Fig. 3.1
The Mattox maneuver of left-sided visceral rotation to expose the proximal abdominal aorta
Alternatively, the aorta may be approached through the lesser sac. The lesser omentum is widely opened and the left lobe of the liver retracted. This provides a window to the gastroesophageal junction. Again, the esophagus is mobilized and the aorta can be clamped (Fig. 3.2).
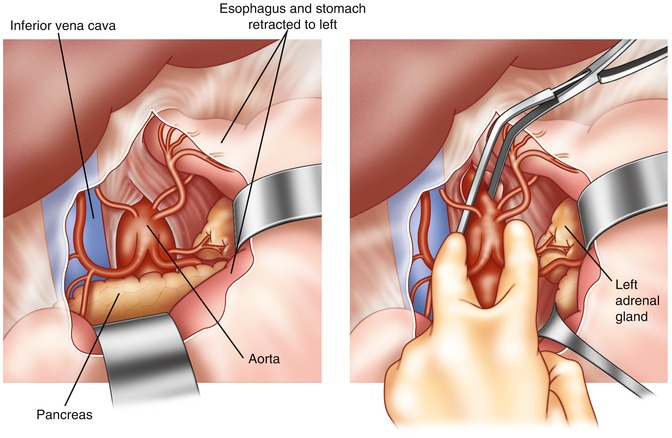
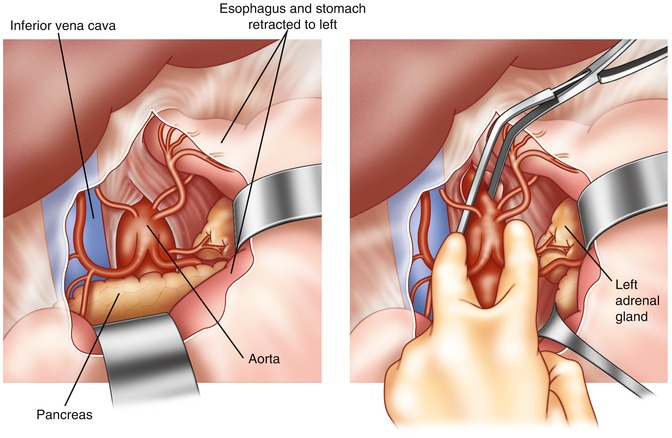
Fig. 3.2
Access to the proximal aortic aorta through the lesser sac
Some have advocated aortic compression be accomplished with compression devices, either a sponge stick or a more formal device known as an aortic compressor (Fig. 3.3). This allows aortic compression and presumed occlusion without requiring any other maneuvers. These devices are applied to the aorta anteriorly, hopefully occluding aortic flow. Unfortunately, these devices often migrate, slipping off the aorta. The task of holding these devices is often left to the junior member of the team, who may not be able to maintain true aortic occlusion.
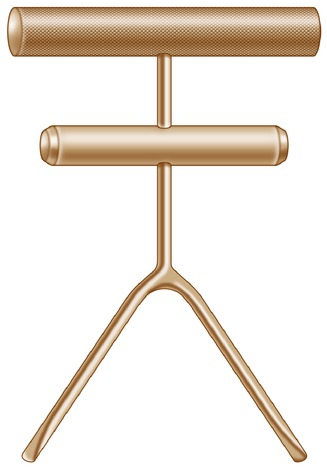
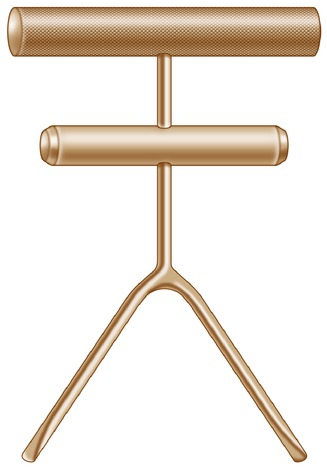
Fig. 3.3
Aortic occlusion clamp
Each of these operative maneuvers has significant disadvantages. They each require time. While philosophically and conceptually simple, either of the operative maneuvers to obtain aortic occlusion takes at least several minutes to accomplish. This is, of course, valuable time that could be spent directly attacking the hepatic hemorrhage. As there is no aortic occlusion achieved until the clamp is applied, the liver simply continues to bleed. In addition, either of the two operative maneuvers requires manipulation of an area close to the liver. If there is a hemostatic clot, which may have formed on the liver during hypotension, it can be misplaced by this manipulation, worsening the hepatic bleeding.
An alternative is to occlude the aorta in the chest [1]. This requires a left anterolateral thoracotomy. The lung is retracted anteriorly and the aorta dissected free just above the diaphragm. Once again, the esophagus must be identified and care taken to positively identify the aorta. A cross clamp is then applied. This has the advantage of being somewhat remote from the liver. Thus, the planes are not obscured by ongoing hepatic hemorrhage. In addition, it would be difficult to worsen the liver bleeding, manipulating the aorta in the chest. This has the downside, however, of requiring the surgeon to open an uninjured body cavity. The thoracotomy itself, when performed rapidly, can be a source of substantial blood loss, as it is usually not possible to obtain meticulous hemostasis of the chest wall musculature. In addition, the open chest serves as a source of heat loss, worsening the possibility of hypothermia.
Resuscitative Endovascular Balloon Occlusion of the Aorta
Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a new technique which can be attractive as an adjunct to hepatic hemorrhage. The REBOA is placed via the common femoral artery. A standard femoral arterial line is placed, an Amplatz wire is placed via the femoral arterial catheter and the catheter removed. A 12 French introducer is then placed over the guidewire and threaded up into the iliac artery (Fig. 3.4). The guidewire is left in place. The balloon occluder is then threaded over the guidewire, through the introducer system, and up into the aorta. In the case of hepatic hemorrhage, the balloon must be positioned in the distal thoracic aorta, in order to provide inflow occlusion. Placement of the balloon can be confirmed via plain X-ray or fluoroscopy, particularly if some contrast has been instilled into the balloon (Fig. 3.5). Clinicians facile enough with the ultrasound probe may be able to identify the balloon ultrasonographically. There are a number of technical tips important for safe placement of the REBOA. It must be placed into the common femoral artery. The 12 French introducer system simply is too large to be inserted via the superficial femoral artery. If it is to be inserted percutaneously, care must be taken to access the common femoral artery. Ultrasound guidance can be helpful in ensuring that the common femoral artery is in fact accessed.










