Renal masses
Anthony Koupparis
Malignant renal masses
Introduction
Renal cell carcinoma (RCC) is the most common renal tumour. It accounts for approximately 3% of adult malignancies, 85% of renal malignancies and 2% of all cancer deaths. In 1999 in the UK, 3676 patients were diagnosed with RCC, with just over 2000 dying from the disease in the year 2000. In the USA, approximately 36 000 new cases occurred in 2005, with 12 500 deaths occurring in the same year. RCC is the most lethal of urological tumours, with approximately 40% of patients dying of the condition. Roughly 25% of patients present with locally invasive or metastatic disease. RCC is most commonly sporadic; however, distinct groups of patients have been identified that develop rarer hereditary forms.
History
RCC has a variety of synonyms. It has been termed hypernephroma, due to the fact it was incorrectly thought to arise from the adrenal gland. Its other names include Grawitz tumour after Paul Albert Grawitz, professor of pathology at Greifswald Germany, clear cell carcinoma and nephrocarcinoma.
In 1826 Konig first described the anatomy of kidney tumours. In 1861 Wolcott reported the first nephrectomy; interestingly, he presumed he was operating on a hepatoma. This was followed by the first ‘planned’ nephrectomy in 1869 by Simon. In 1903 the incorrect term hypernephroma was corrected by Albarran and Imbert, who recognized that these tumours originated from the kidney as opposed to the adrenal glands.
Epidemiology
Overall, RCC affects males twice as commonly as females. There are variations within the histological subtypes; for example, papillary RCC is five times more common in men. In general, RCC usually presents in the fourth to sixth decades of life.
Aetiological risk factors include:
Smoking.
Urban residents.
Low socioeconomic status.
Renal failure and long-term kidney dialysis.
Obesity.
Asbestos exposure.
Hypertension.
Anatomical: polycystic and horseshoe kidney.
Nutritional factors: vitamins A, C and E and fruit and vegetables are protective.
Genetic factors. Several inherited forms of kidney cancer exist: von Hippel-Lindau (VHL); inherited form of clear cell: hereditary papillary renal carcinoma; inherited form of type I papillary RCC: hereditary leiomyoma RCC; inherited form of type II papillary RCC: Birt-Hogg-Dube syndrome (BHD); risk of developing several different types of kidney cancer, including chromophobe RCC and oncocytoma.
Pathology
RCC is an adenocarcinoma of the renal cortex, probably arising from the proximal convoluted tubule. Macroscopically, RCCs are typically round and vary in size. They are generally comprised of areas of yellow or brown tumour interposed with areas of haemorrhage and necrosis. They are often surrounded by a pseudocapsule of compressed tissue. Up to 20% contain calcification, and are multifocal. Approximately 25% are cystic, with 2% of cases associated with synchronous or asynchronous bilateral tumours.
Histological classification
Conventional: comprise 80% of RCCs and arise from the proximal convoluted tubule. Microscopically, they can include clear cell, granular cell or mixed types (7.1).
Papillary: comprise 15% of RCCs and also arise from the proximal convoluted tubule. Two subtypes of papillary RCC exist: type 1 and type 2. Type 2 cancers are genetically more heterogeneous, have a poorer prognosis, and may arise from type 1 cancers.
Chromophobe: comprise 5% of RCCs and probably arise from the distal convoluted tubule.
Collecting duct (Bellini): comprise <1% of RCCs.
Sarcomatoid variant: rare subtype that exhibits an aggressive behaviour and has a poor prognosis.
Medullary cell: very rare; associated with sickle cell trait or disease and arise from the cortical medullary collecting duct.
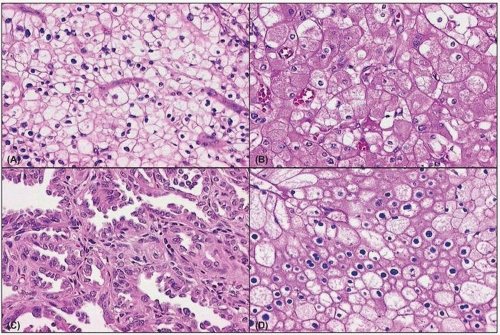 7.1 (A) Histological slide of a conventional clear cell RCC. Note the round or polygonal cells with abundant cytoplasm. (B) Histological slide of a conventional granular cell RCC. The granular cells have eosinophilic cytoplasm and abundant mitochondria. (C) Histological slide of a papillary renal cell RCC. Microscopically, they consist of eosinophilic cells arranged in a tubular or papillary fashion. (D) Histological appearance of a chromophobe RCC. Note the relatively transparent cytoplasm with a fine reticular pattern which has a plant-cell appearance. |
Grading
RCCs are assigned a grading according to Fuhrman’s criteria proposed in his article the Prognostic significance of morphologic parameters in renal cell carcinoma published in 1982 in the American Journal of Surgical Pathology. The nuclear grading system is based on nuclear size and shape, number and size of nucleoli, and clumping of chromatin. These characteristics give an indication of how actively the tumour cells are producing protein, and give an important indication of survival.
1. Well differentiated.
2. Moderately differentiated.
3/4. Poorly differentiated/undifferentiated.
Staging
Genetics
Studies from the early 1980s observed that deletions and translocations of the short arm of chromosome 3 occur in sporadic, non-inherited kidney cancer. Furthermore, loss of a segment of chromosome 3 could be an early event in the development of RCC. This led to an enormous amount of work on hereditary forms of RCC with the hope that observations in these groups of patients might be applicable to RCC as a whole and lead to the development of new treatment strategies for the management of RCC.
von-Hippel Lindau (VHL) syndrome
VHL is a rare autosomal dominant cancer syndrome. Affected individuals develop retinal angiomas, haemangioblastomas of the cerebellum and spine, phaeochromocytomas, renal and pancreatic cysts (7.2) and in approximately 50% of cases bilateral, multifocal clear cell RCCs (7.3). The VHL tumour suppressor gene responsible for this syndrome was identified in 1993. It undergoes a ‘two-hit’ loss of function whereby both copies of the gene present in the tumour tissue have been inactivated by mutation or loss. Interestingly, defects in the VHL gene appear to be responsible for approximately 60% of cases of sporadic clear cell RCC.
|
The VHL protein produced in this condition arises from theVHL gene. It functions as a tumour suppressor by binding to transcriptional activators of hypoxia-inducible genes, such as hypoxia-inducible factor-α (HIF-1α) and 2α (HIF-2α), thereby destabilizing them. In particular, the VHL protein promotes the ubiquitination and destruction of HIF-1α. In clear cell RCC, loss of the VHL gene leads to an increase in HIF-1α, resulting in overexpression of proteins normally seen with hypoxia, for example, vascular endothelial growth factor (VEGF), transforming growth factor-α (TGF-α) and -β (TGF-β), and platelet-derived growth factor-β (PDGF-β




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








