Pulmonary and Critical Care Medicine
Question 1
A 57-year-old man presents to his primary care physician with 3 months of persistent dry cough and unintentional weight loss of 25 lb. He has occasional night sweats. He has a 40 pack-year smoking history and quit 6 months ago. He has worked in a shipyard most of his adult life. His chest X-ray (CXR) shows a right hilar mass. He wishes to know more about the development of his condition. Which one of the following statements is true?
a) The most common histologic type of lung cancer is small cell carcinoma.
b) It is the most common cancer in the United States.
c) Eighty percent of lung cancer deaths among men are attributable to smoking.
d) Screening has proved beneficial in decreasing mortality from lung cancer among the general population.
View Answer
Answer and Discussion
The answer is c.
Objective: Identify important epidemiology regarding lung cancer.
According to the National Cancer Institute and American Cancer Society, lung cancer was the second most common cancer identified in both men and women, second only to prostate cancer and breast cancer, respectively. Lung cancer, however, remains the most common cause of cancer-related mortality in the United States, claiming over 160,000 deaths in 2012 alone. Less than 20% are small cell in type, whereas over 80% are non-small cell. According to the CDC, 80% of mortality among men and ~50% of mortality among women from lung cancer can be directly attributable to smoking. Despite advances in radiologic imaging with low-dose computed tomography (CT) and positron emission tomography (PET) scanning, screening has not yet proved beneficial in decreasing mortality from lung cancer.
Question 2
A 64-year-old woman presents to clinic with increasing fatigue, cough with scant sputum production, and ~15 lb weight loss over the last 2 months. She has a 45 pack-year smoking history and quit around the time her symptoms started. She also reports increased headache. On examination, she is mildly plethoric. She is comfortable at rest, but dyspneic with any exertion. Her lung examination is unrevealing. Her labwork is remarkable only for Na of 120. Which of the following statements about the management is true for her condition?
a) Surgery is the most important treatment modality.
b) Supraclavicular node involvement ipsilateral to the sentinel lesion qualifies as extensive stage disease.
c) Approximately 80% of patients respond to chemotherapy.
d) Prophylactic cranial irradiation has been shown to prolong survival.
View Answer
Answer and Discussion
The answer is c.
Objective: Identify the presentation and treatment of small-cell lung cancer (SCLC).
SCLC is considered a systemic disease, and thus surgery plays no part in the management of the disease. Multiple staging systems are used for SCLC, including the American Joint Cancer Commission (AJCC), the Veteran’s Administration Lung Study Group (VALG), and the International Association for the Study of Lung Cancer (IASLC). All of these classifications attempt to identify SCLC as either limited stage disease (those lesions that can be encompassed in a single radiation field) or extensive disease. Limited stage disease describes disease confined to one hemithorax that can be included in a reasonable thoracic radiation field. This includes extension to supraclavicular nodes on the same side as the sentinel lesion. Approximately 80% of patients respond to chemotherapy. Prophylactic cranial irradiation reduces the incidence of brain metastases, but has not been shown to prolong survival.
Question 3
A 54-year-old Caucasian man presents to the emergency department (ED) with 6 months of persistent dry cough and unintentional weight loss of 30 lb. He has a 30 pack-year smoking history and quit 6 months ago at the onset of his symptoms. He is found to have a parenchymal mass, which on biopsy shows squamous cell cancer. He wishes to know what his overall treatment and prognosis is. Which one of the following statements is true for non-small-cell lung cancer?
a) Stage IV disease is associated with 5-year survival rates of approximately 10%.
b) About 60% of patients are suitable for resection at diagnosis.
c) Stage IA disease is associated with 5-year survival rates of approximately 40%.
d) Surgery offers the best chance of cure.
View Answer
Answer and Discussion
The answer is d.
Objective: Identify appropriate therapeutic and prognostic information for non-small-cell lung cancers.
With currently available modalities in thoracic surgery, postoperative mortality rate is <5%. About 20% to 33% of patients are suitable for resection at the time of diagnosis, and lobectomy is the most commonly performed operation. Surgery offers the best chance of cure for non-small-cell lung Ca. Stages IA and IB diseases are associated with 5-year survival rates of 67% and 57%, respectively, whereas stages IIA, IIB, and IIIA have 5-year survival rates of 55%, 39%, and 26%, respectively. Advanced stages such as IIIB and IV have poor 5-year survival rates of 5% and 1%, respectively.
Question 4
You are called by the ED to see a 64-year-old male patient with a known history of chronic obstructive pulmonary disease (COPD; FEV1 of 25% of predicted) secondary to long standing tobacco use. He has been noticing a progressive decline in his functional status due to shortness of breath. He denies any acute change in sputum production, worsening wheezing, or fevers. He reports compliance with his medications, which includes inhaled steroids and long-acting β-agonists (LABAs), along with short-acting β-agonist and anti-cholinergic. He uses his combination β-agonist and anti-cholinergic about 4 to 6 times daily. You get an arterial blood gas (ABG), which shows a pH of 7.35, PCO2 of 88, and PO2 of 60 with an SaO2 of 85%. ABG done 2 weeks ago as an outpatient after recovery from an acute COPD exacerbation showed a pH of 7.38, PCO2 of 86, and PO2 of 73 and an SaO2 of 87%.
Which of the following is the most important variable to correct in this patient with very severe COPD?
a) PaCO2
b) pH
c) Hypoxemia
d) Pulmonary hypertension
e) Cardiac output
View Answer
Answer and Discussion
The answer is c.
Objective: Identify indications for supplemental oxygen therapy in COPD patients.
The overriding concern is to improve tissue oxygen delivery. Following are the current guidelines for long-term supplemental O2 therapy based on the gold criteria: PaO2 of 55 mmHg or less OR an SaO2 of less than 88% confirmed twice over a 3-week period. Alternatively, supplemental O2 is also indicated if one has a PaO2 between 55 and 60 mmHg OR an SaO2 of 88% if they have one of the following conditions: pulmonary hypertension, peripheral edema suggesting congestive heart failure, or hematocrit >55%. Although supplemental oxygen may contribute to hypercapnia (mostly by affecting ventilation-perfusion mismatching rather than the suppression of hypoxic drive), correcting hypoxemia is critical. The mechanism whereby chronic oxygen improves survival is probably by reducing pulmonary hypertension. The best way to reduce pulmonary artery pressures is to correct hypoxemia.
Question 5
Which of the following chest radiographic findings is inconsistent with the diagnosis of asbestosis?
a) Presence of pleural plaques
b) Presence of pleural effusion
c) Reticulonodular infiltrates
d) Upper lobe predominance
e) Reduced lung volumes
View Answer
Answer and Discussion
The answer is d.
Objective: Identify the different pulmonary findings of asbestosis.
Asbestos exposure represents a spectrum of histopathologic and radiographic findings that are typically broken up into three major categories: pleural disease, interstitial disease, and malignancies.
Pleural disease is often considered the hallmark of asbestos exposure, and upwards of 50% of patients will have some pleural involvement. Pleural disease manifests as either pleural plaques, pleural adhesions causing rounded atelectasis, or benign asbestos pleural effusions (BAPEs). Pleural plaques preferentially involve the parietal pleura adjacent to the ribs. They are considerably less extensive in the visceral pleura and the intercostal space and are almost never seen in the costophrenic angles or the apices. Rounded atelectasis is a non-specific finding and can be seen with just about any type of pleural inflammation. BAPEs are typically very small and unilateral and can be seen before the interstitial disease. Pleural fluid analysis can be varied: up to one-third have increased pleural eosinophils and can be as high as 50% of the total nucleated cell count.
The interstitial process typically involves the lower lung zones and can be seen as non-specific imaging findings of haziness on CXR and ground glass opacities on CT scan early in the disease. This eventually progresses to honeycombing. Lymphadenopathy, either hilar or mediastinal, is not associated with asbestosis.
Asbestos is classically linked to mesothelioma, and along with smoking is a major risk factor for this malignancy. However, asbestos exposure has also been linked to both small- and non-small-cell lung cancers.
Question 6
Which one of the following statements is incorrect?
a) Obtaining an occupational history is imperative before diagnosing a patient with sarcoidosis.
b) An elevated serum angiotensin-converting enzyme (ACE) level is not diagnostic.
c) Sarcoidosis can involve any organ system.
d) The presence of sarcoid granulomas in the pulmonary parenchyma is an indication for treatment.
e) The most common presentation is an asymptomatic chest radiograph abnormality.
View Answer
Answer and Discussion
The answer is d.
Objective: Identify indications for treatment in sarcoidosis.
Sarcoidosis is an inflammatory condition marked by noncaseating granulomas of affected tissue without evidence of another identifiable etiology. Given that infection, particularly mycobacterial and fungal infections are on the differential, a travel and occupational history is important. Occupational history is also important, as there have been association with certain occupational irritants, specifically insecticides and building materials. Clinical presentation can vary substantially and can involve any organ systems. The most common organs involved are the lymphatic system, lungs, skin, and eyes. Up to 90% of patients with sarcoidosis will have some involvement from these systems. The most common presentation is a chest radiograph showing hilar lymphadenopathy or reticulonodular infiltrates in an asymptomatic patient. Angiotensin-converting enzyme (ACE) is produced by granulomas, and elevated levels can be seen in up to 60% of patients. However, genetic polymorphisms can lead to variable levels in individuals, leading to a lack of both sensitivity and specificity in the diagnosis of sarcoidosis. Currently, the role of ACE levels is controversial at best. Making a histologic diagnosis of sarcoidosis is not considered sufficient reason to treat with steroids. Commonly accepted indications for treatment include significant symptoms or progressive loss of lung function. Involvement of critical extrapulmonary organs, such as cardiac or renal sarcoid, also may prompt treatment.
Question 7
A 53-year-old man presents to your clinic to establish care. Patient has no significant past history, although has not really followed with a physician. He reports a family history notable for hypertension in his parents, but is otherwise unremarkable. He has a 40 pack-year smoking history and has worked most of his life in demolition of old buildings. He has had multiple former coworkers diagnosed with asbestosis, and he wants to know his risk of developing this condition.
Which one of the following statements to this patient about asbestos-related lung disease is incorrect?
a) Benign asbestos pleural effusion is one of the earliest manifestations of asbestos exposure.
b) Pleural thickening in a patient with asbestos exposure indicates asbestosis.
c) Pleural plaques almost never result in symptoms or physiologic impairment.
d) Mesothelioma may develop in patients with brief, low-level exposure to asbestos.
e) Rounded atelectasis is a benign manifestation of asbestos exposure that can be mistaken for a malignancy.
View Answer
Answer and Discussion
The answer is b.
Objective: Define asbestosis and differentiate from isolated pleural disease.
This question is meant to emphasize the fact that the term asbestosis should be reserved for patients with evidence of pulmonary parenchymal scarring. Pleural disease does not merit the diagnosis of asbestosis. The clinical relevance of this distinction centers around two issues: increased symptoms in patients with asbestosis, as most pleural disease does not cause symptoms or impairment, as well as the increased risk of malignancy in patients with asbestosis versus asbestos associated with pleural disease. Patients with any asbestos exposure, even low level exposure without evidence of pleural or parenchymal disease are at increased risk for mesothelioma compared with the general population. Those patients with asbestos-associated pleural disease have a comparable risk of mesothelioma as those with asbestos exposure without pleural disease. However, asbestosis is associated with a higher risk of mesothelioma compared with those with pleural disease. This risk is further increased by concurrent smoking, and as such, all patients with asbestosis should be strongly discouraged against smoking. BAPEs are typically very small and unilateral and can be seen before the interstitial disease. Patients with evidence of pleural disease can develop rounded atelectasis, which can appear mass like on imaging and is often mistaken for malignancy.
Question 8
Which one of the following statements is incorrect?
a) Silicosis shows a predominantly lower zone distribution on the chest radiograph.
b) Progressive massive fibrosis is a complication of silicosis.
c) There is an increased incidence of tuberculosis (TB) in patients with silicosis.
d) There is an increased incidence of rheumatoid arthritis and scleroderma in patients with silicosis.
View Answer
Answer and Discussion
The answer is a.
Objective: Identify clinical features and other conditions associated with silicosis.
Silicosis represents pulmonary manifestations after exposure to silica. Silica exposure is often seen in mining, glass manufacturing, sand blasting, and road and building construction. Silicosis manifests clinically along a spectrum of
simple chronic silicosis (most common), accelerated silicosis and acute silicosis, based on the chronicity of symptom development compared to exposure to silica. They all lead to increased inflammation in the pulmonary parenchyma and intrathoracic lymph nodes, predominantly in the upper lobes. Silicosis is associated with the following complications: progressive massive fibrosis, lung cancer, and respiratory failure. Silicosis is also associated with an increased risk of TB, and therefore, patients should get regular Tb testing. Silicosis has also been associated with higher incidence of autoimmune conditions such as rheumatoid arthritis, scleroderma, and systemic lupus erythematosus.
simple chronic silicosis (most common), accelerated silicosis and acute silicosis, based on the chronicity of symptom development compared to exposure to silica. They all lead to increased inflammation in the pulmonary parenchyma and intrathoracic lymph nodes, predominantly in the upper lobes. Silicosis is associated with the following complications: progressive massive fibrosis, lung cancer, and respiratory failure. Silicosis is also associated with an increased risk of TB, and therefore, patients should get regular Tb testing. Silicosis has also been associated with higher incidence of autoimmune conditions such as rheumatoid arthritis, scleroderma, and systemic lupus erythematosus.
Question 9
Which one of the following statements is correct?
a) Interstitial lung disease (ILD) is more common in women with rheumatoid arthritis than in men with rheumatoid arthritis.
b) Five percent of patients presenting with acute lupus pneumonitis have had no history of lupus.
c) There is poor correlation between the severity of the cutaneous and pulmonary manifestations of scleroderma.
d) Jo-1 antibody is not associated with the presence of ILD in patients with polymyositis.
e) ILD associated with Sjögren syndrome often involves neutrophilic infiltration.
View Answer
Answer and Discussion
The answer is c.
Objective: Identify features of ILD associated with connective tissue disease.
Pulmonary involvement is a major cause of mortality in connective tissue disease. Pulmonary involvement is most commonly ILD but can also involve pulmonary hypertension, pulmonary thromboembolic disease, and pulmonary nodules. As with many of the connective tissue disease-associated ILDs, there is no real correlation between the severity of the ILD and the extrapulmonary manifestations. It is generally more common in men with rheumatoid arthritis versus women with rheumatoid arthritis. To further underscore the disconnect between pulmonary and extrapulmonary manifestations of connective tissue disease, lupus pneumonitis can be seen in up to 50% of patients without any previous history of lupus. Jo-1 is associated with dermatomyositis/polymyositis and has a stronger association with ILD. ILD associated with Sjögren syndrome is associated with a lymphocytic infiltrate, not neutrophilic infiltration.
Question 10
A 70-year-old man with a history of insulin-dependent diabetes mellitus, alcohol abuse, severe gastroesophageal reflux disease, emphysema, and benign prostatic hyperplasia requiring an indwelling catheter and frequent courses of intravenous antibiotics presents with high-grade fever; congestion; cough productive of thick, yellow, blood-tinged sputum; and right pleuritic chest pain.
On examination, you are presented with an ill-looking man febrile to 39°C. He has a heart rate (HR) of 110 beats/minute with a blood pressure (BP) of 110/54 mmHg. He has a respiratory rate of 24 breaths/minute. He is able to speak in complete sentences and does not appear to be using accessory muscles. Pulmonary examination reveals a right upper lung consolidation and right base dullness. His chest radiograph shows right upper lobe alveolar infiltrate with cavity and moderate right effusion. Laboratory findings show leukocytosis with left shift. His ABG analysis shows pH, 7.32; PCO2, 52; and arterial oxygenation, 80 on 3-L forced inspiratory oxygen.
His pleural fluid is thick, yellow, and purulent. Laboratory findings are pH, 7.82; glucose, 30 mg/dL; and lactate dehydrogenase, 1,050 IU/dL.
Along with IV fluids and broad-spectrum antibiotics, what would be the most appropriate immediate action?
a) Urine culture and sensitivity; replace Foley
b) Intubation and mechanical ventilation
c) Thoracic surgery consult for open thoracostomy
d) Tube thoracostomy
e) Stop antacid, order esophagogastroduodenoscopy
View Answer
Answer and Discussion
The answer is d.
Objective: Identify and manage a gram-negative empyema.
This question identifies a patient with diabetes and alcohol abuse who is at risk for complicated infections, and presenting with sepsis. The management of this patient must be prioritized based on the acuity of the patient. The patient is ill appearing, but is not in acute respiratory distress or in shock. He does not have any indications for urgent intubation and mechanical ventilation. Once emergent issues are addressed, source identification and control is paramount. Patient clearly has a respiratory focus for this infection evidenced by the symptoms of fever, productive cough, and pleuritic chest pain. This is further confirmed by infiltrates on imaging. However, he also has an effusion with pleural fluid analysis suggestive of a urea splitting organism leading to increased ammonia production and increased pH. Some gram-negative bacilli, specifically Proteus is associated with empyema with elevated pH. The mainstay of therapy for an empyema is drainage with tube thoracostomy. If this fails, then open thoracostomy is warranted. Given the overwhelming evidence of a pulmonary infection, management of this should not be delayed looking for other sources. With a chronic indwelling Foley catheter, he is at higher risk for colonization, and a urine culture without urinalysis is of limited utility. Also, EGD would not be warranted in this patient.
Question 11
A 60-year-old white man presents with bilateral, vague, nonpleuritic chest pain, and mild shortness of breath; no fever,
cough, or night sweats. On history taking, 15 months ago, this patient had right effusion that resolved spontaneously; 5 years ago, he had occasional bilateral wrist pain, treated with aspirin. An annual purified protein derivative test was negative 3 months ago. On examination, you find bibasilar dullness and a hard nodule on the nose. His chest radiograph shows bilateral moderate pleural effusion.
cough, or night sweats. On history taking, 15 months ago, this patient had right effusion that resolved spontaneously; 5 years ago, he had occasional bilateral wrist pain, treated with aspirin. An annual purified protein derivative test was negative 3 months ago. On examination, you find bibasilar dullness and a hard nodule on the nose. His chest radiograph shows bilateral moderate pleural effusion.
The pleural fluid analysis reveals a white blood cell (WBC) count of 2,000/mm3; polymorphonuclear leukocytes, 90%; pH, 7.05; lactate dehydrogenase, 1,000 IU/dL; protein, 4 g/dL; and glucose, 5 mg/dL.
Based on the most likely diagnosis, what would be the most appropriate action?
a) Isoniazid, 300 mg; rifampin, 600 mg; ethambutol, 900 mg daily
b) Prednisone, 40 mg daily
c) Bilateral chest tube placement
d) Intravenous ceftazidime and gentamicin
e) Close observation for spontaneous resolution of fluid
View Answer
Answer and Discussion
The answer is b.
Objective: Identify and manage a rheumatoid effusion.
Pulmonary complications are a major cause of mortality of rheumatoid arthritis, however, pleural effusions is an uncommon manifestation. Pleural effusions associated with rheumatoid arthritis are more common in men (as are most pulmonary manifestations). Pleural fluid analysis classically shows a low pH, high LDH, low protein, and low glucose. The fluid is predominantly composed of PMNs, and pleural biopsy may show rheumatoid nodules. These last two findings are more specific findings, and the absence of these should not exclude rheumatoid effusion from the differential. This may be difficult to differentiate from empyema and parapneumonic effusion based on fluid analysis alone. However, in this patient, he had a previous pleural effusion and is non-toxic in appearance. He also has a history of articular symptoms, pointing toward underlying RA. He also had a negative PPD 3 months previously, making TB an unlikely etiology for the pleural effusion.
The mainstay of therapy for rheumatoid arthritis is immunosuppression, especially corticosteroids acutely. Corticosteroids have also been shown to be effective for rheumatoid effusions. There is no role for drainage of a rheumatoid effusion.
Question 12
A 30-year-old woman presents with slowly progressing shortness of breath of 6 months’ duration. Her past medical history includes pneumothoraces, one on either side, 4 weeks apart 1 year ago. She denies any previous surgical history.
On examination, she has increased dullness in the left base, right basilar crackles, and small ascites. Her chest radiograph shows hyperinflated lungs, vague interstitial changes, and left effusion. A pleural tap reveals milky white fluid, with triglycerides, 245 mg/dL and a cholesterol level of 14 mg/dL.
The most likely diagnosis is which of the following?
a) Lymphoma
b) Catamenial pneumothorax
c) Gorham syndrome
d) Lymphangioleiomyomatosis (LAM)
e) Histiocytosis X
View Answer
Answer and Discussion
The answer is d.
Objective: Identify a chylothorax associated with LAM.
The identification of a young woman with a history of spontaneous pneumothorices and interstitial markings on CXR as concerning for LAM is the first step in answering this question. This is further confirmed by evidence of a chylothorax with high triglycerides and low cholesterol levels confirms this finding. Chylothoraces is associated with disruption of the thoracic duct or its tributaries and is classified as either a traumatic cause versus non-traumatic causes. The most common non-traumatic causes in younger patients are lymphoma and LAM. Lymphoma is not typically associated with interstitial markings on CXR and would not explain the pneumothoraces 1 year prior.
Question 13
A 63-year-old man in a wheelchair presents with crippling rheumatoid arthritis. His annual chest radiograph revealed moderate bilateral effusion. No chest pain, cough, or shortness of breath is present.
You review his old radiographs and observe bilateral subpulmonic effusions for 5 years. His purified protein derivative test is negative. His pleural fluid is milky white and shiny; the analysis reveals a WBC count of 2,000/mm3, 90% L; glucose, 16 mg/dL; lactate dehydrogenase, 1,200 IU/dL; triglycerides, 30 mg/dL; cholesterol, 150 mg/dL; and a large amount of cholesterol crystals.
What would be the most appropriate action?
a) Start medium-chain triglyceride diet
b) Lymphangiography
c) Serology for Wuchereria bancrofti infestation
d) Bilateral pleuroperitoneal pump
e) Conservative treatment
View Answer
Answer and Discussion
The answer is e.
Objective: Identify and manage a cholesterol effusion (a.k.a. pseudochylothorax or chyliform effusion).
This is a cholesterol, also known as pseudochylothorax or chyliform effusion, as evidence by low triglycerides and elevated cholesterol in the pleural fluid. The presence of cholesterol crystals is also consistent with a cholesterol effusion. The rest of the pleural fluid is consistent with a rheumatoid effusion and high LDH and low glucose. This is also consistent
with the patient’s history of preexisting rheumatoid arthritis. Cholesterol effusion is associated with chronic inflammation or infection of the pleura, most commonly rheumatoid effusions and tuberculosis. The treatment for a cholesterol effusion is treatment of the underlying condition and conservative management. Medium-chain triglyceride diet is the appropriate diet for a chylothorax, not for a pseudochylothorax. Chylothorax is evidenced by fluid analysis high in triglycerides, and low in cholesterol, which is inconsistent with this patient. Chylothorax is caused by obstruction or damage to the lymphatic system. Lymphangiography would potentially be indicated for a chylothorax. Wuchereria bancrofti is a parasitic infection associated with lymphatic obstruction. It is responsible for up to 90% of lymphatic filariasis. This would present as a chylous effusion as well. Bilateral pleuroperitoneal shunt is a treatment for persistent chylothorax.
with the patient’s history of preexisting rheumatoid arthritis. Cholesterol effusion is associated with chronic inflammation or infection of the pleura, most commonly rheumatoid effusions and tuberculosis. The treatment for a cholesterol effusion is treatment of the underlying condition and conservative management. Medium-chain triglyceride diet is the appropriate diet for a chylothorax, not for a pseudochylothorax. Chylothorax is evidenced by fluid analysis high in triglycerides, and low in cholesterol, which is inconsistent with this patient. Chylothorax is caused by obstruction or damage to the lymphatic system. Lymphangiography would potentially be indicated for a chylothorax. Wuchereria bancrofti is a parasitic infection associated with lymphatic obstruction. It is responsible for up to 90% of lymphatic filariasis. This would present as a chylous effusion as well. Bilateral pleuroperitoneal shunt is a treatment for persistent chylothorax.
Question 14
A 70-year-old man with a history of congestive heart failure, on optimal medication, underwent thoracentesis in the ED for large right effusion using a 16-gauge spinal needle (3.5 L of serosanguineous fluid was removed uneventfully). Minutes after the procedure, the patient developed progressive shortness of breath and needed 100% fractional inspired oxygen.
On examination, you observe tachypnea, right lung wheeze, and basilar rales; BP is 100/70 mmHg, and pulse is 100 beats/minute.
What would be the most appropriate statement regarding the event?
a) Place large-bore chest tube for tension pneumothorax
b) Transfuse 2 U of pack cells for hemothorax
c) Administer Lasix, 60 mg intravenously
d) Intrapleural pressure monitoring could have avoided the event
e) Check creatine phosphokinase and ventilation/perfusion lung scan
View Answer
Answer and Discussion
The answer is d.
Objective: Identify complications from a thoracentesis.
A thoracentesis is a relatively safe procedure. The major complications are pneumothorax, hemothorax, hemorrhage, and re-expansion pulmonary edema. This patient developed reexpansion pulmonary edema, presumed secondary to rapid change in intrathoracic pressure leading to microvascular injury. The patient develops pulmonary edema following drainage of a large volume of a chronic pleural effusion. Intrapleural pressure monitoring could be used to minimize the risk of this occurring. The physical examination findings are not consistent with hemothorax or pneumothorax.
Question 15
A 35-year-old man who smoked one pack per day for 20 years was diagnosed with AIDS 4 years ago. He is allergic to sulfa and receives aerosolized pentamidine for Pneumocystis jiroveci pneumonia prophylaxis. He was doing well until a few days before admission, when he started developing progressive shortness of breath. His respiratory status deteriorated quickly, requiring intubation and mechanical ventilation. The next day, the respiratory therapist called because the patient had developed high airway pressures. This was also associated with a drop in the patient’s BP and arterial oxygen saturation. When you examine the patient, you notice decreased air entry on the left side with a deviation of the trachea to the right.
What should you do next?
a) Order chest radiography
b) Add 10 cm H2O of positive end-expiratory pressure
c) Insert a chest tube in the right lung
d) Insert a large-bore needle in the second intercostal space on the left
e) Place the patient on his side with the left side down
View Answer
Answer and Discussion
The answer is d.
Objective: Identify and manage a tension pneumothorax.
The patient has signs of a left-sided tension pneumothorax on the left as evidenced by a rapid deterioration of respiratory and hemodynamic status, decreased air entry on the left and tracheal deviation to the right. Tension pneumothorax is a clinical diagnosis and does not require radiographic confirmation prior to intervention. Urgent decompression of the pneumothorax is essential and is achieved by needle thoracostomy in the second intercostal space on the side of the pneumothorax. No other intervention will correct the hemodynamic compromise and may actually worsen it.
Question 16
A 44-year-old man with type I diabetes, end-stage renal disease, and diabetic retinopathy develops chest pain and low-grade fever (38.5°C) 5 days after a unilateral below-knee amputation done for a poorly healing ulcer. He had been recovering in a nursing facility but has missed two dialysis sessions due to low BP and has refused prophylactic subcutaneous heparin. After a 500-mL bolus of saline in the ED, he is transferred to the intensive care unit for further management. On examination, he is distressed, with a HR 96 beats/minute, respiratory rate 28 breaths/minute, oxygen saturation on room air is 86%, and BP 82/50 mmHg. The examination is difficult due to his obesity, but does not reveal an obvious cause for his hypotension; the surgical site looks clean and intact, and an indwelling tunneled catheter in his right neck also looks unremarkable. A 12-lead ECG shows nonspecific ST- and T-wave abnormalities but no definite signs of ischemia. A central venous catheter is inserted to guide decision-making. Measurement of the a-wave reveals a central venous pressure (CVP) of 19 mmHg; the tracing shows preserved waveforms except for loss of the y descent. Considering the findings of the central venous catheter,
which choice most effectively addresses the likely cause of shock in this patient?
which choice most effectively addresses the likely cause of shock in this patient?
a) Start broad-spectrum antibiotics; remove the tunneled catheter; and start fluids, pressor agents, and other modalities for likely septic shock using a “goal-directed therapy” approach
b) Consult cardiology service for a pericardiocentesis
c) Resuscitate more aggressively with crystalloids and consider thrombolytic therapy versus surgical consult for likely massive pulmonary embolus
d) Urgent coronary angiogram with percutaneous coronary intervention and placement of intra-aortic balloon pump, if needed, in preparation for mitral valve repair
e) Start dobutamine and prostacyclin for right ventricular failure
View Answer
Answer and Discussion
The answer is b.
Objective: Identify and manage cardiac tamponade as a cause of shock.
Pericardiocentesis with drainage of effusion leads to cardiac tamponade. Recognition of the right-sided waveforms and their derangements in disease is useful when prioritizing diagnostic tests, when decisions must be made urgently, or when there are conflicting data. It is important to be familiar with expected values for filling pressure (typically 4 to 8 mmHg for CVP). The differential diagnosis for elevated CVP in the setting of shock includes acute right heart failure (massive pulmonary embolism, right ventricular infarction), pericardial disease, and acute left heart disease (large myocardial infarction, acute mitral regurgitation, acute ventricular septal defect). The finding of an attenuated y descent is characteristic of cardiac tamponade because there is equalization of pressures between the atria and ventricles, which impairs atrial emptying. In uremic pericarditis, the expected tachycardia may be absent due to autonomic insufficiency; likewise, the ECG may not reveal diffuse ST segment elevations. In the early stages of septic shock, there is usually hypovolemia, so the CVP should be low. Massive pulmonary embolism and acute mitral valve rupture may cause hypotension but should not preferentially affect the y descent.
Question 17
An 18-year-old, 58-kg female asthmatic patient is intubated in the ED for respiratory failure from status asthmaticus. Her initial ventilator settings are assist-control mode with a set rate of 18, tidal volume 500 mL, FiO2 1.0, and positive end-expiratory pressure 5 cm H2O. On arrival to the intensive care unit, she is in shock, with systolic BP of 74 mmHg. Examination reveals an extremely agitated woman with diaphoresis, distended neck veins, and respiratory rate of 36 breaths/minute and SpO2 of 88%. Her breath sounds are markedly diminished but equal bilaterally. In addition to aggressive volume resuscitation and ensuring adequate sedation, you should institute which of the following to reverse her hypotension prior to cardiac arrest:
|
a) Reduce her set rate to 10 breaths/minute.
b) Administer 6 mg of pancuronium IV push
c) Insert a 16-gauge angiocatheter needle into the second intercostal space bilaterally.
d) Increase the inspiratory flow rate
e) Administer paralytics, and then remove her from the ventilator for 30 to 60 seconds
View Answer
Answer and Discussion
The answer is e.
Objective: Recognize common complications of mechanical ventilation.
It is important to recognize common complications of mechanical ventilation in patients with severe airways obstruction. Development of intrinsic positive end-expiratory pressure (PEEP; auto-PEEP, dynamic hyperinflation) is one of the most significant complications. Intrinsic PEEP can result in patient-ventilator dyssynchrony, agitation, difficulty weaning, ventilation/perfusion mismatch, barotrauma, and impairment of right-sided venous return leading to cardiovascular collapse. An important consideration is tension pneumothorax, but typically the patient will exhibit physical examination signs such as tracheal deviation, unilateral decrease of breath sounds, and hyperresonance on percussion. Prevention of intrinsic PEEP is achieved by maximizing alveolar emptying, either by decreasing airways resistance (bronchodilators) or by increasing expiratory time. Techniques to increase expiratory time include ensuring a low respiratory rate using sedatives and, if necessary, paralytics, decreasing the inspiratory time by adjusting the flow rate or the I:E ratio, and setting the mandatory rate on the ventilator as low as possible. Hypercapnia is acceptable to achieve this goal. However, none of these techniques is generally rapid enough to be helpful when hypotension is already established. Temporarily disconnecting the endotracheal tube from the ventilator circuit, and therefore the effects of positive-pressure ventilation, is the quickest way to effectively restore BP.
Question 18
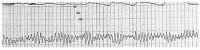
The female patient has been stable for 3 days. She is being treated with clarithromycin, ceftriaxone, Solu-Medrol, bronchodilators, and lorazepam. She became agitated overnight and was given haloperidol. Suddenly, she became hypotensive, and her pulse was not palpable. The ECG tracing is shown (ventricular tachycardia).
The patient is still hypotensive, her WBC count is 15,000/mm3, and her hemoglobin is 10 g/dL. You will do all of the following, except
a) Perform cardioversion-defibrillation
b) Administer magnesium intravenously
c) Temporarily disconnect the patient from the ventilator circuit
d) Correct hypocalcemia, hypokalemia, and alkalosis
View Answer
Answer and Discussion
The answer is c.
Objective: Identify important drug-drug interactions in critical care medicine.
This question highlights an important topic in critical care medicine-drug interactions. An important effect of drug interaction in the critically ill patient is hypotension caused by partial adrenal insufficiency. This drug interaction occurs in patients receiving drugs that can increase the activity of the P450 system (e.g., phenytoin, phenobarbital). When the P450 system is activated, the metabolism of steroids increases, creating a state of partial adrenal insufficiency. This drug interaction should be suspected in patients receiving medication that can increase the metabolism of the P450 system and who present with persistent hypotension in the absence of other etiologies. An increasingly recognized offender is etomidate, a medication commonly used in rapid-sequence intubation, which blocks adrenal steroid production directly.
Macrolides and haloperidol, drugs commonly used in the intensive care unit, are known to increase the QT interval. Patients with underlying ischemic heart disease and electrolyte and acid-base abnormalities are more likely to develop this complication. Phenothiazines, antiarrhythmic medications, tricyclic antidepressants, and antipsychotic agents and cisapride can prolong the QT interval as well.
Question 19
A 34-year-old homeless man is evaluated in the ED, where he was brought after being found obtunded. His medical history is remarkable for HIV and polysubstance abuse. Examination reveals an obtunded man with no focal neurologic signs. He is afebrile, with HR of 104 beats/minute, respiratory rate 22 breaths/minute, and BP 96/68 mmHg. His sodium is 148 mmol/L, potassium 4.0 mmol/L, chloride 115 mmol/L, bicarbonate 10 mmol/L, blood urea nitrogen 47 mg/dL, creatinine 1.3 mg/dL, and glucose 58 mg/dL. Serum albumin is 2.5 g/dL. ABG on room air reveals a pH of 7.12, PCO2 28 mmHg, and PaO2 94 mmHg. His serum lactate is 2.2 mmol/L. Which of the following is true in your evaluation of this patient?
a) He has an anion gap (AG) metabolic acidosis with appropriate respiratory compensation.
b) He has an AG metabolic acidosis and inappropriate respiratory compensation.
c) He has an AG metabolic acidosis, a metabolic alkalosis, and inappropriate respiratory compensation.
d) He has an AG metabolic acidosis, a non-AG metabolic acidosis, and inappropriate respiratory compensation.
e) He has an AG metabolic acidosis, a non-AG metabolic acidosis, and appropriate respiratory compensation.
View Answer
Answer and Discussion
The answer is b.
Objective: Identify acid-base disorders.
Interpretation of ABG abnormalities is a key skill in critical care medicine. Systematic evaluation of the ABG results often leads to unsuspected findings, such as triple acid-base disorders or respiratory insufficiency. In this case, use of “Winter formula” allows assessment of the adequacy of the respiratory response to the primary acidosis:
Expected, PCO2 = ([1.5 × measured HCO3] + 8) ± 2
To evaluate for the presence of two metabolic processes, one must compare the change in AG versus the change in bicarbonate. In the setting of hypoalbuminemia, the expected AG should be reduced by about 2.5 mEq/L for every 1 g/dL decrease in serum albumin, with normal AG in most laboratories ranging from 6 to 12 mEq/L.
Using 12 mEq/L as the AG normal value, in the previous example, the expected AG should be [12 mEq/L – (2.5 × 1.6 g/dL decrease of albumin)] = 8 mEq/L. However, the calculated gap is 23 mEq/L. Thus, the AG has increased by 15 mEq/L over the expected value. Has there been an equivalent (equimolar) change in the bicarbonate level? In this case, the bicarbonate has decreased from 24 mEq/L (normal) to 10 mEq/L = 14 mEq/L. Therefore, all the change in bicarbonate level can be explained by the unmeasured anions. If the change in bicarbonate were more severe than that predicted by the change in AG, a superimposed nongapped acidosis would be suspected; if less profound, then a concomitant metabolic alkalosis should be considered.
Question 20
The male patient in question 19 is diagnosed with ethylene glycol intoxication, after it is noted that there is an osmolar gap present, and treated with ethanol infusion to competitively prevent metabolism of ethylene glycol to formaldehyde and formic acid. He avoids renal failure; however, on the second day in the intensive care unit, he develops a fever (39.5°C) and hypoxemia. Chest imaging shows bilateral diffuse infiltrates. His hemoglobin is stable at 8.7 g/dL. Over the ensuing 24 hours, he develops refractory hypoxemic respiratory failure, requiring intubation. The most appropriate next step now includes
a) Start ceftriaxone and azithromycin
b) Start piperacillin-tazobactam, tobramycin, and vancomycin
c) Start piperacillin-tazobactam, azithromycin, and vancomycin
d) Start piperacillin-tazobactam and ciprofloxacin
e) Perform bronchoalveolar lavage to look for infection with P. jiroveci.
View Answer
Answer and Discussion
The answer is c.
Objective: Identify complication of pneumonia among hospitalized, critically ill patients.
The correct answer depends on recognizing that the likely diagnoses are community-acquired pneumonia or aspiration pneumonitis with acute respiratory distress syndrome (ARDS). The development of pneumonia after 48 hours in the hospital, or within 3 months of a prior hospitalization, classifies as hospital-acquired pneumonia, mandating consideration of antipseudomonal antibiotics as part of the initial therapy. However, in community-acquired pneumonias, there are mitigating factors that may provide indications for more extensive antimicrobial coverage. In patients admitted to the intensive care unit, there is a high likelihood that resistant organisms will be present, including drug-resistant pneumococcus, Legionella species, and community-acquired methicillin-resistant Staphylococcus aureus (MRSA). Therefore, patients with severe community-acquired pneumonia should be treated with a combination of a potent antipneumococcal cephalosporin and either an advanced macrolide or quinolone. In patients with risk factors for Pseudomonas aeruginosa, including immunosuppression, significant structural lung disease [cystic fibrosis (CF), bronchiectasis, or repeated exacerbations of COPD that require frequent glucocorticoid and/or antibiotic use], probable aspiration, or multiple medical comorbidities, an antipseudomonal penicillin should be used. The use of vancomycin in severe community acquired pneumonia is hotly debated, but should generally be reserved for individuals with gram-positive organisms on sputum examination or risk factors for community-acquired MRSA (recent influenza-like illness, prior antibiotic therapy, end-stage renal disease, or injection drug abuse).
Although this individual may have AIDS, the onset of Pneumocystis pneumonia (PCP) is usually subacute. Although the sensitivity of bronchoalveolar lavage for diagnosing PCP is excellent in HIV (97% to 99%), it is less sensitive in the non-HIV population.
Question 21
A 48-year-old man presents with his wife, who complains of her husband’s snoring. Further history reveals snoring for at least 20 years, with restless sleep observed by the wife. The patient denies any problem sleeping, but on direct questioning, he admits to dry mouth and headaches in the morning and sleepiness throughout the day. He confesses that he almost fell asleep at the wheel of the car several times, but he ascribes this to long hours and overwork. Physical examination reveals a stocky man, somewhat overweight, but the examination is otherwise normal. Which would be the most appropriate next step?
a) Sedative medication for the patient to ensure that he gets a better night’s sleep
b) Sedative medication for the wife so that she can sleep through his snoring
c) Sending the patient for sleep studies
d) Advising a weight loss program and following up in 6 months
e) Advising stopping smoking because doing so has been proven to stop snoring in more than 50% of patients
View Answer
Answer and Discussion
The answer is c.
Objective: Understand the diagnostic evaluation of excessive daytime sleepiness.
This man’s clinical picture suggests obstructive sleep apnea. Patients with unexplained excessive daytime sleepiness deserve further evaluation, and the diagnosis of obstructive sleep apnea requires examining a patient during sleep with a polysomnogram.
Question 22
A 21-year-old male patient comes to the emergency room with itching and jaundice. He has a long history of recurrent pulmonary infections, chronic sinusitis, a recent diagnosis of diabetes, and two prior admissions for pancreatitis. Liver biopsy confirms cirrhosis. In regard to this patient’s diagnosis, which of the following is the most accurate statement?
a) The disease is autosomal dominant in inheritance.
b) Alcohol abuse is a common cause for this disease.
c) The most common cause of death is liver failure.
d) A sweat chloride test result of <70 mEq/L is highly sensitive for diagnosis.
e) Digital clubbing is often seen in patients.
View Answer
Answer and Discussion
The answer is e.
Objective: Understand the clinical presentation of CF.
CF is a fatal autosomal recessive, multisystem disease that usually presents with persistent pulmonary infection, pancreatic insufficiency, and sinusitis. Additional features include pancreatitis, infertility, diabetes, deep vein thrombosis (DVT), and, rarely, biliary cirrhosis. Although CF is generally diagnosed in infants and children, patients may present later in life with atypical symptoms. One large retrospective cohort study of 1,051 patients with CF found that 7% received a diagnosis at age 18 years or older. Progressive lung disease and eventual respiratory failure continue to be the major causes of morbidity and mortality. The sweat chloride test is the gold standard for CF diagnosis, and a result of >70 mEq/L distinguishes CF from other lung diseases. More than 95% of men with CF are infertile, mostly due to incomplete development of the Wolffian structures, particularly the vas deferens. Digital clubbing is often seen in patients with moderate to severe disease.
Question 23
You are seated in the hospital cafeteria in the middle of a busy call day when the medical student with whom you are
having dinner complains of pruritus and appears flushed. He states that he has felt like this previously, is allergic to peanuts, and thinks that there may have been nuts in the cake that he just ate. He states that he does not feel too bad and that this is nothing like the last time, when he had some difficulty with breathing; he says that he will go lie down in the call room for awhile and he should be fine. You assess his airway and breathing, and they are normal. What would be the most appropriate next step?
having dinner complains of pruritus and appears flushed. He states that he has felt like this previously, is allergic to peanuts, and thinks that there may have been nuts in the cake that he just ate. He states that he does not feel too bad and that this is nothing like the last time, when he had some difficulty with breathing; he says that he will go lie down in the call room for awhile and he should be fine. You assess his airway and breathing, and they are normal. What would be the most appropriate next step?
a) Let him go and rest; you will go and see a patient who has just arrived and then check on the medical student in an hour or so
b) Keep him with you so that you can take him to the ED if he starts to feel any worse or has any pulmonary symptoms
c) Take him to the ED, and administer 1 mL of 1:10,000 epinephrine intravenously with cardiac monitoring
d) Take him to the ED, recruit assistance from the medical team there, have his airway and cardiopulmonary status assessed and monitored, obtain intravenous access, and administer 0.5 mL of 1:1,000 epinephrine subcutaneously or intramuscularly as soon as possible
e) Give him an antihistamine that you happen to have in your pocket, and keep him with you so that you can take him to the ED if he starts to feel any worse or has any pulmonary symptoms
View Answer
Answer and Discussion
The answer is d.
Objective: Understand the clinical presentation and treatment of anaphylaxis.
Anaphylaxis can occur within 5 to 60 minutes after exposure to an allergen. This medical student is at risk for anaphylaxis and death. He needs a controlled and monitored environment. Epinephrine is the drug of choice; fatality rates are highest in patients in whom epinephrine administration is delayed. Severe airway edema, severe bronchospasm, or hypotension requires intravenous administration of 0.5 to 1.0 mL of epinephrine. Mild or moderate symptoms without laryngeal edema, bronchospasm, or hypotension should be treated with 0.3 to 0.5 mL of 1:1,000 epinephrine subcutaneously or intramuscularly.
Question 24
A solitary pulmonary nodule is seen in the right upper lobe on the chest radiograph and CT scan of a 60-year-old woman with a history of stage IB breast cancer. She underwent right lumpectomy 20 years ago without any further treatment. Regularly scheduled follow-up mammograms have been negative to date. She has a 20 pack-year history of tobacco use and quit smoking 7 years ago. The chest CT scan shows a 1.2-cm mass with smooth borders, popcorn calcification, and a density of 214 Hounsfield units. What is the next step in management?
a) Follow up with serial CTs to evaluate change in size of the nodule
b) Excise the mass for pathologic diagnosis
c) Obtain a fluoro-2-deoxyglucose-PET scan
d) Perform percutaneous needle aspiration and biopsy
e) Order an MRI of the chest
View Answer
Answer and Discussion
The answer is a.
Objective: Understand the diagnostic evaluation of a solitary pulmonary nodule.
A solitary pulmonary nodule is a lesion that is usually <3 cm and surrounded by pulmonary parenchyma. Larger lesions are more likely to be malignant than smaller lesions. Malignant lesions tend to have more irregular and spiculated borders as compared to the smooth and discrete border of benign lesions. Increased density on CT argues against malignancy with the cutoff of >164 Hounsfield units for benign and <164 Hounsfield units for malignant lesions. Certain patterns of calcification such as “popcorn” calcification, laminated (concentric) calcification, central calcification, and diffuse homogeneous calcification suggest that a lesion is benign, whereas reticular, punctate, amorphous, or eccentric calcifications raise the concern for malignancy. A nodule with a low probability of being malignant may be followed with serial chest CT scans. A nodule that is ≥1 cm and has an intermediate probability of being malignant should be evaluated by fluoro-2-deoxyglucose-PET. If the nodule is negative by PET, they too can be followed with serial chest CT scans; if the PET is positive, the nodule should be excised. A nodule that is <1 cm and has an intermediate probability of being malignant can be followed by serial chest CT scans. Any nodule that has a high probability of being malignant should be excised. For nodules ≥4 mm, serial CT scans are not required if the patient is at low risk. Patients who are at high risk or have nodules >4 mm should have follow-up chest CT scanning.
Question 25
A 30-year-old man, who has been your patient for several years, presents for his regular checkup. He is known to have dextrocardia. He suffers from recurrent sinusitis and, for years, has had mucopurulent sputum and episodic hemoptysis. He has digital clubbing and bilateral crackles on auscultation of the lungs. With which of the following conditions are this patient’s symptoms most consistent?
a) α1-Antitrypsin deficiency
b) Kartagener syndrome
c) Young syndrome
d) Williams-Campbell syndrome
e) Yellow nail syndrome
View Answer
Answer and Discussion
The answer is b.
Objective: Understand the clinical presentation and etiologies of bronchiectasis.
The pulmonary symptoms and signs are suggestive of bronchiectasis. Kartagener syndrome consists of dextrocardia, sinusitis, and bronchiectasis. Young syndrome is defined
as obstructive azoospermia; approximately 20% to 30% of patients have bronchiectasis. Early panacinar emphysema, as well as bronchiectasis, may develop in patients with α1-antitrypsin deficiency. Yellow nail syndrome is characterized by the triad of lymphedema, pleural effusion, and yellow discoloration of the nails; 40% of patients have bronchiectasis. Patients with Williams-Campbell syndrome have a deficiency of the bronchial cartilage of medium-size airways, which dilate and can be complicated by bronchiectasis.
as obstructive azoospermia; approximately 20% to 30% of patients have bronchiectasis. Early panacinar emphysema, as well as bronchiectasis, may develop in patients with α1-antitrypsin deficiency. Yellow nail syndrome is characterized by the triad of lymphedema, pleural effusion, and yellow discoloration of the nails; 40% of patients have bronchiectasis. Patients with Williams-Campbell syndrome have a deficiency of the bronchial cartilage of medium-size airways, which dilate and can be complicated by bronchiectasis.
Question 26
Which of the following statements regarding complications of mechanical ventilation in patients with ARDS is false?
a) Barotrauma is often a significant direct cause of death in ARDS patients.
b) Tissue breakdown, excessive tidal volumes, and low airway pressures predispose to barotrauma.
c) Although often accompanied by nonspecific findings, nosocomial pneumonia is an important cause of morbidity and mortality in ARDS patients, with a prevalence of approximately 55%.
d) The combination of a corticosteroid and a neuromuscular blocking agent used for paralysis in these patients can lead to a reversible myopathy.
e) Decreased radiolucency at the lung bases and the presence of the deep sulcus sign on a chest radiography are clues to the diagnosis of pneumothorax.
View Answer
Answer and Discussion
The answer is a.
Objective: Understand the management of ARDS.
ARDS patients who are mechanically ventilated have an intensive care unit course complicated by barotrauma, nosocomial pneumonia, and multiple organ failure. Additional complications include deep vein thromboses, gastrointestinal bleeding, malnutrition, and side effects from sedatives and paralytics. Barotrauma occurs in a minority of ventilated patients (13% in one study), with barotrauma rarely directly causing death. The tissue breakdown seen in ARDS, high airway pressures, and high tidal volumes predisposes to barotrauma. Barotrauma is evidenced by the development of pneumothorax, subcutaneous emphysema, pneumomediastinum, and interstitial emphysema. Increased radiolucency at the lung bases and the presence of the deep sulcus sign on a chest radiograph are clues to barotrauma and pneumothorax. Nosocomial pneumonia is present in 55% of patients with ARDS and is accompanied by nonspecific findings. The combination of a corticosteroid and a neuromuscular blocking agent has been associated with a reversible myopathy that takes several months to resolve.
Question 27
A 70-year-old man with a 10-year history of COPD comes to your outpatient office for routine follow-up. He is a current smoker with a 20 pack-year tobacco history. He has had two COPD exacerbations in the past year requiring hospitalization. His last episode was 1 month prior to this visit. He is currently on Advair 500/50 one puff twice a day and Albuterol aerosols as needed. His laboratory values show WBC count of 6.7/mm3, hematocrit 50%, platelets 350,000 µL, a normal basic metabolic profile, and a normal echocardiogram. Vitals signs were normal with an SaO2 of 92% at rest. SaO2 drops to 89% on walking up two flights of stairs. His forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) is <70% predicted, and his FEV1 is >50% but <80% predicted. All the following are indicated, except
a) Oxygen
b) Advise patient to quit smoking
c) Tiotropium
d) Pneumococcal vaccination
e) Influenza vaccination
View Answer
Answer and Discussion
The answer is a.
Objective: Understand the management of COPD.
Infection is a frequent cause of COPD exacerbation. All patients with stable COPD should be offered pneumococcal vaccine, especially if they are 65 years or older, or with FEV1 <40%. An influenza vaccine should be offered to all patients with COPD annually. All patients should be strongly encouraged to quit smoking because this can minimize exacerbations and retard the rate of FEV1 decline. For all patients with COPD, a short-acting bronchodilator must be used on an as-needed basis and if that is insufficient to control symptoms, a regularly scheduled long-acting inhaled bronchodilator or a long-acting inhaled anticholinergic should be added. Patients who continue to have exacerbations despite being on optimal long-acting inhaled bronchodilators may require inhaled corticosteroids. Indications for continuous long-term oxygen therapy in COPD patients include an arterial partial pressure of oxygen (PaO2) of ≤55 mmHg or arterial oxygen saturation (SaO2) of ≤88%. If patients have cor pulmonale, right heart failure, or hematocrit >55%, oxygen is also warranted. Long-term oxygen therapy improves quality of life and increases survival in these patients.
Question 28
A 50-year-old cirrhotic male patient with a past medical history of smoking, substance abuse, and alcohol abuse presents with acute hemoptysis, wheezing, and fever. His examination shows a cachectic individual with diffuse wheezing and thermal burns on his fingers and thumbs. Chest radiograph show diffuse alveolar infiltrates. Complete blood count shows a WBC count of 14,000/mm3 with eosinophilia. In regard to this patient’s diagnosis, all the following are true, except
a) Expectoration of black sputum is frequently seen
b) He is at an increased risk for pulmonary infections
c) Fresh-frozen plasma is indicated
d) He is at higher risk for acquiring HIV
e) Pneumothorax may be frequently encountered
View Answer




Answer and Discussion
The answer is c.
Objective: Understand the medical manifestations accompanying substance abuse.
Crack lung may occur within 48 hours of smoking of cocaine, which presents as diffuse alveolar infiltrates, eosinophilia, and fever. Patients may present with pleuritic chest pain, dyspnea with even mild exertion, dry or productive cough, wheezing, and hemoptysis. Melanoptysis or expectoration of black sputum is seen from inhalation of black carbonaceous residue from inflammable substances that are typically used to set fire to crack. Finger burns are seen from handling crack pipes. Cocaine users are at an increased risk for pulmonary infections, malnutrition, HIV, and TB. Crack smokers often perform Valsalva maneuver after inhalation or exhale vigorously into each other’s mouths to augment the uptake of the drug, which may lead to the development of pneumothorax, pneumomediastinum, and pneumopericardium.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree