First author
No. of patients
Major leaks (%)
<6 cm (%)
Biondo [7]
211
5.7
Docherty [12]
652
4.4
Alves [5]
707
6
Konishi [10]
391
2.8
Hyman [2]
1,223
2.7
Lipska [6]
541
6.5
Branagan [11]
1,834
3.9
Sorenson (1999)
333
15.9
Wong [15]
1,066
3.8
Platell [9]
1,639
2.4
Karanjia [14]
219
11
97
Law [3]
196
10.2
100
Gastinger [16]
2,729
14
100
Rullier [4]
131
19
100
Vignali [8]
284
7.8
100
Intrathoracic anastomotic leakage represents a much more life-threatening event, with high mortality rate. Its incidence is reported to range between 6 and 30 % [17–19].
14.2 Risk Factors
Many risk factors have been demonstrated to be significantly related to anastomotic leak. Patient risk factors include malnutrition, steroids, tobacco and alcohol use, leukocytosis, cardiovascular disease, ASA score, and diverticulitis; intraoperative risk factors include the distance of anastomosis from the anal verge, operative time >2 h, bowel obstruction, blood supply to anastomosis, perioperative blood transfusion, and intraoperative septic conditions; as regards extraperitoneal anastomoses, male gender and obesity are associated to an increased risk of dehiscence [16, 20–22]. Defunctioning loop stoma has been described to reduce the rate of symptomatic anastomotic leakage in low anterior rectal resection [23].
In a large multicenter analysis of oncological and survival outcomes following anastomotic leakage after rectal cancer surgery, oncological outcome was not significantly influenced by anastomotic leakage, even if overall survival was reduced [24].
14.3 Management
Anastomotic leakage management depends on clinical manifestation, on clinical stability of the patient, and on the distance of the anastomosis from the anal verge, particularly if the anastomotic leak is cervical or extraperitoneal, rather than mediastinal or intraperitoneal.
Conventional operative management includes, as regards colorectal anastomosis, explorative laparotomy, peritoneal lavage, and, in at least 80 % of cases, the creation of a derivative stoma. This reduces complications such as peritonitis and sepsis and mortality rate [16], but surgical management leads to a relatively high morbidity rate. Morbidity rate with stoma creation is 30 % and reversal rate in patient with anastomotic leakage is <50 % [25, 26].
As regards intrathoracic dehiscence , surgical management is a highly demolishing surgery with high morbidity and mortality rate.
Technological improvements allowed introduction of new techniques in the management of anastomotic leaks. Endoscopic treatment of anastomotic dehiscence has been proposed as an alternative to operative management in clinically stable patient without generalized peritonitis. In general, patients who present with generalized peritonitis, free intraperitoneal leak or high-grade sepsis with hypotension should be first resuscitated and surgery is mandatory.
Distance of anastomotic dehiscence from anal verge influences subsequent management because of the different probability of free intraperitoneal leak and subsequent generalized peritonitis. Extraperitoneal leaks (e.g., after anterior resection of rectum) often lead to extraperitoneal abscess, such as presacral collections that allow more likely a nonoperative management.
Three main endoscopic options in the management of anastomotic dehiscence are nowadays available:
Synthesis and suturing devices
EndoVac therapy
Covered self-expanding metal stents (SEMS)
14.4 Synthesis and Suturing Devices
Synthesis and suturing devices allow a closure by first intention of the anastomotic defect. Many synthesis and suturing techniques have been described among which clipping is most frequently used. Different clipping devices have been described. Two-pronged endoclips (e.g., Quickclip II, Olympus, Tokyo, Japan, or Resolution Clip, Boston Scientific, MA, USA) with a maximum opening distance of 11 mm are marketed (Fig. 14.1a). TriClip is characterized instead by a third equidistant prong and an opening distance of 12 mm, theoretically owing to the possibility to grasp a larger and a wider amount of tissue (Fig. 14.1b).
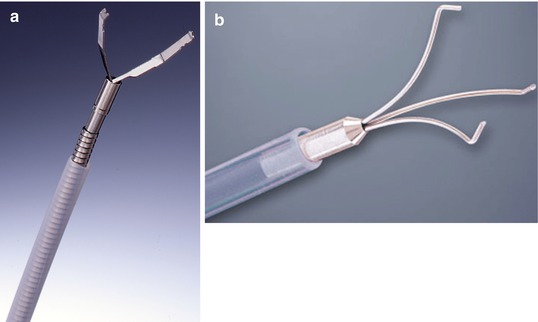
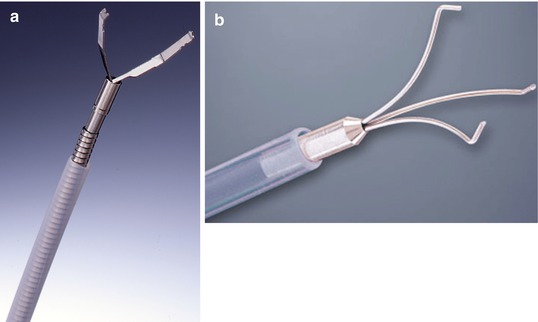
Fig. 14.1
(a) Synthesis and suturing devices, the Resolution clip (Boston Scientific, Natick, MA, USA). (b) Synthesis and suturing devices, the TriClip (Courtesy of Bloomington, IN, USA)
A literature review by Trecca et al. [27] on endoscopic repair of colonic perforation using synthesis devices showed a success rate from 60 to 100 % for nonoperative management of small perforations, in the absence of signs of generalized peritonitis (Table 14.2). This review highlighted the importance of early diagnosis of perforation in order to achieve therapeutic success. Some cases require two or three separate sessions for closure, early diagnosed leaks usually healing within 1 week of clip application, whereas chronic fistulas often require 2- or 3-week-long multiple session treatments.
Table 14.2
Systems ad suturing devices
Author | No. of patients | Cause | Size (mm) | Device | Site | Hospital stay |
|---|---|---|---|---|---|---|
Fujishiro (2006) | 9 | ESD | 3 | Olympus HX-600–090 L | Cecum (2) | 12.1 |
Olympus HX-5QR | Ascending (2) | |||||
Transverse (2) | ||||||
Sigmoid (1) | ||||||
Rectum (2) | ||||||
Barbagallo (2007) | 1 | Polypectomy | 20 | Olympus | Sigmoid | 8 |
Mana (2001) | 1 | Diagnostic | “Small” | Olympus HX-600–135 | Sigmoid | 8 |
Fu (2005) | 1 | EMR | “Small” | N/A | Ascending | 5 |
Taku (2007) | 23 | EMR (12) | N/A | Olympus HX–600–090 L | N/A | 9.1 |
ESD (6) | Olympus HX–5QR | |||||
Hot biopsy (1) | ||||||
Polypectomy (4) | ||||||
Magdeburg (2008) | 27 | EMR (25) | N/A | Boston Scientific Resolution | N/A | 3.5 |
APC (1) | ||||||
Heldwein (2005) | 5 | Polypectomy | N/A | N/A | N/A | N/A |
Yoshikane (1997) | 1 | EMR | 4 | Olympus HX-5QR | N/A | 14 |
Dhalla (2004) | 1 | Polypectomy | 6 | Olympus HX-600–135 | Cecum | 9 |
Kirshniak (2007) | 3 | Polypectomy (2) | 5 | Ovesco OTSC | Splenic flexure | N/A |
Diagnostic (1) | ||||||
Trecca (2007) | 3 | EMR (1) | 26 | TriClip | Descending (1) | 6 |
Diagnostic (2) | Sigmoid (2) |
Many case series report feasibility of endoscopic treatment by using clipping devices in closing anastomotic leakage in esophagogastric surgery [28, 29] and esophago-mediastinal fistula [30, 31]. These two reviews show that endoscopic treatment of small perforations or fistula due to anastomotic leaks with metallic clips can be used safely in selected patients and, alone or in combination with the conservative treatment, may achieve high percentage of leakage closure owing to a reduction of morbidity and mortality if compared with upfront surgical management.
OTSC (over the scope clip ) is a clip of new conception. It consists of a nitinol clip, with a shape similar to a bear trap, attached to an applicator, and applied around a cap mounted on the tip of the endoscope. After placing the tip of the scope in front of a visceral defect, orifice margins are retracted with a grasper into the cap and the clip released (Fig. 14.2). Nitinol is a metal alloy with shape memory, so if it is needed to remove the clip, frozen water irrigation allows OTSC to reduce strength so that it can be easily pulled out using an endoscopic forceps [32].


Fig. 14.2
OTSC system (Courtesy of Ovesco GmbH, Tübingen, Germany)
OTSC is nowadays available in different sizes between 11 and 14 mm in diameter. In all cases this device has a wider diameter compared to other kind of endoclips, and the possibility to retract tissue inside the branches allows to close defect up to 20 mm of diameter and larger.
First clinical series on OTSC were published in 2007 by Kirschniak including also bleeding lesions [33]. In a later report from the same group, eight cases of gastrointestinal fistula and 11 cases of perforation were reported. Primary success rate of 100 % was reported with 26 % of recurrence [34].
Our personal series of OTSC includes 21 cases, of which 17 consist of anastomotic leaks following colorectal surgery. Overall primary success rate was 94.1 % (16/17) with a recurrence rate of 18.8 % (2/16). Surgical intervention with stoma creation was necessary in 2/17 cases (11 %). One of the two recurrences was successfully treated by a second OTSC application (Table 14.3).
Table 14.3
OTSC personal series
Age | Site | Etiology | Time after surgery | Diameter/margins | OTSC mm | Success | Combined treatment | Follow-up | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
1. | 73 | Rectum | Leak colorectal anastomosis | Postradiation | 24 months | 10 | Fibrotic | 12 | Yes | Primary success | |
2. | 58 | Rectum | Leak colorectal anastomosis | Postradiation | 21 months | 8/5 | Fibrotic | 12 | No | Persistent defect | |
3. | 76 | Rectum | Leak colorectal anastomosis | Postradiation | 13 days | 10 | Fibrotic | 12 | Yes | Primary success | |
4. | 41 | Rectum | Leak colorectal anastomosis | Postradiation | 16 months | 6 | Fibrotic | 12 | Yes | Primary success | |
5. | 59 | Rectum | Rectovaginal fistula/anastomotic leak | Postradiation | 25 days | 5 | Fibrotic | 12 | Yes | Primary success | |
6. | 65 | Rectum | Rectovaginal fistula/anastomotic leak | 6 days | 10 | Tender | 12 | Yes | Stoma | Secondary success | |
7. | 73 | Rectum | Leak colorectal anastomosis | Postradiation | 15 days | 10 | Fibrotic | 12 | Yes | Primary success | |
8. | 56 | Rectum | Leak colorectal anastomosis | Postradiation | 20 days | 10 | Fibrotic | 12 | Yes | Primary success | |
9. | 74 | Rectum | Leak colorectal anastomosis | Postradiation | 21 months | 12 | Fibrotic | 12 | Yes | Primary success | |
10. | 66 | Rectum | Leak colorectal anastomosis | Postradiation | 13 days | 8 | Fibrotic | 12 | Yes | Primary success | |
11. | 69 | Rectum | Leak colorectal anastomosis | 25 days | 9 | Fibrotic | 12 | Yes | Primary success | ||
12. | 76 | Rectum | Leak colorectal anastomosis | 16 days | 12 | Fibrotic | 12 | Yes | Primary success | ||
13. | 68 | Colon | Colocutaneus/anastomotic leak | 6 months | 5 | Fibrotic | 12 | Yes | Primary success | ||
14. | 82 | Colon | Colocutaneus/anastomotic leak | 6 months | 2 | Fibrotic | 12 | Yes | Recurrence of defect | ||
15. | 38 | Rectum | Rectovesical fistula | Traumatic | 120 months | 5 | Fibrotic | 14 | Yes | Primary success | |
16. | 63
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| ||||||||||





