Fig. 18.1
Port configuration. C 12-mm camera port, L1 and L2 5-mm assistant ports, L1 is 12 mm if endoscopic stapler is used, R1, R2, and R3 8-mm working ports for arm 1, 2, and 3
Some variations in port setup will be required depending on the case and patient. The narrower the pelvic inlet, the more medial the robotic ports will need to be placed.
The most commonly used extraction site is a small transverse Pfannenstiel incision. Alternatively the specimen can be removed with an off midline left lower quadrant or ileostomy site incision if there is adequate reach to the right to place an extracorporeal purse string. A transanal extraction can be used for most distal malignancies when a handsewn coloanal anastomosis is planned and the mesocolon and/or tumor are not too bulky to fit through the anal canal.
Operative Steps (Table 18.1)
Table 18.1
Operative steps
Operative steps | Degree of technical difficulty (scale 1–10) |
|---|---|
1. Exploratory laparoscopy | 1 |
2. Identification of the ureter and ligation of the inferior mesenteric artery and vein | 5 |
3. Mobilization of the sigmoid colon | 3 |
4. Mobilization of the descending colon and splenic flexure | 5 |
5. Rectal mobilization | 5 |
6. Transection of the rectum | 3 |
7. Anastomosis with leak test | 2 |
During a hybrid approach to a robotic-assisted low anterior resection, steps 1–4 are performed in a laparoscopic fashion and are essentially the same as in a laparoscopic sigmoid resection. The various approaches to these steps have been described in a previous chapter, and we will briefly review the steps again.
Exploratory Laparoscopy
Both surgeon and assistant stand on the right side of the patient. It may be necessary to have the anesthesia team move away from the patient’s head or move the patient table caudally to allow for two people to work side by side on the patient’s right. The peritoneum is first examined for any evidence of metastatic disease. The patient is placed in Trendelenburg position with the left side elevated to promote displacement of small bowel out of the pelvis. Atraumatic bowel graspers are used to avoid bowel injury during mobilization.
Identification of the Ureter and Ligation of the Inferior Mesenteric Vessels
The R1, L1, and L2 ports are used during this portion of the operation. A medial to lateral mobilization of the sigmoid colon starts lateral to the ligament of Treitz. The inferior mesenteric vein (IMV) is identified and gently retracted anteriorly. The peritoneum posterior to the IMV is opened using monopolar cautery or scissors, and blunt dissection is used to elevate the IMV and mesocolon off of the retroperitoneum. After the IMV is dissected from its attachments to the left mesocolon, the vessel is clipped and divided with a vessel sealer device or vascular stapler (see Fig. 18.2).
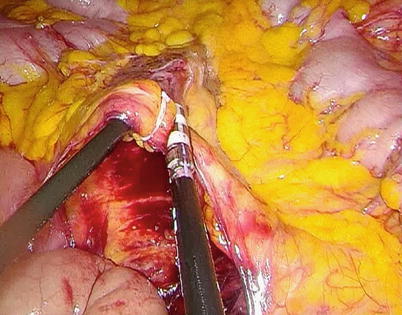
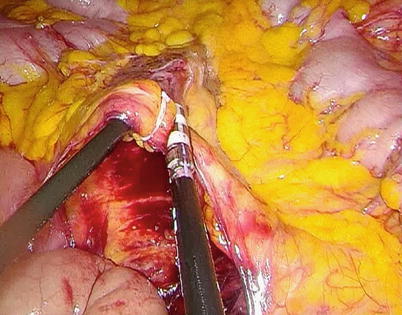
Fig. 18.2
Inferior mesenteric vein clipped and divided
The sigmoid colon is then retracted anteriorly, and the parietal peritoneum is incised medial to the right common iliac artery at the sacral promontory. A combination of sharp and blunt dissection is used to enter this avascular plane and isolate the superior hemorrhoidal artery and the pedicle of the inferior mesenteric artery (IMA). Care is taken to avoid injury to the hypogastric nerve plexus and the left ureter (see Fig. 18.3). These structures are swept posteriorly. The IMA is dissected out until the junction of the left colic artery and superior hemorrhoidal artery can be visualized in a “T”-shaped configuration (see Fig. 18.4). The IMA is then divided at its origin with a vessel sealer device or vascular stapler. The left ureter should be reidentified just prior to transection of the vessel. In most patients, the left colic artery is also divided in this location to allow for greater left colon mobilization into the pelvis. The medial to lateral mobilization of the left colon mesentery is completed to the left abdominal wall.
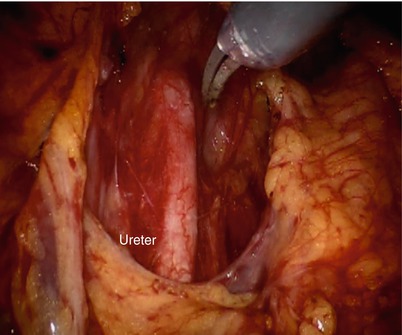
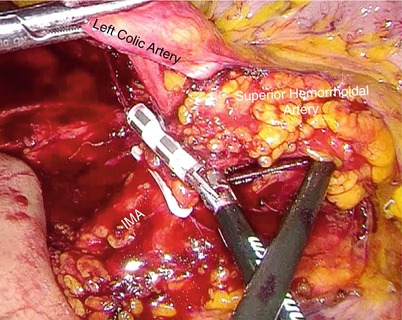
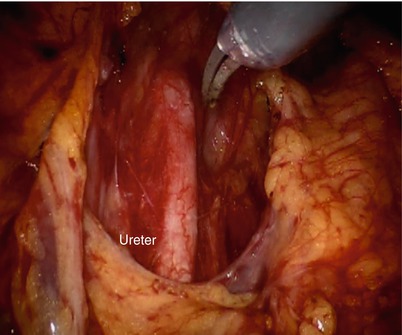
Fig. 18.3
Care should be taken to avoid injury to the ureter
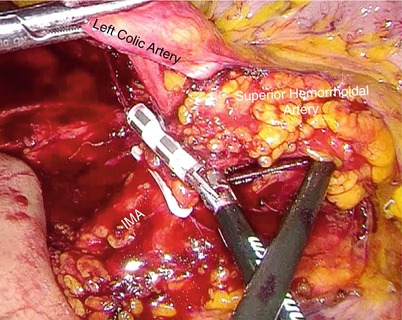
Fig. 18.4
View of the “T formation” created by the inferior mesenteric artery, left colic artery, and superior hemorrhoidal artery
There are some instances when access to the base of the mesentery can be difficult, such as an obese patient or a small patient with minimal intra-abdominal domain or distended small bowel. This can limit the medial-to-lateral approach or make it impossible to safely accomplish. In these cases, a lateral-to-medial approach should be considered.
Mobilization of the Sigmoid Colon
After the medial dissection is complete, lateral dissection is begun at the sacral promontory. The assistant surgeon retracts the colon medially, and the lateral peritoneal reflection is dissected at the line of Toldt (see Fig. 18.5).
Fig. 18.5
Dissection beginning at the line of Toldt
Mobilization of the Descending Colon and Splenic Flexure
The plane between the colonic mesentery and the retroperitoneum is entered medially. The dissection should run along the inferior border of the pancreas, toward the left upper quadrant in the direction of the splenic hilum. Lateral dissection is continued cephalad by division of the phrenocolic and splenocolic ligaments (see Fig. 18.6). The lesser sac is entered (see Fig. 18.7), and the dissection is carried to the base of the mesentery. Care is taken to avoid injury to the tail of the pancreas.
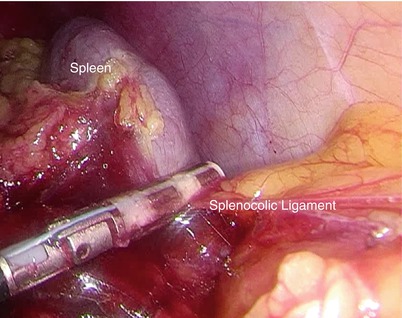
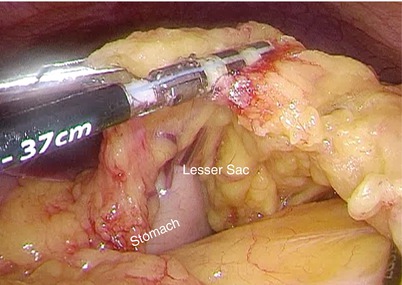
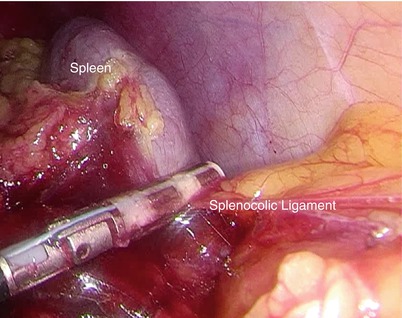
Fig. 18.6
Takedown of the splenocolic ligament at the splenic flexure
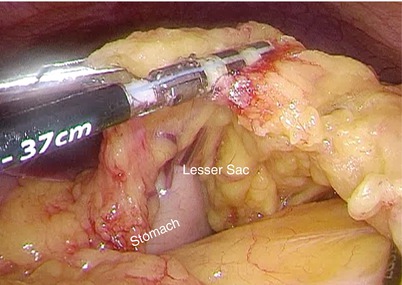
Fig. 18.7
Entry into the lesser sac
Rectal Mobilization
A four-arm da Vinci robot is docked at the patient’s left hip. This setup allows access to the anus to perform intraoperative digital or endoscopic examinations as well as transanal extraction of the specimen. A 0-degree robotic camera is placed in C. Arm 1 is docked in R1 using a “trocar-in-trocar” technique and will carry a hook cautery or monopolar scissors. Arm 2 is docked in R2 with a bipolar fenestrated grasper. Arm 3 is docked in R3 with a Prograsp™, Cadiere™ forceps, or robotic suction irrigator. The assistant surgeon continues standing on the right side of the patient, while the surgeon moves to the console. The assistant will use L1 and L2 to assist in retraction as well as suction/irrigation. An extended-length (rather than standard length) suction irrigator is usually necessary.
The robotic total mesorectal excision (TME) is begun at the sacral promontory below the superior hemorrhoidal artery. Arms 1 (right hand of the surgeon) and 2 (left hand of the surgeon) are used to develop a plane of dissection within the avascular presacral space, while Arm 3 provides retraction (see Video 18.1). It is important to be careful grasping the mesorectum with Arm 2, as the strong robotic arm may tear the tissue and cause bleeding (Box 18.1). Monopolar scissors are preferred to advance the plane of dissection with minimal use of electrocautery (see Fig. 18.8). The hypogastric nerves and both ureters are identified. It is important to perform the dissection in the posterior mesorectal space and not the presacral space. Entering the presacral space will result in injury to the hypogastric nerves and presacral venous bleeding. After entering the plane between the presacral fascia and mesorectum, the dissection is started posteriorly. The sigmoid is retracted anteriorly, and Waldeyer’s fascia (rectosacral fascia) is entered distally at approximately the level of S3. The dissection is advanced caudally to the level of the levator muscles. It is then carried circumferentially within the lateral and anterior planes (see Video 18.2). The hypogastric nerves are identified laterally and preserved along the pelvic sidewall, performing complete autonomic nerve preservation (see Fig. 18.9). Anteriorly, dissection is achieved by incising the peritoneum between the rectum and vagina in women or the seminal vesicles and prostate in men (Box 18.2). In the case of large anterior tumors, the Denonvilliers’ (rectovesical) fascia is resected en bloc with the rectum (see Video 18.3). Arm 3 is the ideal anterior retractor during this part of the operation. The lateral stalks are divided close to the rectum to avoid nerve injury (see Video 18.4).
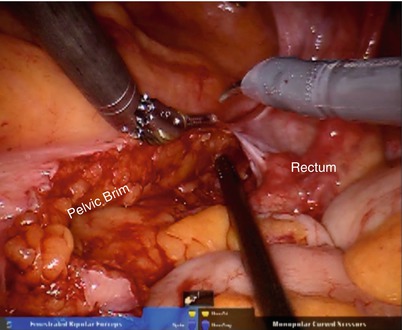
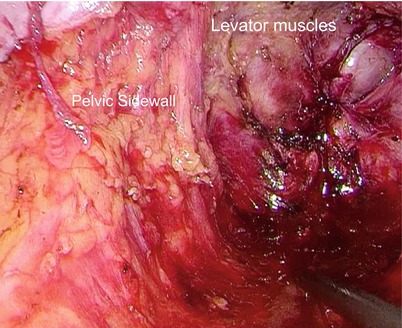
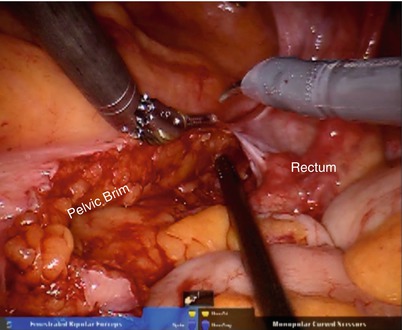
Fig. 18.8
The sharp dissection should be performed using endoshears
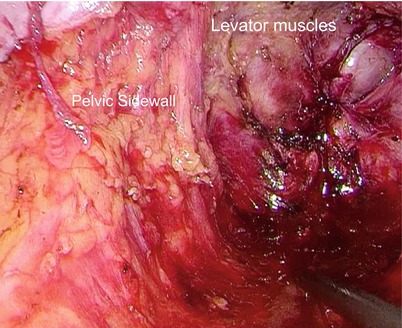
Fig. 18.9
A view of the pelvic sidewall and levator muscles after total mesorectal excision
Box 18.1 Tip
Avoid grasping the mesorectum and/or mesentery to prevent bleeding and subsequently obscuring the surgical field and the exact TME plane of dissection. Grasp the rectal wall, appendages, or peritoneum instead, and meticulously control any miniscule bleeding immediately.









