Since the postulation of an “antiproliferative factor” in 1998 and a description, six years later, of this putative central protein in the etiologic pathway of the painful bladder syndrome/interstitial cystitis, there have been no dramatic breakthroughs in the field. Although much potentially exciting work is in progress with regard to epidemiology, etiology, and clinical treatment, many clinicians and researchers have used this hiatus to take another look at what exactly is being studied and how the syndrome should be approached. This article explores some of the current “hot-button” issues of definition and nomenclature that have formed the basis of many international meetings in the last 5 years.
New developments in infection/inflammation in urology Re-imagining interstitial cystitis
Since Keay postulated an “antiproliferative factor” (APF) in 1998 and described this putative central protein in the etiologic pathway of the painful bladder syndrome/interstitial cystitis (PBS/IC) six years later , there have been no dramatic breakthroughs in the field. Although much potentially exciting work—largely funded by the National Institute of Diabetes, Digestive, and Kidney Disorders (NIDDK) and with the essential support of the Interstitial Cystitis Association (ICA)—is in progress with regard to epidemiology, etiology, and clinical treatment, many clinicians and researchers have used this hiatus to take another look at what exactly is being studied and how the syndrome should be approached. This article explores some of the current “hot-button” issues of definition and nomenclature that have formed the basis of many international meetings in the last 5 years.
Definition
“When I use a word,” Humpty Dumpty said, in rather a scornful tone, “it means just what I choose it to mean—neither more nor less.” “The question is,” said Alice, “whether you can make words mean so many different things.” “The question is,” said Humpty Dumpty, “which is to be master—that’s all.”
Tage Hald refered to it as “a hole in the air” . It has been 20 years since the NIDDK proposed diagnostic criteria for entrance into research studies of interstitial cystitis (IC) , and so inadvertently defined the disorder for a generation of urologists. There has been a change in the way the disease (symptom complex, syndrome?) is perceived, and it is valuable to review briefly some of the ways it has been defined in the past ( Box 1 ).
1887 Skene : An inflammation that has destroyed the mucous membrane partly or wholly and extended to the muscular parietes.
1915 Hunner : A peculiar form of bladder ulceration whose diagnosis depends ultimately on its resistance to all ordinary forms of treatment in patients with frequency and bladder symptoms (spasms).
1951 Bourque : Patients who suffer chronically from their bladder; and we mean the ones who are distressed, not only periodically but constantly, having to urinate at all moments of the day and of the night suffering pains every time they void.
1978 Messing and Stamey : Nonspecific and highly subjective symptoms of around-the-clock frequency, urgency, and pain somewhat relieved by voiding when associated with glomerulations upon bladder distention under anesthesia.
1990 Revised NIDDK Criteria: Pain associated with the bladder or urinary urgency, and, glomerulations or Hunner’s ulcer on cystoscopy under anesthesia in patients with 9 months or more of symptoms, at least 8 voids per day, 1 void per night, and cystometric bladder capacity less than 350cc .
1997 NIDDK Interstitial Cystitis Database Entry Criteria: Unexplained urgency or frequency (7 or more voids per day), OR pelvic pain of at least 6 months duration in the absence of other definable etiologies .
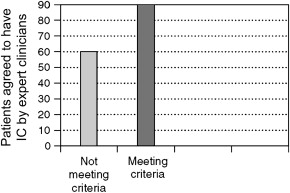
When the NIDDK-revised criteria were compared with the database entry criteria, it was apparent that up to 60% of patients clinically believed to have IC by experienced clinicians were being missed when the NIDDK research criteria were used as a definition of the disease ( Fig. 1 ) .
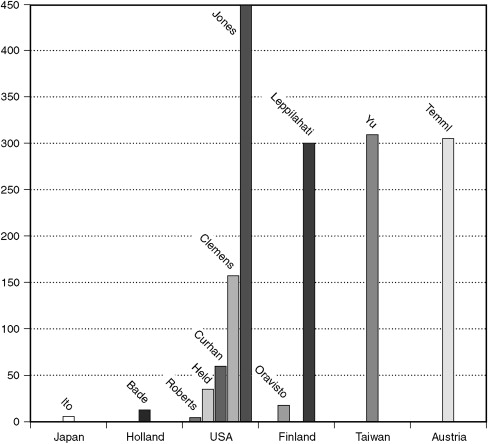
The lack of clarity in terms of definition is highlighted when looking at the results of numerous epidemiology prevalence studies that show widely disparate results, depending on how the disorder is defined ( Fig. 2 ) . These studies show prevalence rates in 100,000 females, from 1.8 when physician-assigned diagnoses were used in Olmstead County, Minnesota, to 450 when patients self-reported a diagnosis in the National Household Interview Survey . Interestingly, rates are surprisingly similar in Finland, Taiwan, and Austria (at about 300) when a high O’Leary-Sant symptom score is used as a surrogate for a diagnosis of IC (see Fig. 2 ) .
Unfortunately, histopathology does not help when it comes to defining this symptom. One can have bladder biopsies consistent with the diagnosis of IC, but there is no microscopic picture pathognomonic of this disorder. The role of histopathology in the diagnosis of IC is primarily one of excluding other possible diagnoses. Rosamilia and colleagues reviewed the pathology literature pertaining to IC and presented their own data . They compared forceps biopsies from 35 control and 34 IC patients, 6 with bladder capacities less than 400cc under anesthesia. Epithelial denudation, submucosal edema, congestion and ectasia, and inflammatory infiltrate were increased in the IC group. Submucosal hemorrhage did not differentiate the groups, but denuded epithelium was unique to the IC group and more common in those with severe disease. The most remarkable finding in this study was that histologic parameters were normal and indistinguishable from control subjects in 55% of IC patients. Method of biopsy can be important in interpreting findings, because transurethral resection biopsies tend to show mucosal ruptures, submucosal hemorrhage, and mild inflammation , whereas histology is normal approximately half the time with cold-cup forceps biopsies .
Keay’s finding that cells from the bladder lining of normal controls grow significantly more rapidly in culture than cells from IC patients, and her subsequent discovery and description of a frizzled 8 protein produced by bladder uroepithelial cells (APF) of IC patients, holds promise as a marker of the disease and, perhaps, a way to define it. As of 2007, neither have her findings been replicated by other centers, nor has a commercially available assay for APF been approved. The use of APF as a diagnostic marker and a part of the clinical definition of the syndrome remains tantalizing but not clinically accessible.
Is there a clinical test that, by virtue of its sensitivity and specificity, could be used to diagnose IC and thereby become a part of the definition of the disorder? Unfortunately, there is not. The potassium chloride test proposed by Parsons and colleagues —an intravesical challenge comparing the sensory nerve provocative ability of saline versus potassium chloride using a 0.4M-KCl solution—has not gained acceptance as a diagnostic test for a variety of reasons . It has neither the specificity nor the sensitivity to be used as a diagnostic test, and therefore results of the test could not be a part of any clinically useful definition.
As the new century dawned, there was much confusion as to how to define this 100-year-old syndrome, and the need for a clinically useful, universally accepted way to characterize IC took to the forefront. Abrams and the International Continence Society (ICS) preferred Bourke’s term “painful bladder” and defined painful bladder syndrome as “the complaint of suprapubic pain related to bladder filling, accompanied by other symptoms such as increased daytime and night-time frequency, in the absence of proven urinary infection or other obvious pathology.” Rather than drop the designation of IC all together, they limited it to patients with painful bladder who had “typical cystoscopic and histological features” without identifying those features . The term “urgency” was effectively taken out of the IC equation, and used to identify “ the complaint of a sudden compelling desire to pass urine which is difficult to defer. ” It became an integral part of the definition of overactive bladder: urgency with or without urge incontinence, usually with frequency and nocturia. Some degree of confusion has resulted , and patient organizations have not been happy to give up the urgency term, one that many patients identify with their IC symptoms . When looking at the Interstitial Cystitis Symptom Index (O’Leary-Sant ICSI), the ICSI question for urgency, “the strong need to urinate with little or no warning,” consistently yields lower scores than the severity question of “the compelling urge to urinate that is difficult to postpone” .
Warren compared the ICS painful bladder criteria with symptoms of patients he recruited for a case control study of newly diagnosed women with IC. His criteria for entrance into the study included women greater than 18 years of age with symptom onset within 12 months. They had greater than 4 weeks of perceived bladder pain at or greater than 3 on a 10-point Likert scale and at least two of frequency (≥8/24 hours), urgency (≥3 on a Likert scale), or nocturia. Exclusionary criteria were those of the NIDDK. He found that the ICS definition identified only 66% of his 138 cases. Those who met the definition did not differ from those who did not. The restriction to “suprapubic pain” in the ICS definition and the relationship of pain to filling were the criteria most responsible for the poor sensitivity.
Soon after the ICS terminology publication, several high-profile international meetings were held to tackle the problem of definition and nomenclature and establish a new framework for future collaborative research. Although each meeting had long, complex agendas, it is useful to look at how each approached the definition of the syndrome.
The first of these meetings was the International Consultation on Interstitial Cystitis Japan (ICICJ), held in Kyoto in March 2003, under the direction of Ueda, Sant, Yoshimura, and the present author . This meeting concluded by suggesting the following:
Interstitial cystitis should be suspected and further investigation is recommended in any patients with pelvic pain and urgency and/or urinary frequency associated with no obvious treatable condition/pathology. The term IC should be expanded to a term IC/CPPS (interstitial cystitis/chronic pelvic pain syndrome) when pelvic pain is at least of 3 months duration and associated with no obvious treatable condition/pathology.
The ICICJ was quickly followed by a meeting of a newly formed European Society for the Study of IC (ESSIC). The first meeting was held in Denmark in May 2003, with annual meetings thereafter. A process was begun that culminated in 2005 with the acceptance by ESSIC of the ICS definition of PBS with only minor modification . IC was a subset of PBS defined as:
A disease of unknown origin consisting of the complaint of suprapubic pain related to bladder filling accompanied by other symptoms, such as increased daytime (>8×) and nighttime (>1×) frequency, and with cystoscopic (glomerulations and/or Hunner’s lesions) and/or histological features (mononuclear inflammatory cells including mast cell infiltration and granulation tissue) in the absence of infection or other pathology.
On October 29 2003, the NIDDK convened a meeting of the members of the Interstitial Cystitis Epidemiology Task Force, the IC executive committee, ad hoc participants, and National Institutes of Health staff to review the status of current investigations of IC and to plan new epidemiology investigations . The following served as their working definition:
Interstitial cystitis is a symptomatic diagnosis based on the presence of three key symptoms: pain, urgency, and frequency, as well as exclusion of a short list of other conditions that cause the same symptoms. Pain is the most consistent and disabling symptom for IC patients. Some will not use the term pain, but will rather describe a sense of pressure or discomfort. Typically, but not always, the pain is worse with filling of the bladder and is relieved by emptying of the bladder. Urgency in IC patients differs from that experienced by patients with urinary incontinence. In IC patients, the urgency is driven by pain, in patients with incontinence (detrusor overactivity), it is driven by their fear of losing control. Not enough information is available on normal variability of urinary frequency to establish a number that can help diagnose IC.
Immediately following the epidemiology meeting, the NIDDK, in conjunction with the ICA, held a basic and clinical science symposium . It concluded: “The struggle to define IC will continue. Bladder pain will continue to be the key to the definition in the near future.”
In June 2004 the third International Consultation on Incontinence, cosponsored by the International Consultation on Urological Diseases in official relationship with the World Health Organization, the International Society of Urology, the ICS, and the major international associations of Urology and Gynecology, adopted the ICS definition of IC and PBS. It noted that because of the ambiguity in defining IC as a subset of PBS, the terms would be used together to refer to the same constellation of symptoms (PBS/IC) . Further, it concluded that: “Interstitial cystitis is a clinical diagnosis primarily based on symptoms of urgency/frequency and pain in the bladder and or pelvis. The combined term PBS/IC will be used until more specific criteria can be established.”
Soon after the International Consultation on Incontinence, the Multinational Interstitial Cystitis Association met to carry the discussion forward . The group kept the ICS definition of PBS, but broadened the symptom of pain to include “pressure” and “discomfort.” The group went on to note:
Interstitial cystitis may be a subgroup of this larger syndrome (PBS) … but as this remains somewhat vague, a general nomenclature is preferred and the question of what is “IC” alone is left to be determined. Urgency is a common complaint of this group of patients. The ICS definition of urgency could be interpreted as compatible with either detrusor overactivity of PBS/IC. Because the term of urgency would tend to obfuscate the borders of these two conditions and may be unnecessary as a part of the definition of PBS/IC, its place in the definition will need to be worked out in conjunction with the ICS terminology committee.
The ESSIC presented a comprehensive report at the NIDDK 2006 “Frontiers in Painful Bladder Syndrome and Interstitial Cystitis” meeting in October 2006. In response to a decision made public there by the ESSIC to drop the moniker “interstitial cystitis” in favor of “bladder pain syndrome”—which was to be further categorized by results of optional investigations (see below)—the ICA, in conjunction with the Association of Reproductive Health Professionals, held a meeting in Washington, DC. The meeting included a cross-section of invited American urologists, gynecologists, nurses, and representatives from the German patient organization and a urologist from Germany. The following definition was promulgated at the meeting and is available at http://www.arhp.org/healthcareproviders/visitingfacultyprograms/icpbs/whitepaper.cfm : IC/PBS is defined by pelvic pain, pressure, or discomfort related to the bladder, typically associated with persistent urge to void or urinary frequency, in the absence of infection or other pathology.
The term “persistent urge” was meant to include the idea of urgency in the definition while not directly impinging on the ICS’s use of the term as defined for overactive bladder.
In a compromise presented at the second International Consultation on Interstitial Cystitis Japan, in March 2007, the ESSIC agreed to modify the name and definition to be acceptable to all stakeholders. This was confirmed at their meeting in Muenster, in May 2007.
Bladder pain syndrome/interstitial cystitis would be diagnosed on the basis of chronic pelvic pain, pressure or discomfort perceived to be related to the urinary bladder accompanied by at least one other urinary symptoms like persistent urge to void or urinary frequency. Confusable diseases as the cause of the symptoms must be excluded. Further documentation and classification of BPB/IC might be performed according to findings at cystoscopy with hydrodistention and morphological findings in bladder biopsies.
Definition
“When I use a word,” Humpty Dumpty said, in rather a scornful tone, “it means just what I choose it to mean—neither more nor less.” “The question is,” said Alice, “whether you can make words mean so many different things.” “The question is,” said Humpty Dumpty, “which is to be master—that’s all.”
Tage Hald refered to it as “a hole in the air” . It has been 20 years since the NIDDK proposed diagnostic criteria for entrance into research studies of interstitial cystitis (IC) , and so inadvertently defined the disorder for a generation of urologists. There has been a change in the way the disease (symptom complex, syndrome?) is perceived, and it is valuable to review briefly some of the ways it has been defined in the past ( Box 1 ).
1887 Skene : An inflammation that has destroyed the mucous membrane partly or wholly and extended to the muscular parietes.
1915 Hunner : A peculiar form of bladder ulceration whose diagnosis depends ultimately on its resistance to all ordinary forms of treatment in patients with frequency and bladder symptoms (spasms).
1951 Bourque : Patients who suffer chronically from their bladder; and we mean the ones who are distressed, not only periodically but constantly, having to urinate at all moments of the day and of the night suffering pains every time they void.
1978 Messing and Stamey : Nonspecific and highly subjective symptoms of around-the-clock frequency, urgency, and pain somewhat relieved by voiding when associated with glomerulations upon bladder distention under anesthesia.
1990 Revised NIDDK Criteria: Pain associated with the bladder or urinary urgency, and, glomerulations or Hunner’s ulcer on cystoscopy under anesthesia in patients with 9 months or more of symptoms, at least 8 voids per day, 1 void per night, and cystometric bladder capacity less than 350cc .
1997 NIDDK Interstitial Cystitis Database Entry Criteria: Unexplained urgency or frequency (7 or more voids per day), OR pelvic pain of at least 6 months duration in the absence of other definable etiologies .
When the NIDDK-revised criteria were compared with the database entry criteria, it was apparent that up to 60% of patients clinically believed to have IC by experienced clinicians were being missed when the NIDDK research criteria were used as a definition of the disease ( Fig. 1 ) .







