(1)
Division of Colon and Rectal Surgery, George Washington University Hospital, Washington, DC, USA
(2)
Department of Surgery, George Washington University Hospital, Washington, DC, USA
Electronic supplementary material
Supplementary material is available in the online version of this chapter at 10.1007/978-1-4899-7531-7_10. Videos can also be accessed at http://www.springerimages.com/videos/978-1-4899-7530-0.
Keywords
Right HemicolectomyIleocecectomySingle port robotic approachColorectal surgeryIntroduction
Single-incision robotic surgery is utilized in many procedures including but not limited to colectomies, prostatectomies, cholecystectomies, and hysterectomies. The greatest advantage of single-incision robotic surgery compared to laparoscopic is ergonomic superiority and return of triangulation via the cross-arm technique on the da Vinci robot, enhanced three-dimensional acuity, camera stability, and better assistant positioning. Disadvantages such as increased operative and docking time and cost of robot utilization may be offset by more experience and decreased length of stay, respectively. Further studies with larger sample size and cost-benefit analysis will help guide the future of robotic surgery.
Background
Dr. Philip Turner first documented a case of double inguinal hernia in which both sacs were removed through a single transverse suprapubic incision over 90 years ago. Since then there continues to be advancements in the spectrum of single-site techniques [1]. Single-incision surgery has been performed and documented in nearly all surgical domains, including but not limited to colectomies, cholecystectomies, adrenalectomies, splenectomies, appendectomies, lobectomies, herniorrhaphies, hepatectomies, hysterectomies, and oophorectomies. To date, there have been over 1,100 citations in the literature regarding single-incision laparoscopic surgery alone – with single-incision cholecystectomy and single-incision colectomy as the most cited (>250 and >115 citations, respectively) [2].
Prior to trocar placement – whether single or multiport – vascular injury, bowel injury, and incisional hernia must be considered. In general, laparoscopic surgery complications occur in 0.1–10 % of procedures. Nearly 50 % of trocar-related injuries to bowel and vessels occur in the initial entry and are not diagnosed at the time of injury in 30–50 % and 15–50 %, respectively. Literature suggests that the most common complications are bowel and vascular injuries while incisional hernias are rare, with a reported incidence of <1 % [3]. Most reports of incisional hernias have been made with port sites >10 mm; however, hernias with 5 mm trocar placement, although rare, have been noted by several authors [4–10]. Thus, 5 mm ports are not truly “free” and single-port/incision surgery may reduce some of these trocar complications.
Single-incision laparoscopy has several advantages to its multi-incision counterpart as a result of reduced intraperitoneal access via a single laparoscopic port. In addition to fewer incisions and cosmetic benefits, advantages include minimal abdominal wall trauma, decreased postoperative pain and incisional hernia formation, reduction in morbidity, and potentially less narcotic use contributing to shorter duration of postoperative ileus and decreased length of hospital stay [11–14].
Comparisons between single-incision and conventional laparoscopic procedures have been extensively reviewed, with reports of the first laparoscopic colectomy case dating back to 1991 [11]. In one case-controlled study of segmental colectomies, it was found that operative times were longer for single-incision versus multi-incision laparoscopic colectomy (134 vs 104 min, P = 0.0002), while morbidity and length of hospital stay remained similar. In addition, 4 of 29 cases were converted to multiport while 1 of 29 cases was converted to open. The study concluded that while single-incision laparoscopic colectomies are feasible and safe, procedures tend to take longer [15]. A similar study case matched for age, gender, BMI, ASA score, previous abdominal surgery, and splenic flexure mobilization concluded that operative time, conversions, estimated blood loss, and readmission rates were the same when comparing single-incision versus multiport laparoscopic sigmoid colectomies. The authors also noted that length of stay (3.7 vs 5.0 days, p < 0.05) and visual analog pain score on postoperative days 1 and 2 for single-incision procedures were significantly less [16]. Another study by Wolthuis et al. comparing single-port colectomies to the conventional laparoscopic approach reports similar median operative times, estimated blood loss, pain scores, analgesic requirements, inflammatory response, and length of hospital stay [17]. Nonetheless, review of the literature suggests that single-incision laparoscopic colectomies can be performed safely and successfully [18, 19]. Additional studies validate single-incision hemicolectomy as an oncologically feasible and safe procedure with suitable mesocolic excision [20, 21].
In an early multi-institutional study with single-incision laparoscopic colectomies, it was found that surgeons felt the following areas to be more difficult with single-incision laparoscopic surgery: exposure to clinical structures, ease of instrumentation, ease of camera operation, flexure mobilization, surgical ergonomics, and instrumentation conflict. The study also exhibited a 12.8 % conversion rate and associated 7.7 % complication rate in 39 single-incision laparoscopic colectomies performed [22].
While single-incision laparoscopy offers numerous advantages, the procedure also presents several disadvantages. Single-incision laparoscopy, in itself, is technically challenging: instruments crossing, poor positioning with assistant, poor ergonomics, camera instability, and two-dimensional view. The visual axis is often altered as it becomes more axial. There have also been varying reports of length of operative time in the literature with the majority suggesting an increase. Length of hospital stay also varies with literature review though consensus tends to be decreased length. Could robotic surgery offset these technical challenges?
With the advent of robotic surgery, multiple arms may be operated remotely from a stable three-dimensional video-assisted visualization console, which may notably minimize many of the aforementioned disadvantages. The greatest advantage of robotic procedures may be the elimination of instrument conflict with ergonomic superiority. The da Vinci system utilizes a cross-arm technique in which the system’s right and left controls are reversed and the extracorporeal robotic arms are crossed. With this method, the surgeon is no longer required to mentally reverse the function of his/her right and left hands [23]. The robot’s wristed instruments enable emulation of wrist action leading to greater range of motion and ability to operate in tighter spaces in a single-port setting. The robot’s additional degrees of articulation and cross-arm technique also deliver a triangulated field for dissection. This technique takes the conundrum of assistant positioning out of the equation as the assistant is situated between the arms of the robot and becomes an integral component to the procedure itself.
Currently, single-incision robotic surgeries include but are not limited to colectomies, prostatectomies, cholecystectomies, and hysterectomies [24]. One of the first reports of robotic-assisted single-incision right colectomy included three patients utilizing a 4 cm incision with three ports (12 mm, 8 mm, 8 mm) in a medial to lateral approach with extracorporeal resection and anastomosis. It was found that operative time was 152 min with a 33 % conversion rate due to air leak [24]. Lim et al., on the other hand, reviewed 22 cases of robotic single-incision anterior resection for sigmoid colon cancer and reported that it is a safe and viable option for patients. Lim et al. continued to state an estimated blood loss of 24.5 mL mean operating time of 167.5 min, median skin incision size of 4.7 cm, and mean lymph node harvest of 16.8 [25].
In a similar robotic single-port experience at George Washington University (GWU), 11 patients with unresectable polyps and colon cancer requiring right hemicolectomies were observed. Initial results indicated no conversions to open, three conversions to laparoscopy, and three cases of postoperative complications (ileus, wound infection, and anastomotic bleed). In contrast, a similar population of ten patients who underwent laparoscopic right hemicolectomy and ileocectomy resulted in one conversion to open due to adhesions and one postoperative complication (postoperative bleed). In comparing robotic versus laparoscopic procedures, it was found that there were no differences in operative time, estimated blood loss, length of hospital stay, lymph node harvest, and complications; however, there was one conversion from laparoscopic to open with the conventional laparoscopic method.
Nonetheless, robotic single-port surgery does have its disadvantages. While increased operative and docking time may be unattractive to some, with greater surgeon and ancillary team experience, both operative and docking time seem to be comparable to that of non-robotic single-port surgery. Loss of tactile sensation through the robotic arms may be compensated for as the surgeon gains experience with the controls and may be negated by the enhanced three-dimensional visual acuity and camera stability of the robot. Cost of robot utilization must be considered prior to robotic approach initiation and may be offset with procedures that may be more difficult and/or require longer operation time. Decreased length of hospital stay may, in fact, offset the cost of robot utilization and ultimately benefit the patient. Further studies with larger sample size and cost-benefit analysis will help guide the future of robotic surgery and provide more insight into the technicalities of the procedures performed.
Room Setup and Positioning
The patient is placed in the supine position on the operating table on a beanbag. Following induction of general anesthesia and insertion of an oral gastric tube and Foley catheter, both legs are placed in yellow fin stirrups. Both arms are then tucked at the patient’s side and then the beanbag is aspirated. If obese patients will not fit on the OR table, the left arm is left out from the side. The abdomen is then prepared with antiseptic solution and draped routinely.
The primary monitor is placed on the right side of the patient at the level of the shoulder. The secondary monitor is placed on the left side of the patient at the same level, which is primarily for the assistant or observers. The assistant is on the left side of the patient. The operating nurse’s instrument table is placed to the right of the patient’s legs. A 30° upward facing camera lens is preferred.
Port Placement and Extraction Sites
The single-port device is typically placed in the midline and periumbilical location, which also serves as the extraction site. Only two robotic arms are used in addition to the camera port. The robotic arms #1 and #2 are crossed at the fascia and a 30° up scope goes below the two arms (Fig. 10.1). A 5 mm assistant port can be used through the GelPOINT. The robotic arms are then switched on the console manually so the surgeon controls what he or she views as the correct instrument internally.
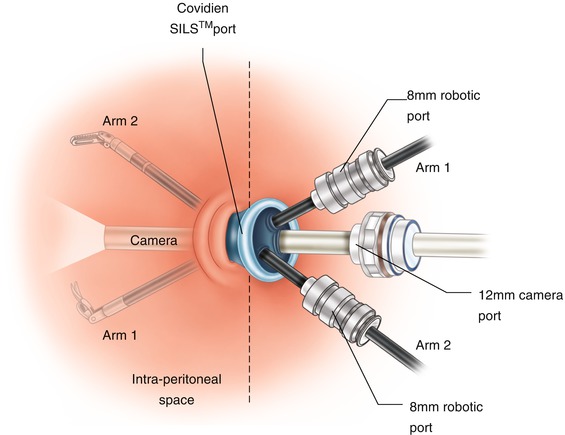
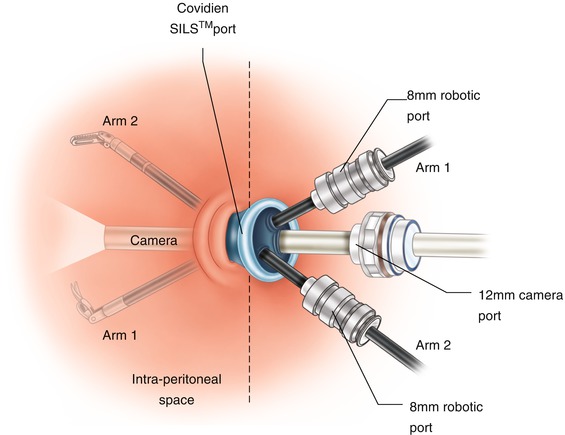
Fig. 10.1
Robotic arm crossing
Operative Steps (Table 10.1)
Table 10.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Single-port insertion and exploratory laparoscopy | 1 |
2. Single-port docking | 3 |
3. Identification and ligation of the ileocolic vessels | 4 (medial to lateral) |
4. Dissection of retroperitoneal plane and identification of the duodenum | 4 (medial to lateral)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





