Fig. 33.1
Different types of tumor growth in the cervix (exophytic, endocervical, deep stromal)
Early Stages
Patients with micro invasive carcinoma stage FIGO IA (stromal invasion ≤5 mm; horizontal extension ≤7 mm) have an excellent prognosis and, not surprisingly, minimal risk of parametrial invasion [1, 27, 65]. Simple extrafascial hysterectomy is an appropriate surgery in this case. In recent years a number of reports show that satisfactory outcomes can be achieved even in selected patients (largest tumor size ≤2 cm, stromal invasion ≤2/3; negative pelvic lymph nodes) with IB stage when parametrectomy is not performed [21, 50]. These reports are supported by arguments from retrospective series substantiating low risk of parametria involvement in this very group of patients [21, 63]. However, these retrospective series are limited by standard parametrial pathological processing which does not enable small size metastasis detection, particularly tumor emboli in lymphatic channels. Therefore the standard surgical procedure in stage IB should, according to current knowledge, be radical hysterectomy, which means including parametria removal. Any change in the guidelines should be preceded by the confirmation of oncological safety in ongoing prospective trials (SHAPE—Simple Hysterectomy and Pelvic Node Dissection in Early Stage Low Risk Cervical Cancer).
Locally Advanced Staged
A broad range of alternatives is currently applied in the management of locally advanced stages (IB2, IIA, IIB): (a) Primary chemoradiation, (b) neoadjuvant chemotherapy followed by radical hysterectomy, (c) neoadjuvant radiotherapy followed by simple or radical hysterectomy, or (d) upfront radical surgery with or without adjuvant radiotherapy or chemotherapy. It is necessary to emphasize that as a result of the massive improvement of imaging diagnostics (MRI, ultrasound, PET) clinical staging, including the assessment of parametrial, paracolpial or pelvic lymph nodes involvement, has become much more accurate. It can be assumed that the spectrum of patients classified into stage IB2 or IIB is currently much more accurate compared to 5 or 10 years ago.
Primary surgical treatment of large tumors or tumors with initial parametrial invasion is feasible and it has, according to available data, a satisfactory oncological outcome comparable with radiotherapy [10, 26]. Surgical approach has two main limitations though. Extensive parametrectomy (type C2 or D) must be performed due to anatomical conditions in patients with massive tumors, a high risk of parametrial metastatic involvement in stage IB2 or the presence of parametrial invasion in patients with stage IIB. Furthermore, the proportion of patients referred to adjuvant treatment for lymph node involvement is high in these stages, reaching up to 40 % [12]. Postoperative morbidity increases in a large number of patients due to the accumulation of two different treatment modalities—extensive surgical procedure and adjuvant radiotherapy. Prospective studies are necessary to refine the management of locally advanced stages, as they would compare oncological outcome and their impacts on quality of life in each treatment modality.
33.4 Terminology
The unification of terminology describing the key anatomical structures is crucial for international understanding and comprehension. One of the key structures for radical hysterectomy is the parametrium, which has three components on both sides of the cervix: the ventral parametrium (including vesico-uterine and vesico-vaginal ligaments), the lateral parametrium (paracervix or cardinal ligament), and the dorsal parametrium (including recto-uterine and recto-vaginal ligaments) (Fig. 33.2). The term “mesoureter” describes the lateral laminar part of the dorsal parametria, which is stretched dorsally and caudally from the ureter and contains the inferior hypogastric plexus [62].
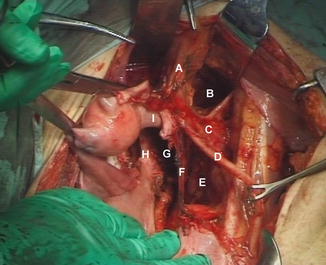
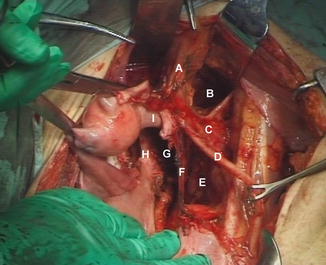
Fig. 33.2
Intra-operative picture of the ventral, lateral and dorsal parametrium. A Ventral parametrium, B paravesical space, C lateral parametrium, D ureter, E pararectal space (lateral pararectal space), F dorsal parametrium, G sacro-uterine space (medial pararectal space), H rectum, I cervix
Two parts of the ventral parametria are recognized in sagittal plane—cranial (above the ureter) and caudal (below the ureter), divided by the course of the ureter. Two different spaces are described dorsally—the sacro-uterine space (medial pararectal space) between the rectum and the dorsal parametrium, and the pararectal space between the dorsal parametrium and iliac vessels (Fig. 33.2). The deep uterine vein (vaginal vein) is an important landmark in the lateral parametrium (Fig. 33.3). In most cases there is not only one but a few veins in the lateral parametrium, and it is the largest one which is called the vaginal vein, usually located about 1–2 cm below the uterine artery and vein.
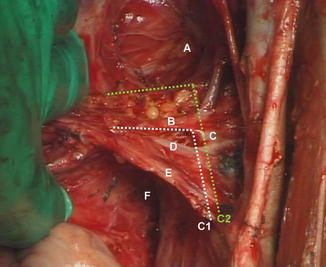
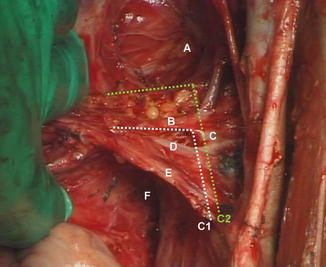
Fig. 33.3
Intra-operative picture of resection lines on the lateral parametrium A paravesical space, B deep uterine vein (vaginal vein), C internal iliac vein, D uterine vein, E uterine artery, F pararectal space. C1, C2 resection lines on the lateral parametrium for types C1 and C2 radical hysterectomy
33.5 Classification
Different classifications are currently used to describe individual types of radical hysterectomy. Most historical classification systems do not include an unambiguous and precise description and specification of anatomical landmarks. As a consequence, the extent of the parametria resection varies substantially among institutions and surgeons, even if the same terminology is used. In many institutions, one type of “universal” or “classical” radical hysterectomy is used even though it is unclear with what kind of parametria resection it corresponds.
Principles of Classification
Modern classification of radical hysterectomy should be based on the following principles:
(a)
The key and sole parameter for differentiation between types of radical hysterectomy is the extent of parametria resection. The resection or removal of other organs or structures (i.e. urinary bladder, ureter, rectum, pelvic floor muscle) is not included in the classification system. Also, the size of the removed vaginal cuff is not a decisive parameter for type of procedure.
(b)
The extent of resection should be precisely defined for all three parts of the parametria (ventral, lateral, dorsal) in all three planes (sagittal, frontal and transverse). The resection margins in the vertical (deep parametrial) dimension determine long term morbidity due to the location of autonomic nerves.
(c)
Although the classification system is usually proposed for radical hysterectomy, it is applicable to the radical trachelectomy and the radical parametrectomy.
(d)
Surgical margins should be defined by stable anatomical landmarks. There are a few of such structures eligible in the pelvis, such as urinary bladder, rectum, ureter, large vessels, and nerves.
(e)
The classification system must be sufficiently comprehensible and simple to allow for easy reproducibility.
ABCD Classification System
The classification system described in this chapter was first published by Querleu and Morrow in 2008 [52], and later extended into a 3D model [11]. Five types of the procedure (A, B, C1, C2, D) correspond to other common historical types of radical hysterectomy (Table 33.1). The new classification system has some exceptional aspects to it: (a) recognizes the size and type of parametria resection as the crucial and sole parameter for classification, (b) includes new type of nerve sparing procedure, (c) uses stable anatomical landmarks for description of surgical resection margins, (d) identifies surgical landmarks in three planes—frontal, sagittal and transverse.
Table 33.1
ABCD classification system and corresponding historical types of radical hysterectomy
New classification system | Corresponding types |
|---|---|
A | Extrafascial hysterectomy |
B | Modified radical hysterectomy |
Type II radical hysterectomy | |
C1 | Nerve sparing radical hysterectomy |
C2 | Type III radical hysterectomy |
Classical/standard radical hysterectomy | |
D | Laterally extended parametrectomy |
Type A corresponds to the extrafascial hysterectomy, the main principle of which is pericervical tissue removal up to the attachment of vaginal fornices. The ureter does not need to be identified or dissected in the parametrium, parametria are not resected and autonomic nerves remain fully preserved.
Type B corresponds mostly to the modified radical hysterectomy. Ureter is the major resection margin ventrally and laterally (Fig. 33.4). It must be identified in the parametrium, its course is unroofed, dissected from the cervix and displaced laterally, but not dissected from the lateral or ventral parametria. Such extent of distal ureteral dissection enables the resection of only a small initial part of the ventral and lateral parametria. Identification of autonomic nerves is not required, and the hypogastric plexus remains hidden in a deeper part of the parametria, thus remaining fully preserved.
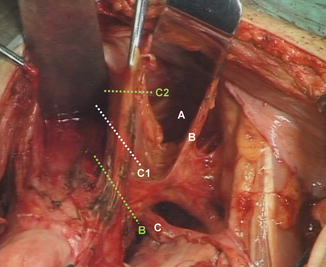
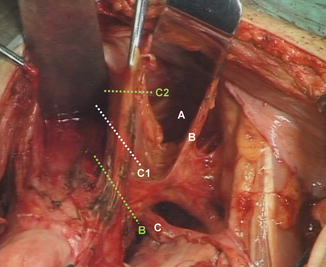
Fig. 33.4
Intra-operative picture of horizontal resection lines on the ventral parametrium A paravesical space, B umbilical ligament, C ureter. B, C1, C2 resection lines on the ventral parametrium for types B, C1 and C2 radical hysterectomy
There are significant differences, particularly in the vertical (deep parametrial) dimension, between type C1, which corresponds to the nerve-sparing procedure, and type C2, which aims for a complete parametrial resection. In type C1 the ureter is unroofed, dissected from the cervix and lateral parametria, but only partially from the ventral parametria, while type C2 requires complete dissection of the ureter from the ventral parametria up to the urinary bladder wall. Laterally, resection margins in a transverse plane are identical for both types, formed by the medial aspect of the internal iliac vein (Fig. 33.4). In type C1 the deep parametrial resection margin on the lateral parametria is formed by the deep uterine vein (vaginal vein), which is a large vein located about 1–2 cm below the uterine artery and vein (Fig. 33.3). As such the caudal part of the lateral parametria containing the splanchnic nerves is preserved. In type C2 the resection line continues alongside the medial aspect of the internal iliac vessels up to the sacral bone (Fig. 33.3). Such deep resection allows for greater mobility of the lateral parametria, facilitating its complete removal. Ventrally, in type C1 a partial dissection of the ureter from the ventral parametria allows for limited resection in a sagittal plane of 1–2 cm of the ventral parametria (Fig. 33.5). Even more important is a vertical resection margin on the ventral parametria, which must be at the level of ureter to preserve bladder branches of the hypogastric plexus localized below the course of the ureter [29, 30]. In type C2, a complete dissection of the ureter from the ventral parametria is required, which allows for complete resection of the ventral parametria up to the urinary bladder wall (Fig. 33.5). Bladder branches of the hypogastric plexus are sacrificed. Dorsally, type C1 requires separation of two parts of the dorsal parametria: the medial part, which is composed by the recto-uterine and recto-vaginal ligaments, and the lateral laminar structure, which contains the hypogastric plexus, also called the mesoureter (Fig. 33.6). Main branches of the hypogastric plexus are preserved on the lateral part (mesoureter), while recto-uterine and recto-vaginal ligaments can be resected at the level of its rectal attachment. Type C2 aims to a complete resection of the dorsal parametria deeply below the rectal attachment, so that separation of major branches of the hypogastric plexus is not needed and these nerves are sacrificed (Fig. 33.6).
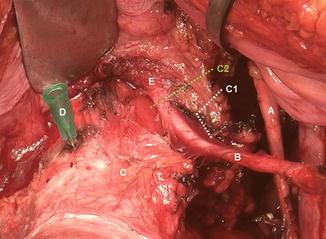
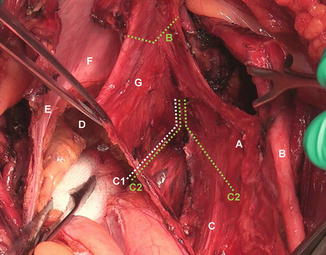
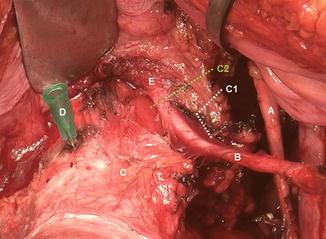
Fig. 33.5
Intra-operative picture of resection lines on the ventral parametrium (ureter unroofed) A umbilical ligament, B ureter, C cervix, D needle indicating level of vaginal fornix, E distal ureteral entrance into the bladder. C1, C2 resection lines on the ventral parametrium for types C1 and C2 radical hysterectomy
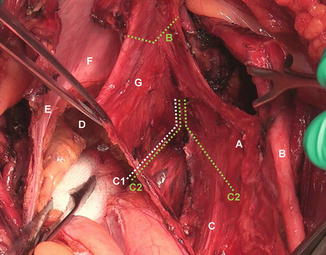
Fig. 33.6
Intra-operative picture of resection lines on the dorsal parametrium A mesoureter; B ureter, C branches of the hypogastric plexus (white strips), D rectovaginal space, E left dorsal parametrium (mesoureter not yet dissected from recto-uterine ligament), F cervix, G recto-uterine ligament. B, C1, C2 resection lines on the dorsal parametrium for types B, C1 and C2 radical hysterectomy
Type D differs from type C2 only in a lateral extent of the lateral parametria resection. Ureteral dissection and resection of both dorsal and ventral parametria is identical to type C2. Laterally, however, it requires ligation and removal of internal iliac artery and vein, together with their branches, including gluteal, internal pudendal and obturator vessels. Lateral resection line is formed by the lumbosacral nerve plexus, piriformis muscle and obturator internal muscle.
33.6 Procedure Performance
Procedure performance depends mostly on the type of radical hysterectomy. The sequence of each procedure step can vary according to surgeon’s preference. Pelvic lymphadenectomy, which is typically part of the procedure, is preferably performed at the beginning as it enables better pelvic structure identification. The entire procedure can be divided into a few steps:
Lateral Dissection
Round ligament is identified at the beginning of the procedure, cut through and the retroperitoneum is broadly exposed above the external iliac vessels. Paravesical and lateral pararectal spaces are opened by blind dissection and the lateral parametrium remains revealed between these two spaces. Umbilical ligament is dissected from the ventral parametria and preserved. The origin of the uterine artery is identified on the medial aspect of internal iliac artery; at this point it is interrupted, usually together with the uterine vein, localized below the artery. Now the lateral parametrium can be dissected from the pelvic side wall—lateral resection margin is formed by the medial aspect of internal iliac vein—caudal margin depends on the type of radical hysterectomy, formed by the deep uterine vein in type C1, while dissection continues up to the sacral bone in type C2. Type D requires ligation and resection of both internal iliac vessels.
Distal Dissection of the Ureter
Ureter is identified on the posterior leaf of broad ligament; it is sharply mobilized up to its entrance to lateral parametria. Mobilization of the distal ureter requires caudal dissection of the urinary bladder from the cervix and proximal vagina. Ureteral tunnel in the lateral parametrium is blindly opened; parametria resected above the ureter and the ureter is completely mobilized from the cervix and ventrally from the upper vagina. Such dissection of distal ureter is adequate for type B, while type C1 requires complete mobilization of the ureter from lateral parametria, whereas for type C2 additional complete dissection from ventral parametria up to its entrance into the urinary bladder is necessary.
Ventral Dissection
The extent of urinary bladder caudal dissection is determined by the projected size of vaginal cuff removal. The extent of ventral parametrial resection depends on the type of radical hysterectomy: ventral parametria are not resected in type B, while about 2 cm of proximal part located above the ureter is removed in type C1. In type C2 and D after the ureter has been fully dissected, ventral parametrium is resected completely at the bladder wall.
Dorsal Dissection
The rectovaginal peritoneal flap is cut and rectum is caudally dissected from the vagina and lateral parametria. Dorsal parametria are resected in the extent of 1–2 cm in type B. Type C1 requires separation of two parts of the dorsal parametria—hypogastric plexus is preserved in laterally separated part (mesoureter) while sacrouterine and sacrovaginal ligaments can be resected at the level of its attachment into the rectum. Separation of two parts of the dorsal parametrium is not required for type C2 or D as dorsal parametria are completely resected and hypogastric plexus is inevitably sacrificed.
Final Specimen Removal
Finally the paracolpium is interrupted in transverse plane at the level of intended vaginal resection, the vagina is resected and vaginal cuff sutured, preferably by submucosal closure which allows for further complete visualization of the upper vagina during the follow-up.
33.7 Choice of Radical Hysterectomy Type
The type of radical hysterectomy is determined by a number of prognostic factors: tumor size, depth of stromal invasion, presence of LVSI (lymphovascular invasion), or lymph node status. Indication criteria for C2 resection are not uniform, these procedures are typically performed in bulky tumors with their size bigger than 4 cm, also when two-thirds of cervical stroma is involved, when tumors invade into uterine isthmus and also in tumors of stage IIB with initial invasion into parametria. Type B or C1 should be preferred in small size tumors with negative lymph nodes with the intention to decrease postoperative morbidity thanks to autonomic nerve preservation. From the above description it is obvious that type B hysterectomy only enables a small part of parametria removal—it is a task for future studies to prove if this extent of parametrectomy brings any benefit for oncological outcome or if an identical outcome can be achieved in the same size tumors when simple hysterectomy is performed. Type D radical hysterectomy is done rarely, mostly for central pelvic recurrences or locally advanced tumors [42].
33.8 Pre-operative Procedure Description
An accurate surgical plan should be determined conclusively before every single procedure. Considering the above-mentioned principles of radical hysterectomy classification it is obvious that the type of radical hysterectomy purely describes the radicality of the surgery performed on parametria. For an adequate description of the procedure performance, the following parameters should be specified pre-operatively: (a) procedure on the adnexa (i.e. salpingo-oophorectomy; ovarian transposition.); (b) type of lymph node dissection (i.e. sentinel node biopsy, pelvic lymphadenectomy and its type, paraaortic lymphadenectomy and its cranial extent); (c) size of the vagina removal; (d) type of the procedure (radical hysterectomy, radical parametrectomy, radical trachelectomy), and (e) extent of parametria removal (classification system—type A–D).
33.9 Surgical Approach
An alternative to classical radical hysterectomy performed by laparotomy is an endoscopic approach. These procedures can be performed fully by laparoscopy or robotically or in combination with vaginal approach (LARVH—laparoscopic assisted radical vaginal hysterectomy; VALRH—vaginal assisted laparoscopic radical hysterectomy). Feasibility of both minimally invasive approaches, laparoscopic or robotic surgery, were well proven in early stages, locally advanced stages, old patients, obese patients, or for nerve sparing type (type C1) of radical hysterectomy [14, 23, 25, 31, 38, 40, 43, 44, 61].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








