Chapter 41 Radiology of Minimally Invasive Abdominal Surgery
Imaging techniques
Laparoscopic cholecystectomy
Normal Imaging Findings after Uncomplicated Laparoscopic Cholecystectomy
Common Bile Duct Stones
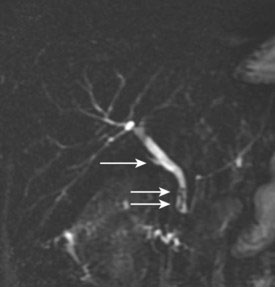
Retained stones can cause partial or complete biliary obstruction after laparoscopic cholecystectomy. Although intraoperative cholangiography is the gold standard for detecting choledocholithiasis during cholecystectomy, MRCP is valuable in the preoperative and postoperative detection of CBD stones (Fig. 41-1). Small gallstones may migrate into the CBD in the patient with a patulous cystic duct during cephalad retraction of the gallbladder. ERCP is useful in diagnosing and treating these cases.
Bile Leakage
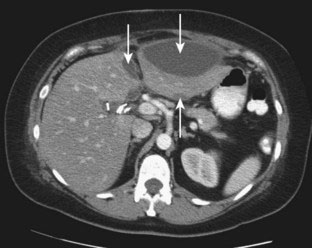
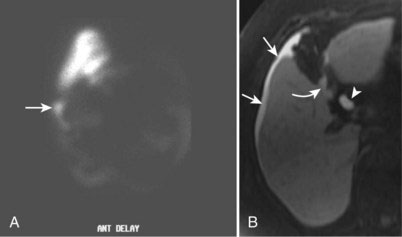
Bile leakage is one of the most common complications of laparoscopic cholecystectomy. Most leaks occur from the cystic duct stump. Other causes include laceration, transection, or thermal injury of the CBD or an unrecognized anomalous duct. CT and ultrasound are the initial imaging studies performed in the postoperative patient with suspected bile leak or biliary sepsis. Although both studies are useful in detecting intra-abdominal fluid collections, neither can differentiate between lymphocele, hematoma, seroma, or biloma (Fig. 41-2). Cross-sectional imaging studies can show a fluid collection in the gallbladder fossa, but such imaging cannot determine whether there is active bile leakage. Hepatobiliary scintigraphy (Fig. 41-3A), ERCP, or percutaneous transhepatic cholangiography (PTC) can show an active bile leak and the site of leakage. MRI employing gadoxetate disodium (Eovist), a gadolinium-based agent that is excreted in the bile, also is effective in showing bile leakage (Fig. 41-3B).
Acute Biliary Obstruction and Bile Duct Injury
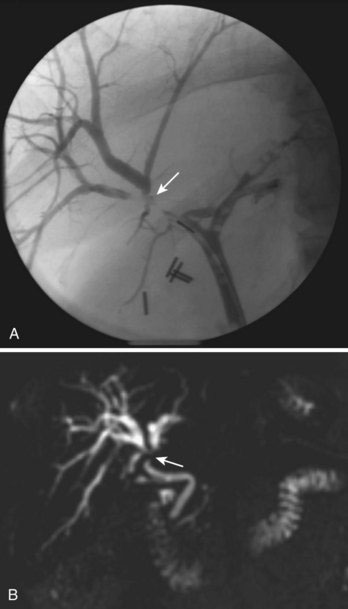
A bile duct injury typically manifests with biliary dilation (Fig. 41-4) or bile leakage. The site of injury is described according to the Bismuth classification. A Bismuth type 1 injury indicates a remaining (noninjured) common hepatic duct longer than 2 cm; a type 2 injury has a remaining common hepatic duct shorter than 2 cm; a type 3 injury is located at the confluence of the right and left hepatic ducts; a type 4 injury extends into the right and left hepatic ducts. Major ductal injury from laparoscopic cholecystectomy generally is high in the biliary system, and multiple ducts often are involved. Mechanisms of CBD injury include malpositioning of surgical clips, thermal injury from sealing and cauterizing instruments, sharp incision, and en bloc excision.
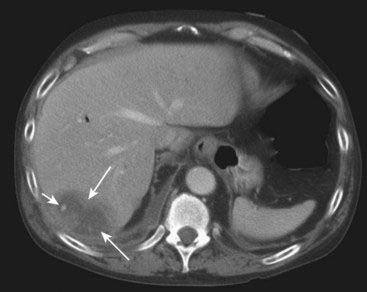
Hemorrhage
Hemorrhage after laparoscopic cholecystectomy (Fig. 41-5) may occur from the cystic artery stump or the right hepatic artery. Bleeding may be secondary to thermal or mechanical injury, as with bile duct injury, or from dislodged hemostatic clips. Bleeding also can occur at a trocar insertion site, from the omentum or abdominal wall. MDCT is the most effective method for detecting bleeding because it will show the hyperdense hemorrhage and may show a focus of active bleeding or a pseudoaneurysm on contrast-enhanced scans. Transcatheter arterial embolization or surgical hemostasis may be considered, particularly if extravasation of the intravenous contrast agent is seen.
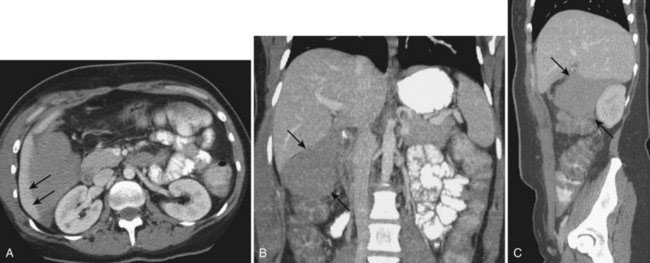
Abscess with Retention of Peritoneal Gallstones or Spilled Clips
Gallstone and bile spillage develops in up to one third of patients during laparoscopic cholecystectomy. Dropped stones can lodge in virtually any crevice of the abdominal cavity. The combination of pneumoperitoneum and peritoneal irrigation may disperse the calculi throughout the peritoneal cavity. Stones have been reported in the right pleural space and have eroded into to colon. Abscess formation occurs in about 0.6% of patients in whom bile spillage alone occurs and in 0.6% to 2.9% of cases in whom both bile and stone spillage occurs. An abscess also can be associated with dropped surgical clips. Most abscesses associated with unretrieved peritoneal gallstones or spilled clips are seen in the perihepatic space (Fig. 41-6), but they may occur anywhere in the peritoneal cavity. Visualization of the spilled stone or clip in the abscess is the key to the radiologic diagnosis of this entity. Sonographically, a typical abscess appears as an echogenic focus with posterior acoustic shadowing. On MDCT, a central or eccentric calcified stone or metallic nidus may be identified.
Trocar Site Hernia
An umbilical hernia at the Hasson cannula site is the most common type of trocar hernia, which generally occurs within a few days of surgery and often presents with small bowel obstruction. It can take several months, however, before symptoms of a trocar hernia develop. If the hernia causes small bowel obstruction (Fig. 41-7) and strangulation, operative intervention is needed. A trocar hernia also may be complicated by panniculitis.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree