Fig. 6.1
Port configuration: inferior approach. Hand port: right hand. C: 5 mm camera port. L1: 5 or 12 mm working port right hand. L2: 5 mm optional assistant port
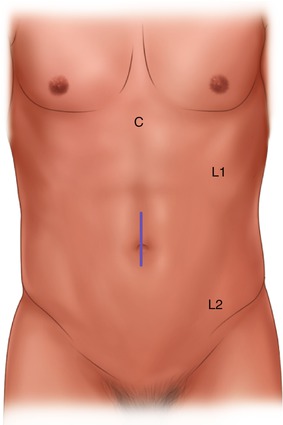
Fig. 6.2
Port configuration: superior approach. Hand port: left hand. C: 5 mm camera port. L1: 5 or 12 mm working port right hand. L2: 5 mm optional assistant port
The assistant will be holding the laparoscope during the procedure. Additional working ports might be inserted once the patient’s anatomy is defined (Box 6.4). Additional ports may be inserted in the lower midline (LM), upper midline (UM), or right upper quadrant (RUQ) to facilitate retraction of the colon or small bowel by the surgeon’s assistant. This additional port is typically 5 mm in size to permit the use of a bowel grasper by the assistant.
Box 6.4. Tip
The retraction using the hand port is superior to a laparoscopic grasper alone. Therefore, no additional working ports and no assistant to retract and coordinate are needed most of the time.
When using a hand-assisted laparoscopic technique, the specimen is extracted through the hand port. The most common site of extraction is therefore a midline periumbilical location. Alternatives include an infraumbilical midline, supraumbilical midline, or transverse umbilical site for the hand port and extraction site. The size of the hand port is based on surgeon glove size, and hand ports come with rulers and instructions for sizing the incision.
A Pfannenstiel or right lower quadrant muscle splitting incisions are typically reserved for a total laparoscopic right hemicolectomy with intracorporeal anastomosis or as part of a total colectomy. The advantages of a muscle splitting technique include reduced postoperative pain, less bleeding from muscle, and a reduction of the risk of hernias.
Operative Steps (Table 6.1)
Table 6.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Exploratory laparoscopy and insertion of the hand port | 1 |
2. Identification and ligation of the ileocolic vessels | 2 |
3. Dissection of retroperitoneal plane and identification of the duodenum | 3 |
4. Mobilization of the right colon and terminal ileum | 2 |
5. Mobilization of the proximal transverse colon and hepatic flexure | 3 |
6. Identification and ligation of the middle colic vessels | 5 |
7. Extracorporeal anastomosis, closure, and reinspection | 2 |
There are common steps that must be included in a safe hand-assisted laparoscopic right hemicolectomy. Depending on the approach used, these steps will be performed in varying sequences and are described below.
Exploratory Laparoscopy and Insertion of Hand Port
Upon initial establishment of pneumoperitoneum and insertion of the laparoscope, general inspection of the abdomen ensues (Box 6.5). Adequate visualization may first require the insertion of additional working ports for retraction. This includes insertion of a hand port in the most appropriate location based on body habitus, location of diseased bowel, and chosen approach. Changes in patient position may also be useful at this time. Exploratory laparoscopy should include the peritoneal surface and omentum for possible tumor seeding. The liver must be evaluated for visible metastases, and placing the patient in reverse Trendelenburg position and using a 30° laparoscope will facilitate its inspection. In a female, the pelvis should be inspected for ovarian metastases. The primary tumor should be identified, either with palpation with a grasper, anatomic landmarks such as the cecum, or perhaps most definitively with localization of ink tattoo on the serosa of the colon.
Box 6.5. Tip
The hand allows for quick adequate positioning of the omentum and small bowel loops. If the patient is very obese or cannot tolerate Trendelenburg positioning, a lap pad placed at the mesenteric root can be useful.
Invasion of local structures such as the abdominal wall, kidney, or duodenum may be appreciated at this stage. In the setting of Crohn’s disease, inspection of the small bowel and colon is performed to assess the extent of disease by running the bowel with an atraumatic grasper and the surgeon’s hand. The cecum, right colon, and terminal ileum must be visualized and assessed for any complicating anatomy, namely, fistulae to small bowel or sigmoid colon, abscess formation, or contained perforation. If there are concerning features present, a trial of dissection may be performed at this time to determine if the right colon and ileum are resectable and whether one can safely proceed laparoscopically. The threshold for conversion to open procedure is different for each surgeon depending on experience with laparoscopic techniques, and consultation with a more experienced colleague may be attained if the anatomy appears challenging during exploratory laparoscopy.
Identification and Ligation of the Ileocolic Vessels
The timing of division of the ileocolic pedicle during the procedure varies depending on which approach is used for laparoscopic right hemicolectomy. Although many divide intracorporeally and as one of the initial steps, extracorporeal division is acceptable, and no data support any improved oncologic outcome using one technique over another as long as a high ligation can be achieved safely through the extraction site to yield adequate number of lymph nodes in the pathologic specimen for malignant disease (Box 6.6). The extracorporeal vessel ligation may be preferentially utilized for patients with friable mesentery in Crohn’s disease.
Box 6.6. Caveat
Evaluate the mesenteric length and abdominal wall thickness. The slightly larger extraction site through the hand port might give enough exposure to perform an adequate extracorporeal high ligation of vessels without the risk of bleeding from traction.
The ileocolic vascular pedicle is a preserved structure in all patients. The pedicle is found in the mesentery of the right colon and can usually be easily identified with proper retraction on the cecum to the right iliac crest (Box 6.7). Using a grasper and the surgeon’s hand, the cecum is retracted anteriorly and slightly inferiorly and the ascending colon anteriorly and superiorly. Left tilt (right side up) of the patient is performed, and the small bowel is brought to the left across the midline. Retraction of the small bowel is typically accomplished with proper positioning. The ileocolic pedicle will be visibly prominent in the mesentery of the right colon and can be grasped with the thumb and index finger of the surgeon’s hand (see Fig. 6.3).


Fig. 6.3
Ileocolic pedicle
Box 6.7. Tip
The ileocolic pedicle can be frequently palpated, encircled, and lifted with the surgeon’s thumb and index finger placed around the pedicle close to the root without the need to create tension first for visual identification.
A window is made in the mesentery along the inferior side of the ileocolic pedicle by first using hook electrocautery or other instruments to score the mesentery and then blunt dissection to create the window, sweeping the mesentery anteriorly and the retroperitoneal structures posteriorly including the duodenum in the medial to lateral approach. This plane is already dissected in all other approaches. Similarly, electrocautery is used to score a short length of the mesentery along the superior border of the pedicle. The superior border of the pedicle is further defined by using blunt dissection. A critical maneuver prior to division of the ileocolic vessels is to identify and separate the duodenum from the ileocolic pedicle. The pedicle can be encircled between the surgeon’s two fingers to confirm its isolation before it is divided (see Videos 6.1 and 6.2).
During the superior approach, the ileocolic pedicle is identified after the right branch of the middle colic is ligated, and the transverse colon, hepatic flexure, and ascending colon are fully mobilized and rotated medially and inferiorly. The pedicle will be then grasped with the left hand from the opposite site of the ileocolic mesentery.
As in the open approach, high ligation of the ileocolic pedicle is performed to ensure adequate lymph node assessment for staging. That is, in the setting of an oncologic indication for right hemicolectomy, the ileocolic vessels are divided away from the bowel and close to their takeoff so that a complete wedge of mesentery is resected along with the colon. For inflammatory bowel disease, this is not a critical step and the vessels may be divided closer to the colon itself. To divide the pedicle, various techniques are used, including clips, laparoscopic staplers, or advanced energy devices. Isolation of artery and vein is necessary in order to place clips, with two or three clips placed on the “staying side” of the ileocolic artery and two on the vein. Isolation of artery and vein is not necessary if using a laparoscopic stapler or bipolar energy device. The surgeon’s hand can be used to safely guide the working instrument into proper position. Inspect for hemostasis after division prior to moving on to step 3.
Dissection of the Retroperitoneal Plane and Duodenum
The duodenum must always be identified during laparoscopic right hemicolectomy (Box 6.8). With the use of electrocautery and advanced energy devices during colon mobilization and division of the mesentery and its vessels, the duodenum is at risk of injury at many stages of the procedure. With the creation of a window in the right colon mesentery during the medial to lateral approach, blunt dissection mainly with a grasper or occasionally the surgeon’s fingers is used to identify and isolate the duodenum along its inferior border at the level of its sweep. Again, by retracting the right colon anteriorly with the surgeon’s right hand in the abdomen, adequate visualization is achieved. Once a window is made in the right colon mesentery, the surgeon’s fingers are placed within the defect to tent up the right colon. A grasper is then used to bluntly sweep down the duodenum and sweep up the superior edge of the mesenteric defect. This should be an avascular plane and the loose areolar tissue should easily separate with blunt dissection. There is no need to grasp the duodenum at all during its identification and isolation (see Video 6.3). Once this is done, the duodenum is used as a landmark during dissection of the hepatic flexure.
Box 6.8. Tip
The hand with the finger’s spread is placed as a wide “retractor” under the ascending colon and mesentery and allows to create excellent counter traction even with more bulky and heavy colon.
For an inferior approach, this can be similarly accomplished by grabbing the cecum and terminal ileum with the right hand and retracting cephalad initially, and once the plane between the ileal mesentery and retroperitoneum is entered, the hand is place under the cecum and ascending colon.
Mobilization of the Right Colon and Terminal Ileum
The patient should be placed in fairly steep left tilt for right colon mobilization. Release of lateral attachments may proceed in either an inferior to superior or superior to inferior direction. The lateral attachments of the right colon are taken down by dividing the attachments along the white line of Toldt, while retracting the colon medially and cephalad with the surgeon’s right hand and utilizing the energy device through the LLQ working port during a medial, lateral, or inferior approach (see Video 6.4). Alternatively, the colon is retracted medially and caudally with the left hand utilizing the LUQ working port. An advanced energy device once again facilitates this dissection, though hook electrocautery should also be adequate in this avascular dissection. The index finger may be used to gently push along the white line to facilitate and expedite the identification of the proper dissection plane (see Video 6.5). The dissection is already accomplished and avoided in a medial or inferior approach, which allow rapid division of the peritoneal attachments only.
As one dissects the right colon, a common pitfall may be encountered (Box 6.9). It is quite easy to enter a dissection plane too lateral, leading to a retrorenal dissection. The dissection must stay anterior to Gerota’s fascia and the right kidney. Using the duodenum as a landmark helps ensure that the surgeon remains in the correct plane. The duodenum should be visualized and protected during division of the lateral attachments once the white line of Toldt is incised.
Box 6.9. Tip
A superior or medial approach avoids a potential wrong line of retrorenal dissection during the lateral approach.
The terminal ileum and appendiceal attachments are also released laterally at this point (see Video 6.6). With proper medial positioning of the terminal ileum, by medially sweeping with the surgeon’s fingers, the right ureter and common right iliac artery can be visualized. These structures must be avoided during mobilization of the terminal ileum.
Mobilization of Proximal Transverse Colon and Hepatic Flexure
The falciform ligament is used as a landmark for the planned distal resection margin (Box 6.10). The middle colic artery is also useful in this regard. The greater omentum is retracted anteriorly/superiorly and divided from the transverse colon using cautery or an advanced energy device (see Fig. 6.4). The use of such a device allows for substantially faster dissection and better coagulation. Clips should routinely not be necessary for dissection of the colon if the surgeon remains in the right plane and uses a bipolar energy coagulation device. The mesentery of the colon is not divided at this stage; rather dissection proceeds above the colon, entering the lesser sac by dividing the gastrocolic ligament and reflecting the gastrocolic omentum.
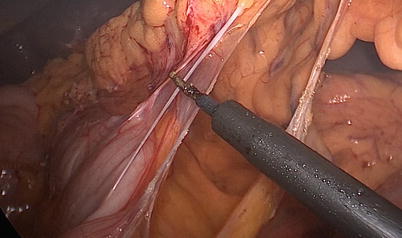
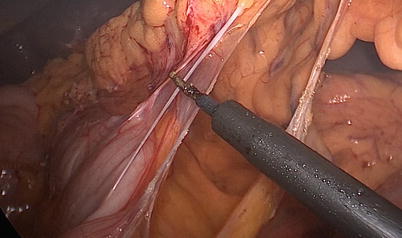
Fig. 6.4
Omentum
Box 6.10. Tip
The LLQ port should be placed medially to the epigastric vessels if the hepatic flexure is mobilized from a lateral approach so the dissecting instrument reaches the hepatocolic ligament.
During the superior approach, the advanced energy device should be used with the surgeon’s right hand through the LUQ port, working in the direction of the hepatic flexure. Mobilization continues around the hepatic flexure, incising the hepatocolic ligament reaching the most superior aspect of the ascending colon. The patient position for this step should be in reverse Trendelenburg. The transverse colon and hepatic flexure are retracted inferiorly during dissection using the left hand. Dissection may be challenging in both thin and obese patients, as the correct plane may not be visible to enter the lesser sac. Gentle blunt dissection with the surgeon’s fingers may facilitate the identification of the right plane. Slow and meticulous dissection is usually adequate to find the correct plane. The transverse colon and hepatic flexure will progressively move into an inferior position as dissection proceeds (see Video 6.7).
The hepatic flexure can also be mobilized just continuing the lateral dissection during latter phases of the medial, lateral, and inferior approach (see Fig. 6.5 and Video 6.4). The ascending colon is retracted medially with the right hand, and the right index finger continually dissects below the hepatocolic ligament entering the lesser sac. The instrument through the LLQ port is reaching over the colon to divide the attachments.
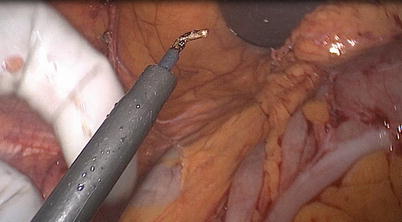
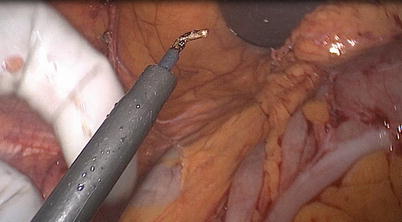
Fig. 6.5
Hepatic attachments
Identification and Ligation of the Middle Colic Vessels
In addition to the division of the ileocolic vessels, the right branch of the middle colic artery may be divided if the patient’s anatomy allows, but is not an essential step in an ileocecectomy. Placing the patient in reverse Trendelenburg position will allow the small bowel to move inferiorly into the pelvis and the transverse colon mesentery to be better visualized. There are two approaches to the transverse mesocolon: inframesocolic and supramesocolic from laterally or medially.
For the inframesocolic approach, the transverse colon is lifted anteriorly and superiorly with the surgeon’s right hand to create tension on the transverse mesentery. The middle colic pedicle is usually visualized and palpated with a grasper at the midpoint of the transverse colon or slightly more proximally. If the mesentery is not filled with excess adipose tissue, the surgeon should visually appreciate a “Y” structure, where the right and left branches take off of the middle colic artery. One should preserve the left colic artery for blood supply of the upcoming ileocolic anastomosis. Electrocautery is used to score the mesentery on either side of the right branch of the middle colic artery, and blunt dissection used to create mesenteric windows. Clips and scissors or an advanced energy device is used to divide the right branch of the middle colic artery.
Occasionally the mesentery is foreshortened, and a supramesocolic approach can be used as an alternative (Box 6.11). The transverse colon is pulled caudally with the right hand toward the pelvis through the LLQ port, and the lesser sac entered with the dissecting instrument by dividing the omentum of the transverse colon. The previous cut end of the mesocolon is identified below the omentum, and the right branch of the middle colic vessels subsequently ligated from lateral. Alternatively, the left hand retracts the transverse colon inferiorly through the LUQ port, and the right branch of the middle colic is divided from medial after entering the lesser sac.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








