Fig. 5.1
Port configuration. C 5 or 12 mm camera port. L1 5 mm or 12 mm (for stapler) working port right hand. L2 5 mm working port for left hand. L3 5 mm assistant port (not utilized for three-port technique). L4 5 mm port as alternative to L2
Box 5.2. Tip
Visualize the epigastric vessels and place the LLQ port laterally. It should be moved medially to the vessels for morbidly obese patients.
Box 5.3. Tip
The 4-port technique allows optimal exposure, but a 3-port technique is using the L1 and L2 trocars for the surgeon only without an assistant port.
A less invasive technique preferred by one of the authors utilizes an LLQ port L1, an LUQ port L2, and an upper midline (UM) port L4 only (all 5 mm). Extraction and anastomosis can then be accomplished through a far lateral right-sided incision (outside the rectus sheath) for an extracorporeal anastomosis. An off-midline, muscle-splitting incision carries the advantage of a reduced incidence of extraction site hernia. In addition, the extraction and anastomosis may be carried out with less colonic mobilization. An alternative site for extraction is a low transverse Pfannenstiel incision, which also carries a low risk of hernia formation and an improved cosmetic result. However, this approach often requires an intracorporeal anastomosis. Intracorporeal anastomosis can be accomplished by placing a 12 mm port at an LM location to divide the colon and ileum and to perform a stapled anastomosis, which is then incorporated into the incision for extraction after completion.
Operative Steps (Table 5.1)
Table 5.1
Operative steps and degree of technical difficulty
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Exploratory laparoscopy | 1 |
2. Identification and ligation of the ileocolic vessels | 3 (medial to lateral) |
4 (lateral to medial) | |
3. Dissection of retroperitoneal plane and identification of the duodenum | 3 (medial to lateral) |
4 (lateral to medial) | |
4. Mobilization of the right colon and terminal ileum | 2 |
5. Mobilization of the proximal transverse colon and hepatic flexure | 4 |
6. Identification and ligation of the middle colic vessels | 6 |
7. Extracorporeal anastomosis, closure, and (alternative) reinspection | 2 |
Intracorporeal anastomosis | 6 |
Exploratory Laparoscopy
The primary surgeon and assistant both stand on the patients left side: the surgeon toward the feet and the assistant toward the head. The liver and peritoneal cavity are examined for evidence of metastatic disease, a step often facilitated by moderate reverse Trendelenburg position (Box 5.4). The bed is then tilted in a left-side down position, and the small bowel is swept to the left side of the abdomen. The ileum should lie in the pelvis. The greater omentum is lifted over the transverse colon. Some Trendelenburg position may now be necessary to keep the transverse colon out of the operative field. It has been said that “surgery of the right colon is surgery of the duodenum,” and the importance of this statement cannot be overstated. It is at this point in the case that the 2nd portion (descending portion) of the duodenum may already be visible through the right colon mesentery (see Fig. 5.2).
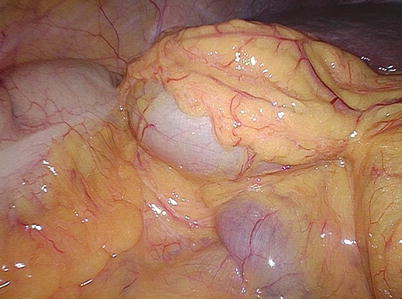
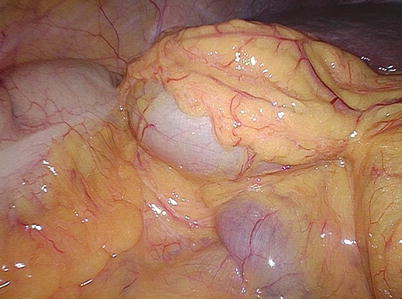
Fig. 5.2
Right colon and duodenum
Box 5.4. Tip
The degree of Trendelenburg versus reversed Trendelenburg positioning depends on the ability to retract the omentum and transverse colon cephalad and the small bowel either cephalad or into the pelvis.
Identification and Ligation of the Ileocolic Vessels
The surgical assistant holds the laparoscope in the left hand and a laparoscopic bowel-grasping instrument in the right hand. The assistant grasps the colonic mesentery medial to the cecum and elevates it toward the right lower quadrant anterior abdominal wall. This will elevate the ileocolic pedicle and allow its identification. The ileocolic artery and vein arise off the superior mesenteric artery and vein. When the assistant properly elevates the right colon mesentery, the ileocolic pedicle can be easily visualized running in a straight line toward the cecum (see Figs. 5.3 and 5.4 and Box 5.5).
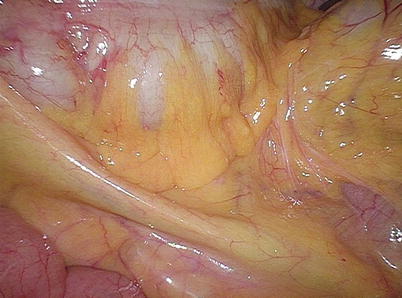
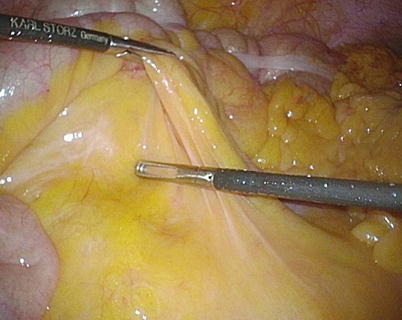
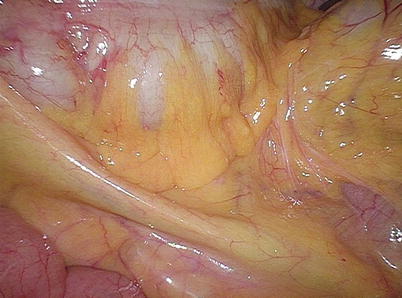
Fig. 5.3
Ileocolic pedicle under tension with cecum elevated
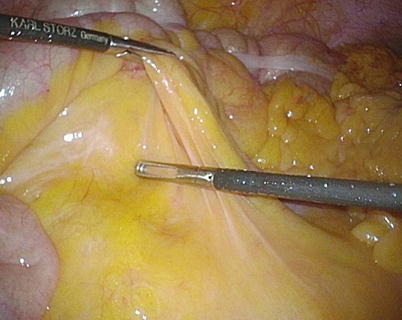
Fig. 5.4
Ileocolic pedicle under tension with mesentery elevated
Box 5.5. Caveat
Ensure that the ileocolic pedicle is not mistaken for ileal branches of the small bowel mesentery. Alternatively, the “bare area” of the ascending colon mesentery next to the duodenum can be identified and incised first.
Once the ileocolic pedicle is elevated, the peritoneum along its base is sharply incised or scored with hook cautery (see Video 5.1). The surgeon accomplishes this maneuver by using a laparoscopic grasper in the left hand and a laparoscopic scissors or hook cautery in the right hand. Alternatively, with the three-port technique omitting the assistant’s port, the surgeon grasps the cecum or its mesentery to allow traction toward the abdominal wall of the right upper quadrant. The peritoneum can be incised sharply with scissors, and no cautery is necessary if the peritoneum alone is opened. Monopolar hook cautery can also be used to the same effect. The use of bipolar cautery in this area tends to fuse the tissues together rather than allow them to open for the dissection (Box 5.6).
Box 5.6. Tip
Incise the peritoneum proximal enough within the mesentery to avoid injuring the ileal branch of the ileocolic pedicle and use blunt dissection parallel to the pedicle to avoid bleeding.
Just cephalad to the ileocolic pedicle, the mesenteric window is obvious and can be opened sharply. The peritoneum anterior to the ileocolic vessels is opened. It is generally not necessary to individually isolate the ileocolic artery and vein prior to vascular ligation, but the pedicle should be widely dissected and care should be taken to clearly identify the duodenum prior to ligation (see Fig. 5.5). In case of a lateral to medial approach, this is typically already accomplished.


Fig. 5.5
Ileocolic pedicle prior to transection with windows created and duodenum dissected off
Box 5.7. Tip
The vessel sealer may be used through whatever port allows a perpendicular seal to avoid bleeding and an endoclip or endoloop should be immediately available for potential bleeding control.
Vascular ligation may be accomplished with a variety of energy devices such as a 5 mm LigaSure, ENSEAL, or THUNDERBEAT (Box 5.7) (see Video 5.1). While the assistant continues to elevate the cecum and transverse colon, the energy device is typically used in the surgeon’s left hand through the LM port L2. Relaxation of the tension before energy application is an essential maneuver to avoid bleeding due to incomplete seal or tissue trauma. A bowel grasper is in the surgeon’s right hand through the RLQ port L1 as a safety tool to quickly occlude the previously dissected ileocolic pedicle base in case of bleeding. With proper attention to tissue tension, this should rarely be necessary. Some surgeons prefer to use clips on the proximal side of the pedicle, which then need to be individually dissected and isolated. Alternatively, the laparoscope can be moved to one of the 5 mm ports, and an Endo GIA may be used to divide the pedicle with a vascular staple load through the central 12 mm camera port or utilizing a 12 mm port for any of the working ports (see Video 5.2).
Dissection of the Retroperitoneal Plane and Identification of the Duodenum
Once the peritoneum is opened at the base of the ileocolic vessels, the retroperitoneal tissue is swept down off of the elevated right colon mesentery in a medial to lateral or inferior to superior approach. The entire 2nd and 3rd portions of the duodenum with the adjacent pancreatic head are exposed and no cautery is used around it (Box 5.8). The retroperitoneal plane is developed further laterally and superiorly. The assistant is generally holding a 30° laparoscope, and the lens may need to be turned to face upward during this dissection (Box 5.9). The assistant is also retracting and tenting up the ascending colon by placing a grasper below the ascending colon and mesentery (see Fig. 5.6). This retroperitoneal plane is extended to the right abdominal sidewall and cephalad beneath the hepatic flexure. The dissection is completed once the lateral peritoneum is reached (see Video 5.3). It is not necessary to dissect and identify the right ureter in routine cases if the correct avascular line of dissection is followed. The same plane is dissected in a lateral to medial approach by rolling over the cecum and ascending colon medially instead similar to a more familiar open approach.
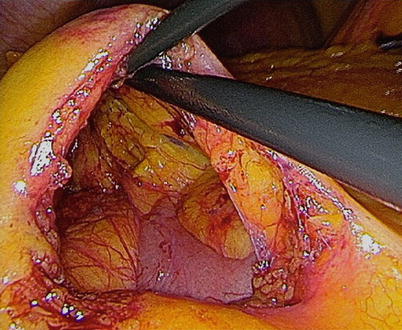
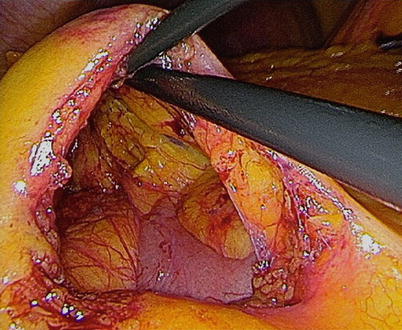
Fig. 5.6
Ascending colon retracted upward and mesentery dissected off retroperitoneum medial approach
Box 5.8. Tip
Look for changes in the fat color to distinguish between retroperitoneal fat and colon mesentery, use blunt dissection in sweeping motions, use the entire dissecting instrument, and use adequate counter traction.
Box 5.9. Caveat
Be very gentle around the duodenum and pancreatic head to avoid bleeding from the trunk of Henle.
Mobilization of the Right Colon and Terminal Ileum
The patient is now placed in a steeper Trendelenburg position, and the ileum that had been resting in the pelvis is elevated to expose the base of the ileal mesentery. In thin patients, the right ureter may be visible through the peritoneum, but does not need to be dissected and visualized if the correct avascular line of dissection is chosen. The assistant will hold the camera and retract the ileum toward the upper abdomen with a laparoscopic grasper. The surgeon uses laparoscopic scissors to sharply incise the peritoneum caudal to the base of the cecum and terminal ileum.
The assistant or surgeon grasps the appendix and cecum and retracts it toward the left upper quadrant. The surgeon divides the lateral attachments of the ascending colon with an energy device (LigaSure, ENSEAL, THUNDERBEAT) or with electrocautery (scissors or hook cautery) in the left hand through the LM port L2. The surgeon’s right hand through the LLQ port L1 retracts the cecum and ascending colon by either grasping and pulling it medially and cephalad or pushing it medially close to the line of dissection (see Videos 5.4 and 5.5). Care is taken to stay anterior to Gerota’s fascia during this mobilization (see Fig. 5.7). An avoidable mistake in laparoscopic right hemicolectomy is to mobilize posterior to Gerota’s fascia toward the liver (Box 5.10). In a medial to lateral approach, the peritoneum is taken down very easily as the plane of dissection is quickly connected to the previous retroperitoneal dissection that was established earlier during the medial approach. To divide the lateral attachments of the distal right colon/hepatic flexure, it may be necessary to place the patient in reverse Trendelenburg position.
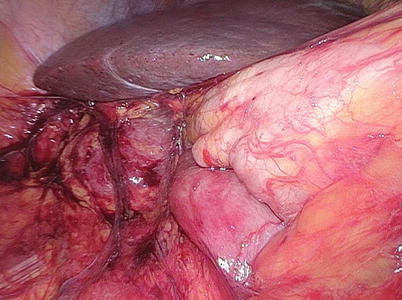
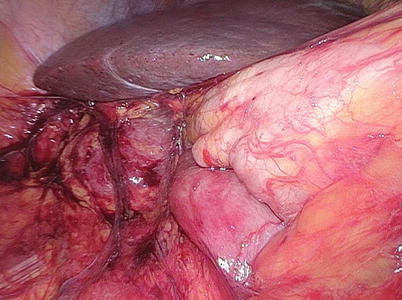
Fig. 5.7
Mobilized colon with visible retroperitoneum and duodenum from lateral approach
Box 5.10. Caveat
Divide the lateral attachments as close as possible to the cecal and ascending colon wall to avoid injury to the ureter/gonadal vessels and to stay in the right plane of dissection
Box 5.11. Tip
Check for adequate mobilization of the ileal mesentery before progressing with the mobilization of the ascending colon.
The mobilization of the terminal ileum is important for an adequate reach of the ileum for an extracorporeal anastomosis (Box 5.11) (see Video 5.5). Occasionally the ileum may be adhered deep in the pelvis, which may necessitate adequate adhesiolysis. This may be facilitated by steep Trendelenburg positioning and placement of small bowel loops out of the pelvis into the upper abdomen. This allows better visualization of the peritoneal line that needs to be incised between the small bowel mesentery and the retroperitoneum.
Mobilization of the Proximal Transverse Colon and Hepatic Flexure
Once the right colon is fully mobilized along the lateral attachments, it is time to mobilize the hepatic flexure. Usually, the surgeon and assistant switch positions at this point with the surgeon now standing to the right of the assistant (both on the patient’s left side) (Box 5.12). The surgeon holds a bipolar cautery device through the LUQ port L3 (LigaSure, ENSEAL, THUNDERBEAT) in the right hand and an atraumatic grasper in the left through the LLQ port L1. The assistant holds the camera in the right hand and an atraumatic grasper through the LM port L2 in the left. The transverse colon is retracted caudally, and the proximal duodenum will be seen inferior to the gallbladder fossa. It may be rarely necessary for the assistant to grasp the gallbladder and elevate it to improve visualization of the hepatic flexure. In morbidly obese patients, an additional trocar may be necessary to retract the liver cephalad. If this additional trocar is needed, it can be placed at the intended extraction site to minimize incisions (see Video 5.6).
Box 5.12. Tip
Depending on the planned distal resection margin, the hepatic flexure and proximal transverse colon can be taken down from a lateral approach by continually rolling over cecum and ascending colon medially and cephalad without the need to enter the lesser sac first from a medial point of dissection.
Occasionally not enough counter traction can be achieved by only pulling the transverse colon caudally (Box 5.13). The surgeon then switches instruments, retracting the omentum or gallbladder and liver cephalad with the right hand and utilizing the left hand for dissection and division of the omentum and hepatocolic ligament while the assistant is pulling the transverse colon or hepatic flexure caudally.
Box 5.13. Tip
Always allow enough traction and countertraction between transverse colon and omentum to enter the lesser sac more easily.
The greater omentum and hepatic flexure are divided with an advanced energy device. It is important to be critically aware of the location of the duodenum, transverse colon, and middle colic vessels during this maneuver. In addition, the ascending colon and transverse colon may be tightly tethered together by omentum. Division of the omental attachments between the ascending colon and transverse colon will help with this and the specimen extraction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








