Background
Radiation therapy (RT) has been considered one of the standard therapeutic approaches for the treatment of prostate cancer since the 1950s. It was believed that RT offered comparable results to the standard radical perineal prostatectomy, with less morbidity. Since that time there have been substantial advances in both surgical and RT techniques. With regard to RT, technological advances in both treatment planning and delivery have resulted in significant improvements in efficacy with a corresponding reduction in morbidity, particularly in the last 20 years.
Standard therapeutic approaches to localized prostate cancer include radical prostatectomy (retropubic or perineal), robot-assisted laparoscopic prostatectomy, external beam radiotherapy (EBRT), high dose rate and low dose rate brachytherapy and combinations of external beam radiotherapy with brachytherapy. Several factors should be considered when selecting a treatment option. One would be risk of failure based on clinical stage, prostate-specific antigen (PSA) level, and Gleason score. Specific initial therapies are recommended according to whether the risk category is low, intermediate or high, referring to the patient’s risk of recurrence after therapy. Low risk is defined by the National Comprehensive Cancer Network (NCCN) as men with stage T1–T2a prostate cancer, a Gleason score between 2 and 6, and a PSA value ≤ 10 ng/mL. Intermediate risk is defined as any T2b–T2c cancer or any Gleason 7 score or PSA value between 10 and 20 ng/mL. High risk is defined as those with T3a–T3b prostate cancer, a Gleason score of 8–10 or a PSA value > 20 ng/mL. Other factors to consider when recommending treatment options include patient’s life expectancy, underlying medical conditions, and patient preference.
This chapter aims to present evidence available on several topics in which there has been a reasonable degree of consensus achieved. The topics included in the chapter will address external beam radiotherapy dose, intensity-modulated radiation therapy (IMRT) versus three-dimensional conformal radiotherapy (3D-CRT), as well as patient selection for pelvic lymph node irradiation, brachytherapy and androgen deprivation therapy.
Clinical question 29.1
What is the optimal dose for the treatment of localized prostate cancer with external beam radiotherapy?
Literature search
We performed a literature search using PubMed and Medline. Search terms included combinations of the following: “prostate cancer,” “IMRT,” “three-dimensional conformal radiation therapy,” “dose escalation,” “randomized controlled trials.” No time frame limitations were applied.
The evidence
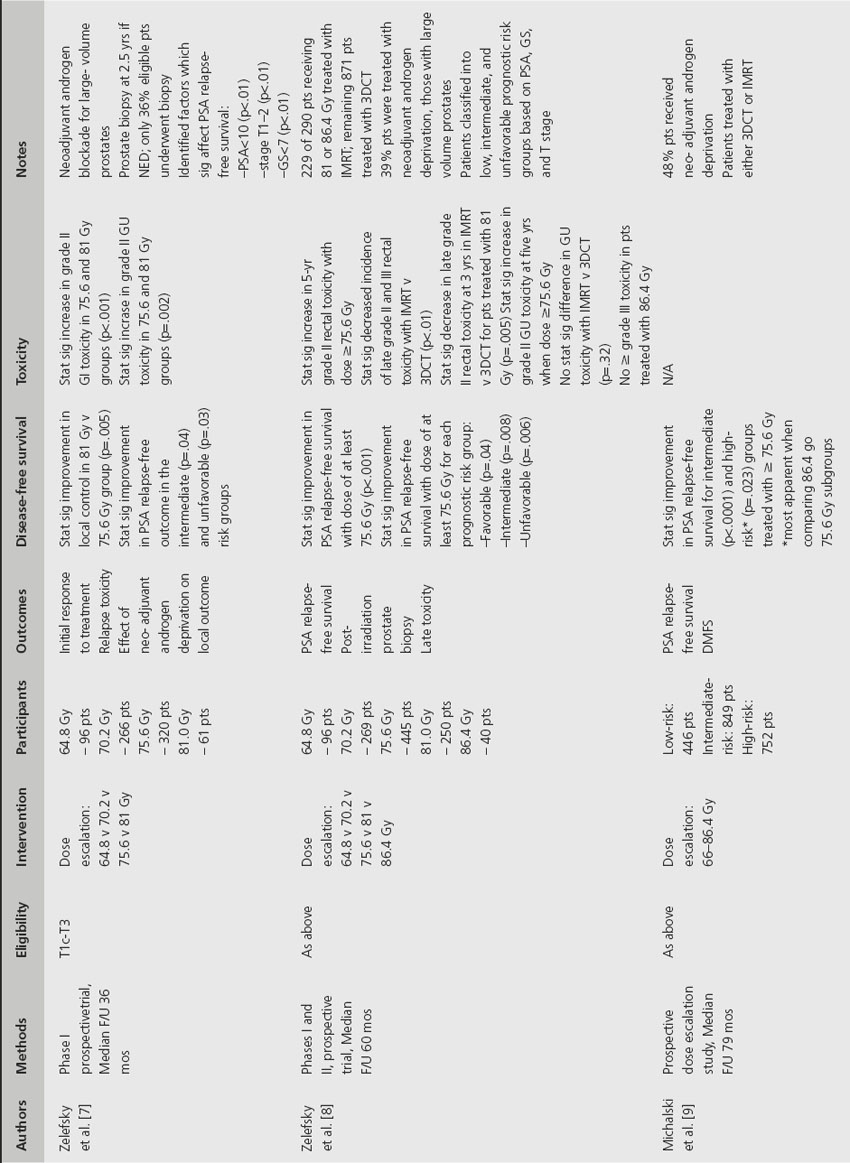
The advent of 3D-CRT and subsequently IMRT provided the capability to deliver higher doses, with an acceptable risk of toxicity, for the treatment of prostate cancer. There have been several single-institution prospective phase I/II trials confirming the benefits of dose escalation as well as a small number of phase III randomized controlled trials (Table 29.1).
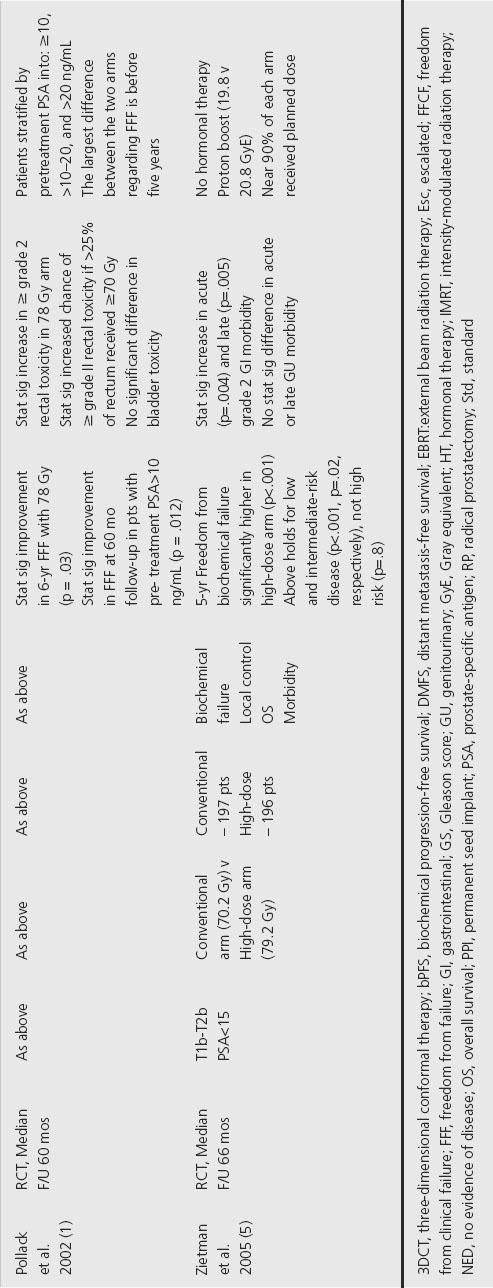
A prospective RCT reported by Pollack et al. enrolled 301 patients with T1–T3 prostate cancer to receive 70 Gy versus 78 Gy [1]. The 6-year PSA relapse-free survival (RFS) for the 70 vs 78 Gy arms were 64% vs 70% (p = 0.03), respectively. Subgroup analysis detected no significant benefit when patients had PSA levels < 10. Recently, the update to this study reported by Kuban et al. found the benefit of dose escalation remained significant with maturation of the study [2]. The difference in PSA RFS outcomes between the two study arms increased with time (78% vs 59% at 8 years, and 73% vs 50% at 10 years). With the longer follow-up, a benefit was now seen for the first time in patients with low-risk disease (8-year PSA RFS of 63% vs 88% for those treated with 70 Gy vs 78 Gy, respectively, p = 0.042).
Table 29.1 Effect of dose escalation trials for localized prostate cancer
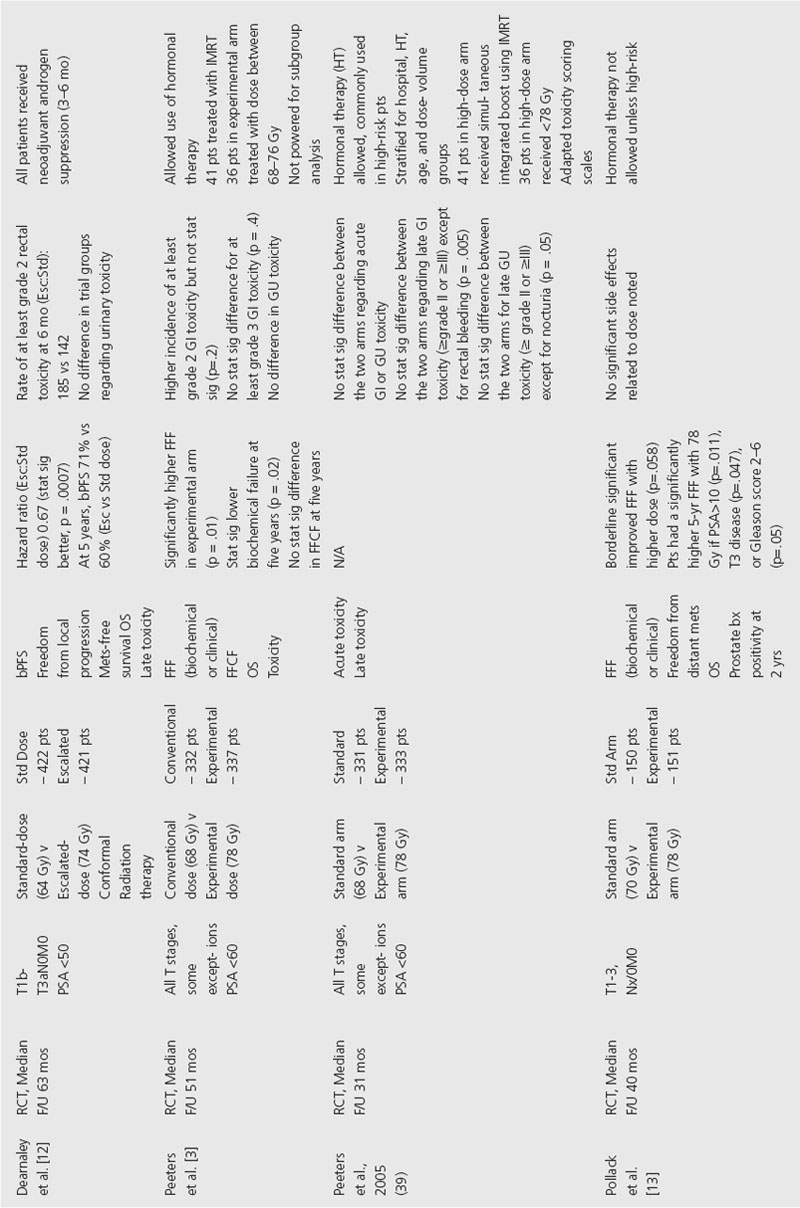
A multicenter RCT from The Netherlands, reported by Peeters et al., enrolled 664 patients with stage T1b–4 prostate cancer to receive either 64 Gy or 74 Gy [3]. Eligibility criteria were adenocarcinoma of the prostate including all T stages with PSA less than 60 ng/mL, except T1a and well-differentiated (Gleason score < 5) T1b–c tumors with PSA < 4 ng/mL. They reported a significant benefit in freedom from failure (FFF) at 5 years of 54% versus 64% for the groups receiving 64 Gy and 74 Gy, respectively. FFF was defined as no clinical evidence of disease or biochemical recurrence by ASTRO definition (three consecutive increases in PSA level after a nadir).
A RCT from the United Kingdom, reported by Dearnaley et al., studied 843 men with localized prostate cancer treated with 3D-CRT to a dose of 64 Gy versus 74 Gy [4]. Eligibility criteria included histological confirmed T1b–T3aN0M0 prostate cancer. All patients received androgen suppression consisting of a luteinizing hormone-releasing analog accompanied by antiandrogen treatment at first to prevent disease flare. They reported a 71% vs 60% biochemical progression-free survival (bPFS) at 5 years in the escalated vs standard groups, respectively (hazard ratio (HR) 0.67 95% confidence interval (CI) 0.53–0.85). Subgroup analysis found a significant bPFS for dose escalation in the high-risk group (HR 0.60, 95% CI 0.44–0.81), but no statistically significant benefit in the intermediate- or low-risk groups.
Zietman et al. conducted a RCT of dose escalation employing a combination of proton therapy as a boost following conventional photon external beam therapy [5]. They studied 393 patients with stage T1b through T2b prostate cancer and PSA levels less than 15 ng/mL who received either 70.2 cobalt gray equivalents (CGE) or 79.2 CGE. The treatment was delivered using a conformal photon dose of 50.4 Gy with a proton beam boost dose of either 19.8 Gy or 28.8 Gy, for total doses of either 70.2 CGE or 79.2 CGE. The 5-year freedom from biochemical failure was 61.4% for conventional-dose and 80.4% for high-dose therapy (p < 0.001). When subgroup analysis was performed the authors observed a significant benefit in both low-risk and intermediate-risk patients, but no benefit in the high-risk group.
Hanks et al. reported the phase I/II experience from Fox Chase in which they confirmed the direct relationship between dose and PSA outcome in patients when comparing doses from 70 Gy up to 78 Gy [6]. This study also divided the group into six subgroups based on PSA value (< 10, 10–19.9, ≥ 20) as well as favorable (stage T1–T2a, GS < 7) and unfavorable (stage T2b–T3, GS 7–10) risk groups. There was a significant 5-year PSA RFS in three of the six subgroups including PSA < 10 unfavorable, PSA 10–19.9 unfavorable and PSA ≥ 20 favorable. The authors concluded that a dose between 70 and 80 Gy is absolutely critical except for the most favorable and the most unfavorable subsets. Dose below 70 Gy may be acceptable for the most favorable subgroup.
The phase I/II experience from the Memorial Sloan Kettering Cancer Center (MSKCC), reported by Zelefsky et al., looked at both post-treatment biopsy and PSA failure in patients treated with dose-escalated EBRT [7]. In this study the radiation dose was systematically increased from 64.8 to 86.4 Gy by increments of 5.4 Gy in consecutive groups of patients. A positive biopsy at > 2.5 years after treatment was observed in only 1/15 (7%) of patients receiving 81.0 Gy, compared with 12/25 (48%) after 75.6 Gy, 19/42 (45%) after 70.2 Gy, and 13/23 (57%) after 64.8 Gy (p = 0.05). An update to this study evaluated clinical outcome according to risk group based on T-stage, pretreatment PSA and Gleason score [8]. Low-risk patients were considered those with PSA < 10 ng/mL, T-stage < T2b and Gleason score < 7. Those patients meeting all three criteria, two criteria or 0–1 criterion were considered favorable risk, intermediate risk and high risk, respectively. The 5-year actuarial PSA RFS rate for favorable risk disease receiving 64.8–70.2 Gy was 77% compared to 90% for those treated with 75.6–86.4 Gy (p = 0.05). The corresponding rates were 50% versus 70% in intermediate-risk cases (p = 0.001), and 21% versus 47% in unfavorable risk cases (p = 0.002).
The main limitation to dose escalation for prostate cancer has been the surrounding normal tissue tolerance, most importantly that of the rectum and bladder. Michalski et al. reported the toxicity outcome for 173 patients enrolled on RTOG 9406, a prospective phase I dose escalation study conducted to determine the maximally tolerated radiation dose in men treated with 3D-CRT for localized prostate cancer [9]. They found that despite a nearly 20% dose escalation (81.6 Gy vs 68.5Gy), compared to the historical RTOG trials, significantly fewer long-term bowel or bladder complications were noted. Storey et al. reported on the toxicity of the M.D. Anderson hospital experience and found that the group receiving 78 Gy had a significantly higher late grade 2 rectal toxicity than the group receiving 70 Gy [10]. However, if less than 25% of the rectum received 70 Gy or less, only 13% of patients experienced grade 2 rectal complications as compared to a 37% risk with a greater volume treated. They also reported that bladder complications were no different for the 70 Gy and 78 Gy arms.
Comment
Computed tomography-guided 3D-CRT and IMRT have enabled safe delivery of higher radiation doses to the prostate. For patients with low-risk disease, a minimum dose of 70 Gy is recommended (conditional recommendation Grade 2B). For intermediate- and high-risk disease, a dose of 75 Gy or greater appears to offer improved local control and disease specific survival (conditional recommendation Grade 2B).
Clinical question 29.2
Is IMRT better than 3D-CRT for treating localized prostate cancer?
Literature search
A literature searched was performed using PubMed and Medline. Search terms included combinations of the following: “prostate cancer,” “IMRT,” “three-dimensional conformal radiation therapy,” “dose escalation,” “randomized controlled trials.” No time frame limitations were applied.
The evidence
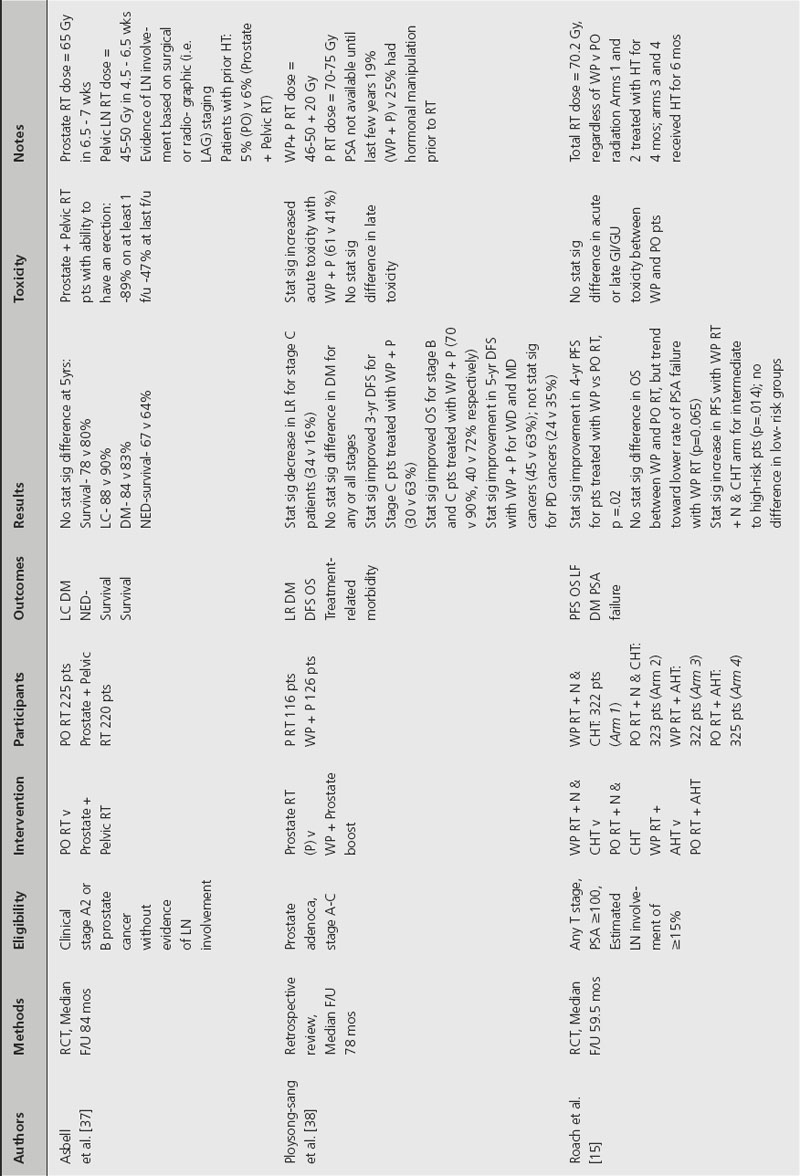
There are no randomized controlled trials that directly compare IMRT to 3D-CRT in localized prostate cancer. Instead, the shift in treatment modality to IMRT has stemmed from dose escalation studies and associated toxicity analyses; see Table 29.2.
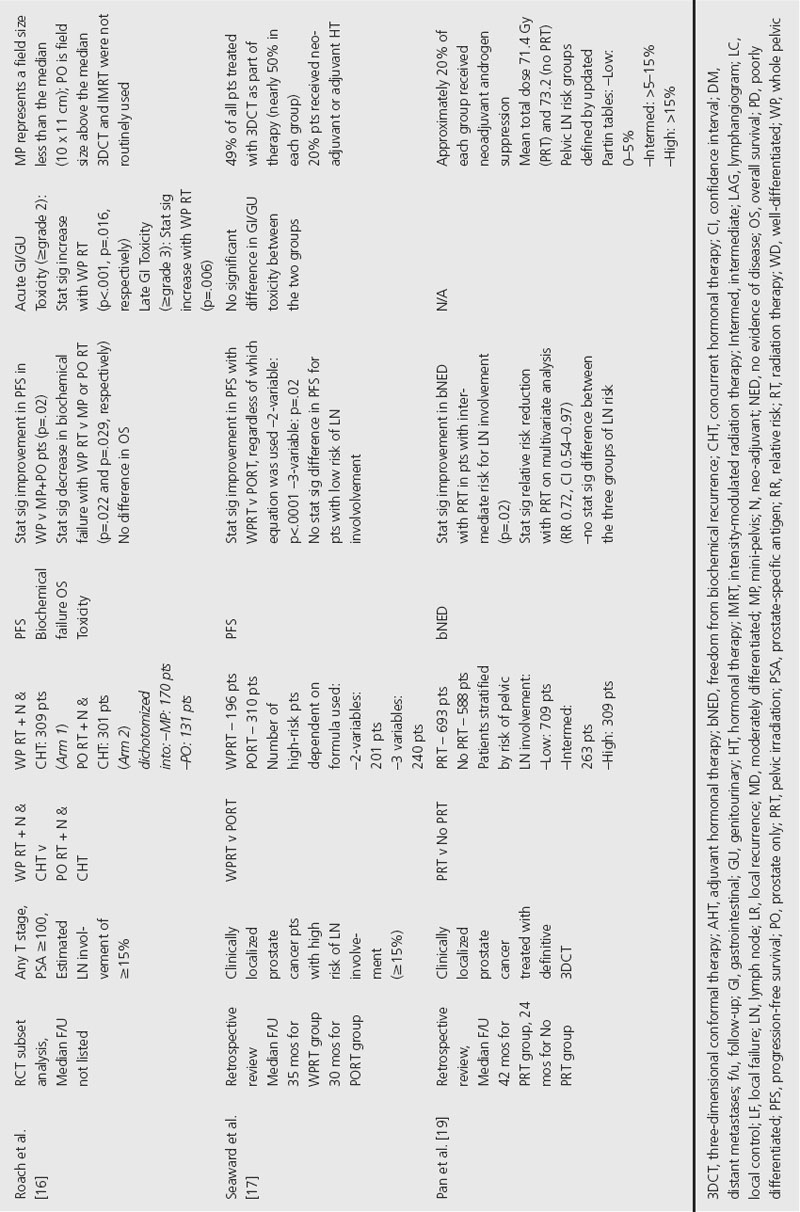
Table 29.2 Effect of pelvic irradiation for localized prostate cancer
The MSKCC has several large prospective phase I/II dose escalation studies that address this issue [7,8,11]. The first two publications demonstrated a statistically significant improvement in PSA RFS and local control with increased dose [7,8]. The most recent publication suggests that intermediate- and high-risk patients are the key patients to target with a higher dose [11].
Five RCTs comparing a standard dose arm to an escalated dose consistently demonstrate improved biochemical disease-free survival with the higher dose for locally advanced prostate cancer [1,2,4,12,13].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








