Reoperative urethroplasty is complicated by increased urethral and periurethral scar and the frequent persistence of comorbid conditions that caused the original failure. Nevertheless, by experienced clinicians, reoperative urethral reconstruction can be completed with success rates comparable with those of primary urethroplasty.
Key points
- •
Reoperative urethroplasty may be compromised by poor tissue vascularity.
- •
Excision of poorly vascularized scar is important for successful reconstruction.
Urethroplasty is the gold standard for treatment of anterior urethral strictures. Reported success rates for excisional and primary anastomosis range from 86% to 99%. Success rates for substitution urethroplasty are lower, but remain high at 80% to 90% for oral mucosal grafts, and 75% to 87% for penile skin flaps. For patients with stricture recurrence, reoperative urethroplasty is rendered more challenging by the presence of dense scar tissue and poor tissue vascularity. Further, patients having prior substitution urethroplasty may have a concomitant shortage of donor sites for penile skin flap or oral mucosa graft. For these reasons, our approach to reoperative urethroplasty has centered on an excisional strategy when possible. The role of excisional reoperative urethroplasty is highlighted in this article.




Preoperative evaluation
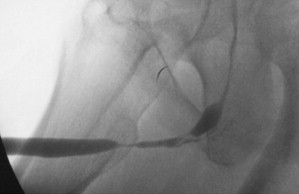
Nearly all patients with stricture recurrence after urethral reconstruction present with recurrent voiding symptoms. At first, imaging studies including retrograde urethrography (RUG) and voiding cystourethrography (VCUG), when possible, are performed because the radiographic appearance of strictures is known to change dramatically over time after intervention. Patients who have previously undergone urethroplasty, especially substitution techniques, often have irregularities on RUG. Urethroscopy is helpful to determine the caliber of the stricture in such cases; our practical general rule for questionable cases is that, if a 16-French flexible cystoscope can be passed through the area of narrowing, we do not offer surgical repair for those areas. In cases in which the patient has an obliterative stricture and a suprapubic tube has been placed, antegrade urethroscopy may be performed with the flexible cystoscope via the suprapubic tube tract.
Endoscopic management with urethrotomy or balloon dilation is performed if there are short, nonobliterative strictures. If a stricture is not amenable to endoscopic management or has failed previous attempts at endoscopic treatment, reoperative urethral surgical reconstruction is performed.
Preoperative evaluation
Nearly all patients with stricture recurrence after urethral reconstruction present with recurrent voiding symptoms. At first, imaging studies including retrograde urethrography (RUG) and voiding cystourethrography (VCUG), when possible, are performed because the radiographic appearance of strictures is known to change dramatically over time after intervention. Patients who have previously undergone urethroplasty, especially substitution techniques, often have irregularities on RUG. Urethroscopy is helpful to determine the caliber of the stricture in such cases; our practical general rule for questionable cases is that, if a 16-French flexible cystoscope can be passed through the area of narrowing, we do not offer surgical repair for those areas. In cases in which the patient has an obliterative stricture and a suprapubic tube has been placed, antegrade urethroscopy may be performed with the flexible cystoscope via the suprapubic tube tract.
Endoscopic management with urethrotomy or balloon dilation is performed if there are short, nonobliterative strictures. If a stricture is not amenable to endoscopic management or has failed previous attempts at endoscopic treatment, reoperative urethral surgical reconstruction is performed.
Surgical technique
We attempt to perform reconstruction in a single stage. If more than one stricture is present, we adapt an ascending approach used for primary repair of synchronous strictures. Patient positioning is determined by the location of the stricture (supine for pendulous strictures, adjustable stirrups are used for dorsal lithotomy positioning for bulbar or synchronous strictures requiring concomitant perineal exposure). Serious position-related complications are more common with prolonged time in high lithotomy. If a stricture is present in both the pendulous and bulbar urethra, we repair the pendulous portion first in low lithotomy before raising the legs to minimize time in high lithotomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






