once the splenic flexure is mobilized, the dissection continues up to the mid-transverse colon. Often this is accomplished by retracting the flexure and transverse colon inferiorly toward the pelvis and taking the mesentery of the colon from the side closest to the stomach within lesser sac.
Following mobilization of the splenic flexure, the dissection can continue along the transverse colon mesentery if visualization is optimal and or turn toward the terminal ileum. The ileocolic artery is identified and divided with the robotic vessel sealer or energy device via the assistant port. The assistant retracts the right colon medially and cephalad as the terminal ileum and ascending colon mobilized. The terminal ileum is then divided with a linear stapler through the assistant port.
The last part of the dissection is the mobilization of the hepatic flexure and completion of dissection of the transverse colon. This can be challenging as the camera is often placed off-center toward the right, so having the TI mobilized and the transverse colon mobilized allows the inferior retraction of the colon leftward and toward the pelvis to better visualize the flexure. The middle colic artery is identified and divided with the robotic vessel sealer or energy device through the assistant port. Additionally, the IMV or branches thereof are divided.
12.4.4.1 Anastomosis and Specimen Extraction
If an end-to-end ileorectal anastomosis is planned, the proximal end of the divided terminal ileum is grasped and brought out through the 12 mm assistant trocar site. The anvil is introduced, and a standard purse-string suture is used to secure the anvil in place prior to replacing the ileal stump into the abdomen. This can also be performed intracorporeally.
The specimen can be extracted via a Pfannenstiel incision, through an enlarged incision at an ileostomy site, or transrectally. In the former, an extracorporeal anastomosis can be performed. If an ileostomy is performed, an incision can be made at that site large enough for the specimen to be extracted. Alternatively, the specimen can be removed in a transrectal fashion. Our technique for transrectal extraction is to irrigate the rectal stump prior to proctotomy. A proctotomy is made along the staple line with robotic scissors through which a flexible endoscope is introduced into the peritoneal cavity. A looped snare is used to grasp the distal end of the specimen (usually the stapled TI), which is then extracted through the proctotomy under robotic visualization, taking care to minimize tension on the specimen and rectal stump during extraction. The robotic arms are used to hold the rectum open to facilitate extraction. The proctotomy is closed with a linear stapler, and an end-to-end ileorectal anastomosis is performed in the standard fashion using an EEA stapler.
The anastomosis is then evaluated endoscopically and a leak test is performed. The final step of the procedure is creation of a diverting loop ileostomy, if indicated. A pelvic drain can be placed through the left lateral port site.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







