Robotic-Assisted Low Anterior Resection
Vincent Obias
KEY STEPS
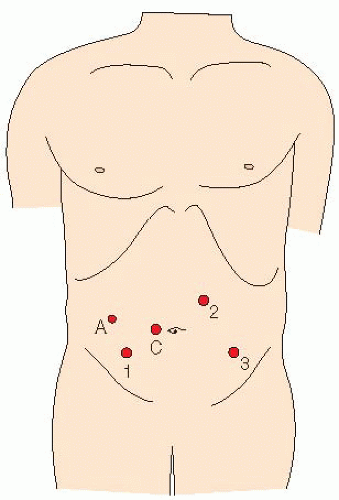
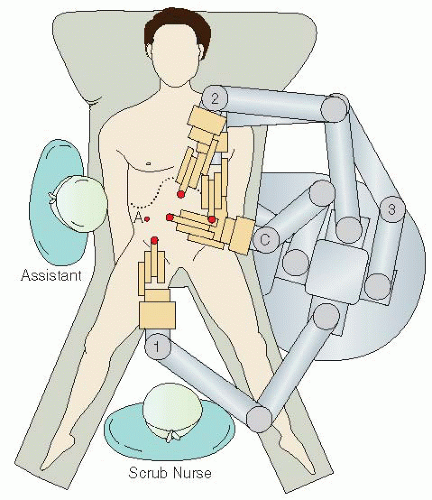
1. Insertion of ports: 12-mm port placed 2 cm to right of umbilicus with optiview after veress needle insufflation (camera port); 12 mm at ostomy site right iliac fossa (8-mm port will go through 12-mm port to be robotic arm no. 1); 5-mm right upper quadrant (this is for the assistant); 8-mm left iliac fossa (robotic arm no. 3); 8-mm left upper quadrant at mid-clavicular line (robotic arm no. 2) (Figs. 22.1 and 22.2).
2. Patient rotated to the right and placed in the Trendelenburg position.
3. Greater omentum reflected over the transverse colon and the small bowel moved to right upper quadrant laparoscopically.
4. Robotically, the inferior mesenteric artery (IMA) pedicle identified and dissected. Left ureter identified and IMA divided with high ligation, proximal to the left colic artery.
5. Medial-to-lateral mobilization of the left colon and division of the inferior mesenteric vein close to the tail of pancreas.
6. Lateral paracolic mobilization of the left colon toward the splenic flexure.
7. Splenic flexure mobilization.
8. Rectal mobilization in the presacral space.
9. Division of peritoneal attachments on the right and left sides of the rectum, and anterior mobilization beginning at peritoneal reflection.
10. Rectum mobilized to anal canal at pelvic floor and divided, after ensuring adequate distal margin.
11. Specimen extracted through keyhole incision at ileostomy site, using a wound protector, for extracorporeal resection and stapled coloanal anastomosis.
12. Formation of right iliac fossa trephine loop ileostomy.
13. Closure of ports >8 mm in size.
ADDITIONAL ADVICE
1. The right-sided ports are placed closer to the midline than in a standard sigmoid colectomy, facilitating access to, and dissection in, the lower pelvis.
2. If it is difficult to find the presacral space on the right side, consider going to a lateral mobilization of the sigmoid before risking nerve or other injury.
3. Making a long incision in the peritoneum to mobilize a long segment of IMA facilitates safe identification of the presacral space and protection of nerves and the ureter.
4. It is often easier to enter the presacral space just inferior to the sacral promontory, and then work back toward the origin of the IMA.
5. Once the IMA and vein are divided, mobilize as much of the descending mesocolon as possible from the medial approach, to facilitate later lateral dissection.
6. When performing the lateral mobilization of the sigmoid colon, draw the colon medially and anteriorly to display the space behind the sigmoid and its mesentery, which has already been dissected with the medial dissection.
7. If it appears necessary to dissect up to the splenic flexure, mobilize the flexure as much as possible (since the patient is in the Trendelenburg position and cannot be repositioned while the robot is docked) and any mesentery necessary at this stage, to avoid potentially compromising blood flow after exteriorizing the specimen, as it is difficult to assess blood flow.
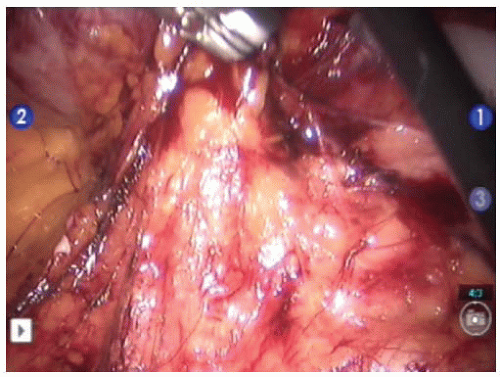
8. Commence the mesorectal dissection posteriorly, using firm anterior and superior retraction of the rectosigmoid to place the loose areolar tissue under tension and facilitate dissection.
9. Firmly pulling the mesentery superiorly, as well as medially away from the lateral pelvic sidewall, facilitates the lateral dissection.
10. The anterior dissection is commenced 1 or 2 mm anterior to the apex of the pouch of Douglas. This enters the correct anatomical plane, keeping the anterior mesorectal fascia intact.
11. Dissection is completed within the anal canal, after seeing the levators curve down into the anal canal, and after confirming an adequate distal margin by digital rectal examination, or endoscopy.
12. Division at the anorectal junction can often be completed using one 45-mm stapler cartridge; however, a second cartridge may be required to divide a final 5 to 10 mm of the rectum. It is important to apply the second cartridge precisely such that the completed distal staple line looks like a single transverse staple line.
13. After resecting the specimen and placing the anvil for anastomosis, the proximal bowel is returned to the abdomen and the ostomy site is temporarily closed with the wound protector to facilitate laparoscopy and anastomosis.
14. If there is not enough reach and the splenic flexure was not fully mobilized, the flexure can now be fully mobilized laparoscopically with the patient placed in the reverse Trendelenburg position or the robot can be redocked.
PATIENT POSITIONING
The patient is placed supine on the operating table on a bean bag. After induction of general anesthesia and insertion of an orogastric tube and Foley catheter, the patient’s legs are placed in yellow fin stirrups. The arms are tucked at the patient’s side and the bean bag is aspirated. The abdomen is prepared with antiseptic solution and draped routinely.
INSTRUMENT POSITIONING
The primary monitor is placed on the left side of the patient at approximately the level of the head. The secondary monitor is placed on the right side of the patient at the same level and is primarily for the assistant during the early phase of the operation
and port insertion. The operating nurse’s instrument table is placed to the right of the patient’s legs. There should be sufficient space to allow the operator to move from either side of the patient to between the patient’s legs if necessary. The assisting operating surgeon stands on the right side of the patient. A 30-degree camera lens is used.
and port insertion. The operating nurse’s instrument table is placed to the right of the patient’s legs. There should be sufficient space to allow the operator to move from either side of the patient to between the patient’s legs if necessary. The assisting operating surgeon stands on the right side of the patient. A 30-degree camera lens is used.
UMBILICAL PORT INSERTION
A veress needle is placed at the base of the umbilicus. Once two “clicks” are felt, sterile saline is injected into the veress needle. If saline flows easily, and air is aspirated easily, the peritoneum is insufflated carefully under low flow. If the opening pressure is lower than 5 mmHg, then the patient is insufflated under high flow.
LAPAROSCOPY AND INSERTION OF REMAINING PORTS
The laparoscopic camera is inserted into the abdomen and an initial laparoscopy is performed carefully evaluating the liver, small bowel, and peritoneal surfaces. A 12-mm port is inserted in the right lower quadrant approximately 6 cm medial and superior to the anterior superior iliac spine. A 5-mm port is then inserted in the right upper quadrant at least a hand’s breadth superior to the lower quadrant port. A 8-mm
left lower quadrant port is inserted. A 8-mm left upper quadrant port is placed in the mid-clavicular line slightly higher than the camera port. The left-sided ports are kept lateral to the epigastric vessels. All ports must be at least 8 cm away from each other to avoid external collisions (see Fig. 22.2).
left lower quadrant port is inserted. A 8-mm left upper quadrant port is placed in the mid-clavicular line slightly higher than the camera port. The left-sided ports are kept lateral to the epigastric vessels. All ports must be at least 8 cm away from each other to avoid external collisions (see Fig. 22.2).
DEFINITIVE ROBOTIC SETUP
The assistant now moves to the patient’s right side, standing cephalad to the surgeon. The patient is rotated with the left side up and right side down, to approximately 15 to 20 degrees tilt, and often as far as the table can go. This helps to move the small bowel over to the right side of the abdomen. The patient is then placed in the Trendelenburg position. This again helps gravitational migration of the small bowel away from the operative field. Laparoscopically, the surgeon then inserts two atraumatic bowel clamps through the two right-sided abdominal ports. The greater omentum is reflected over the transverse colon so that it comes to lie on the stomach. If there is no space in the upper part of the abdomen one must confirm that the orogastric tube is adequately decompressing the stomach of gas. The small bowel is moved to the patient’s right side allowing visualization of the medial aspect of the rectosigmoid mesentery, and also placed up under the transverse mesocolon to give room to see the inferior mesenteric vessels. This may necessitate the use of the assistant’s 5-mm atraumatic bowel clamp through the left lower quadrant in order to tent the sigmoid mesentery cephalad. Any adhesions to the anterior abdominal wall, or adhesions to the pelvis, are laparoscopically lysed at this point.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree