Fig. 8.1
Port configuration. C 5 mm or 12 mm camera port, L1 5 mm working port, L2 5 mm working port, 12 mm (for stapler) using side-to-side isoperistaltic anastomosis, L3 12 mm working port for stapler using side-to-side retroperistaltic anastomosis
The intracorporeal anastomosis allows the extraction site not only to be typically smaller than needed for an extracorporeal technique, it also allows the extraction site to be off the midline or through a Pfannenstiel incision, which both have a decreased incidence of an incisional hernia compared to a midline incision.
Operative Steps (Table 8.1)
Table 8.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Exploratory laparoscopy | 1 |
2. Identification of duodenum and ligation of the ileocolic vessels | 3 (medial to lateral) |
4 (lateral to medial) | |
3. Mobilization of the right colon and terminal ileum | 4 (medial to lateral) |
2 (lateral to medial) | |
4. Mobilization of the proximal transverse and hepatic flexure | 4 |
6 (with vessels) | |
5. Intestinal division and specimen bagging | 5 |
6. Intracorporeal anastomosis | 6 |
7. Anastomotic leak testing with colonoscope | 3 |
8. Specimen extraction | 2 (transabdominal) |
5 (transvaginal) |
Exploratory Laparoscopy
Pneumoperitoneum is established by use of the Veress needle or Hasson technique and the abdomen is insufflated with carbon dioxide gas to a pressure of 15 mmHg. In most cases the Veress needle is placed in the left mid flank; however, an alternate site, such as upper midline, left upper quadrant, is often selected in patients who have had prior abdominal surgery. Following adequate insufflation and trocar placement, the abdomen is thoroughly inspected for signs of metastatic diseases or other disease processes, which may alter the anticipated procedure. Adhesions to the anterior abdominal wall are taken down carefully in a stepwise fashion and the remainders of the working ports are placed under direct visualization. Once all trocars are placed and the diseased segment is identified, a careful “no-touch” technique for handling the colon and the tumor is rigidly enforced.
Identification of Duodenum and Ligation of the Ileocolic Vessels
Most surgeons are very familiar with the anatomy involved with virtually every type of colon resection performed. Laparoscopy offers a different view with which laparoscopic surgeons must recognize. Laparoscopy provides a better, magnified view of surgery, but it is sometimes difficult to identify the origin of the vascular supply intended in the resection with this procedure. In right-sided colon cancer, there are three major vessels, the ileocolic, right colic artery, and superior mesenteric artery, with wide range of variations of vascular architecture. A laparoscopic lymphadenectomy intracorporeally performed may therefore be more difficult for right-sided colon cancer than for left-sided tumors. The duodenum should be clearly identified as the colon is reflected inferiorly of through the mesenteric window of the hepatic flexure early in the dissection (see Fig. 8.2). While some authors prefer division of ileocolic vessels prior to identification of the duodenum, identification of the latter structure can be the first step of a right hemicolectomy. The ileocolic artery can be divided with staples, ligation, clips, or a coagulator device such as the harmonic scalpel or the LigaSure device. It is helpful to retract the mesentery of the ileocecal complex anteriorly, opposite the root of the mesentery, which will tent up, and the ileocolic vessels should be reactively mobile (see Fig. 8.3). During a lateral to medial approach, the duodenum is identified behind the colon, and a window is created in the mesentery. At this point, this mesentery thickness should be one layer and can be expanded inferiorly to identify the colic vessels, immediately caudal to this opening. Care should be taken to ensure the integrity of the superior mesenteric artery and blood supply to the small bowel.
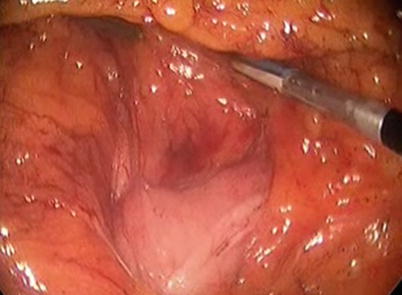
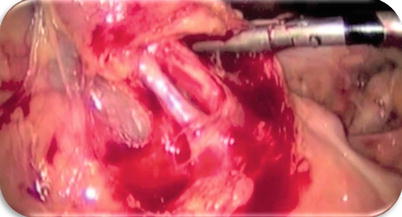
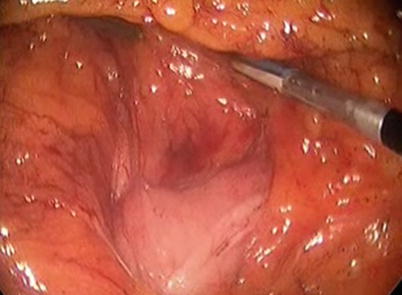
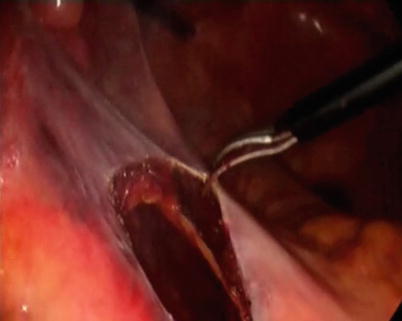
Fig. 8.2
Identification of the duodenum
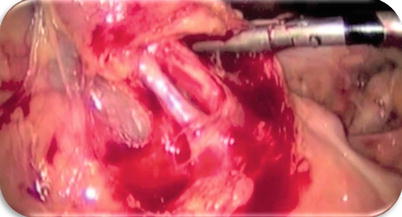
Fig. 8.3
Identification of the ileocolic vessels
Mobilization of the Right Colon and Terminal Ileum
The cecum and the ascending colon, along with lateral attachments, are the most easily exposed segments of the colon during the laparoscopic approach and allows for a very easy mobilization of the right colon once the anatomic relationships of the right mesolocon has been established. It is very important during the mobilization to use gravity to an advantage rather than a disadvantage. Use of the Trendelenburg position, and reverse Trendelenburg and especially right tilt, can allow visualization and mobilization of almost any right colon with much less effort than with nonuse of gravity. It is recommended to push the colon and other organs out of the way rather than pull, as pulling, particularly with torque, tends to injure the colon and other organs. The surgeons should methodically avoid grasping the bowel that is not to be resected and very carefully avoid grasping the tumor in cancer cases. Blunt dissection is always better than sharp dissection unless one can actually see through the tissue being dissected. If inadequate visualization does not allow for clean dissection, change the scope or the position of the scope until the anatomy can be clearly delineated. Often it is helpful to dissect in another angle until anatomy becomes clear.
Two options are available for right colon dissection, lateral-to-medial and medial-to-lateral approach. The medial-to-lateral approach follows the continuous dissection of the retroperitoneum off the colon mesentery from medially. In the case of lateral-to-medial dissection, the terminal ileum and cecum are the first mobilized, followed by the ascending colon through the line of Toldt. The mobilization is done with upward traction of the colon with a nontraumatic instrument and sharp dissection is used for mobilizing the abdominal wall attachments (see Fig. 8.4). Progressive dissection to the terminal ileum may be carried out utilizing sharp dissection with scissors and controlling bleeding or with the use of the abovementioned coagulation devices.