ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Progressive inflammatory, sclerosing, and obliterative disease of the extrahepatic or intrahepatic bile ducts, or both.
Disproportionate elevation of serum alkaline phosphatase (4–10 times normal) is seen in almost all patients.
Magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP) shows multifocal stricturing of the intrahepatic and extrahepatic bile ducts.
Small duct disease is diagnosed by liver biopsy.
Liver biopsy findings that are highly specific include fibrous obliteration of small bile ducts with concentric replacement by connective tissue in an “onion skin” pattern.
Patients have an 8–15% lifetime risk of developing cholangiocarcinoma, and it is often difficult to distinguish a dominant stricture from a cholangiocarcinoma.
GENERAL CONSIDERATIONS
Primary sclerosing cholangitis (PSC) is a disorder of unknown etiology that is characterized by a progressive, inflammatory, sclerosing, and obliterative process affecting medium-sized and large extrahepatic or intrahepatic bile ducts, or both. A vast majority of patients (prevalence rates range from 70% to 90%) have underling inflammatory bowel disease, especially ulcerative colitis. PSC has also been associated (although rarely) with multifocal fibrosclerosis syndromes such as retroperitoneal, mediastinal, and periureteral fibrosis. In retrospect, it appears that some of these latter cases actually represented patients with autoimmune pancreatitis and bile duct strictures masquerading as PSC.
The median survival of patients with PSC from time of diagnosis to death in several series has ranged from 9 to 12 years. Late in the course of the disease, complete biliary obstruction, secondary biliary cirrhosis, portal hypertension with bleeding varices, liver failure, and development of cholangiocarcinoma may occur.
[PubMed: 17414848]
CLINICAL FINDINGS
Patients with PSC are often asymptomatic at the time of diagnosis. The disorder is often suspected in patients with inflammatory bowel disease who have a persistent and other-wise unexplained abnormal elevation in serum alkaline phosphatase (ie, values at least two times the upper limit of normal), and with abnormal values persisting for longer than 6 months. Asymptomatic patients with persistent elevations of serum alkaline phosphatase are often screened for PSC, and many actually turn out to have the disease.
Symptomatic patients who have PSC often present with signs and symptoms of chronic biliary obstruction, right upper quadrant abdominal pain, pruritus, jaundice, and acute cholangitis. Fatigue and pruritus are common features at presentation.
Liver tests usually demonstrate a cholestatic pattern, with serum alkaline phosphatase disproportionately elevated to levels 4–10 times normal and serum aminotransferase that is usually 300 IU/L or less. Serum albumin and globulin levels are usually normal except in patients with advanced disease. As noted later, in the discussion of differential diagnosis, the presence of positive tests for antinuclear antibodies or smooth muscle antibodies, or both, should raise the suspicion of PSC–autoimmune hepatitis (AIH) overlap syndrome.
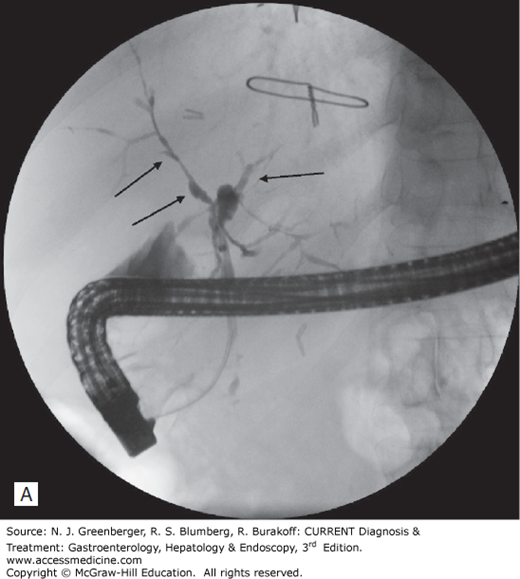
The diagnosis of PSC is usually established by demonstration of the characteristic multifocal stricturing with normal and/or dilated areas of intrahepatic or extrahepatic bile ducts, or both, on cholangiography. The typical appearance reveals narrowing and beading of the bile ducts (Figure 53–1). These abnormalities can be demonstrated by either MRCP or ERCP. MRCP is currently preferred as it is a noninvasive procedure and does not carry the risk of either pancreatitis or cholangitis. The vast majority of patients (~85%) have both intrahepatic and extrahepatic bile duct strictures, approximately 10–15% have intrahepatic bile duct strictures alone, and 2–4% have extrahepatic biliary strictures alone.
It should be emphasized that patients with small duct PSC do not demonstrate cholangiographic abnormalities. In these patients, diagnosis is suspected on the basis of an elevated serum alkaline phosphatase level and established by a liver biopsy in conjunction with other clinical features.
Liver biopsy findings often support the diagnosis of PSC. The most characteristic histologic finding is fibrous obliteration of small bile ducts with concentric replacement by connective tissue in an “onion skin” pattern (Plate 99). More often, histologic abnormalities in PSC are nonspecific and may be similar to those seen in primary biliary cirrhosis.
PSC is frequently staged according to the histopathologic findings. In stage 1 disease, there is enlargement, mononuclear cell infiltration, and scarring in the portal triads. Stage 2 disease is characterized by fibrosis extending into the surrounding parenchyma, stage 3 by bridging fibrosis, and stage 4 by cirrhosis (Figure 53–2).
Figure 53–2.
Imaging findings. A. ERCP demonstrating stricturing and beading of the intrahepatic ducts (arrows denote stricturing). B. MRCP showing stricturing (arrows) of the biliary tree. (Used with permission of Dr. John R. Saltzman, Brigham and Women’s Hospital.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree