CHAPTER 9 RESECTION FOR BILIARY CANCER
INTRODUCTION
This chapter addresses the resection of primary malignancy of the intrahepatic and extrahepatic biliary tree. Gallbladder cancer is an important extrahepatic biliary cancer that is often discovered incidentally. Cholangiocarcinoma occurs at the biliary confluence, in the mid-duct, or in the distal duct presenting as a periampullary tumor (see also Chapter 10). Three distinct macroscopic subtypes of cholangiocarcinoma are well described: sclerosing, nodular, and papillary (Weinbren and Mutum, 1983).
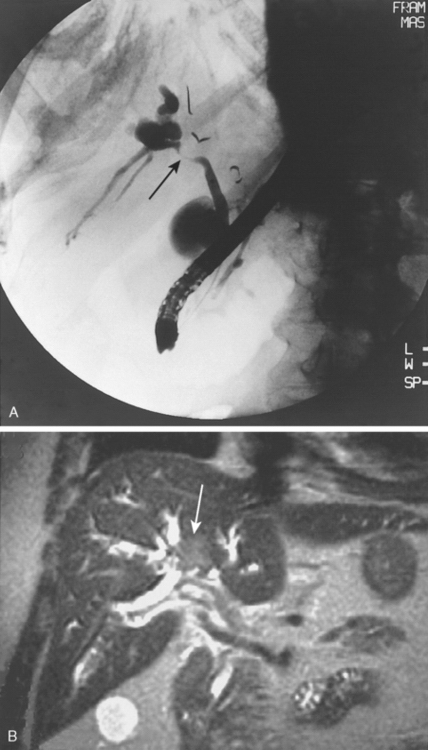
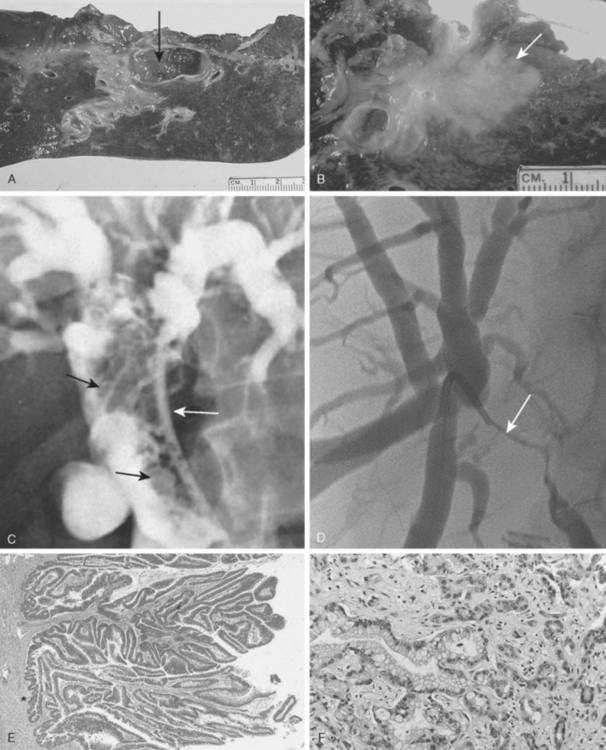
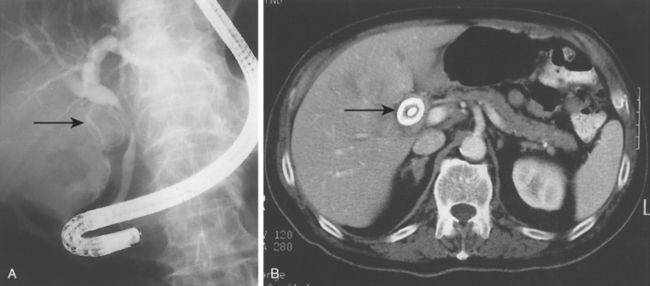
Sclerosing tumors cause an annular thickening of the bile duct, often with diffuse infiltration and fibrosis of the periductal tissues (Figs. 9-1 and 9-2). Nodular tumors are characterized by a firm, irregular nodule of tumor that projects into the lumen of the duct. Longitudinal spread along the duct wall and periductal tissues is an important pathologic feature.
The papillary variant is soft and friable and may be associated with minimal transmural invasion. A polypoid mass that expands rather than contracts the duct (see Fig. 9-2) is a characteristic feature. The bulk of the tumor may be mobile within the bile duct.
Biliary cancer may arise within the intrahepatic biliary tree presenting as a mass or as a biliary cyst. Generally speaking, periampullary cancer is dealt with by pancreaticoduodenectomy (see Chapter 10) and intrahepatic cholangiocarcinoma by hepatic resection (see Chapters 2 to 5). Cholangiocarcinoma involving the proximal bile ducts (hilar cholangiocarcinoma) and gallbladder cancer require biliary resection, with or without a concomitant hepatic resection.
INFECTION
Bacterial contamination of the bile (bactibilia) is common in patients with hilar cholangiocarcinoma (McPherson et al., 1984). Instrumentation and previous operation significantly increase the incidence of bactibilia and the risk of postoperative infection and are associated with greater morbidity and mortality rates after surgical resection.
ATROPHY
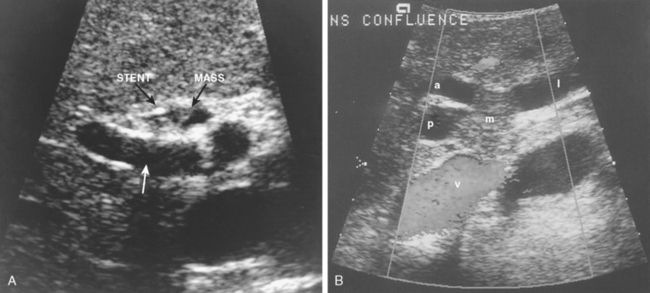
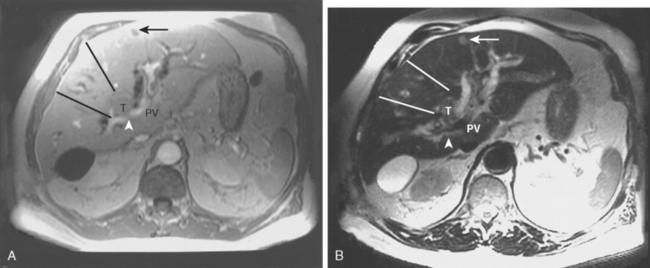
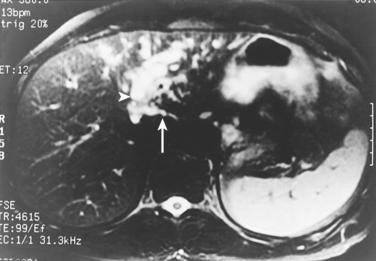
Portal venous inflow and bile flow are important in the maintenance of liver cell size and mass (Hadjis and Blumgart, 1987). Segmental or lobar atrophy may result from portal venous occlusion or biliary obstruction. One or both of these findings are often present in patients with hilar cholangiocarcinoma. Cross-sectional imaging shows a small, often hypoperfused lobe (Figs. 9-3 and 9-4).
CHOLANGIOCARCINOMA INVOLVING THE PROXIMAL BILE DUCTS (HILAR CHOLANGIOCARCINOMA)
CLINICAL PRESENTATION AND IMAGING
Imaging
Alternative Diagnoses
The most common alternative diagnoses are gallbladder carcinoma, Mirizzi syndrome (Fig. 9-8), and idiopathic benign focal stenosis (malignant masquerade) (Hadjis et al., 1985).
Preoperative Evaluation
Assessment includes fitness for surgery (Burke, 1998). Characterization of tumor extent should take into account all available preoperative data related to local tumor, including the extent of tumor within the biliary tree, vascular involvement, lobar atrophy, and metastatic disease. This makes it possible to stage tumors preoperatively in a way that correlates with resectability and outcome. A proposed clinical staging scheme (Table 9-1) underscores the importance of considering portal vein involvement and liver atrophy in relation to the extent of ductal cancer spread. Ipsilateral involvement of vessels and bile ducts is usually amenable to resection, whereas contralateral involvement is not. (Jarnagin et al., 2001, 2005).
TABLE 9-1 Proposed Preoperative T Staging of Hilar Cholangiocarcinoma
| STAGE | CRITERIA |
|---|---|
| T1 | Tumor involving biliary confluence ± unilateral extension to 2 biliary radicles * |
| T2 | Tumor involving biliary confluence ± unilateral extension to 2 biliary radicles and ipsilateral portal vein involvement ± ipsilateral hepatic lobar atrophy |
| T3 |
* Two biliary radicles = secondary biliary radicles.
From Jarnagin WR, et al, 2001: Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 2001;234:507-519.